
![]()
Anterior Repair and Kelly Plication
Site Specific Posterior Repair
Sacrospinous Ligament Suspension of the Vagina
Excision of Transverse Vaginal Septum
Correction of Double-Barreled Vagina
Incision and Drainage of Pelvic Abscess via the Vaginal Route
Transposition of Island Skin Flap for Repair of Vesicovaginal Fistula
McIndoe Vaginoplasty for Neovagina
Marsupialization of a Suburethral Diverticulum by the Spence Operation
Suburethral Diverticulum via the Double-Breasted Closure Technique
Urethrovaginal Fistula Repair via the Double-Breasted Closure Technique
Goebell-Stoeckel Fascia Lata Sling Operation for Urinary Incontinence
Transection of Goebell-Stoeckel Fascia Strap
Rectovaginal Fistula Repair via Musset-Poitout-Noble Perineotomy
Watkins Interposition Operation
The Watkins interposition operation is for repair of pelvic prolapse. Although it is infrequently used, it is an operation which adds the entire uterus as a supporting structure for the pubovesicle cervical fascia thereby supporting and reinforcing the anatomic fascia of the bladder in a way that will provide greater support and tolerate greater pressure associated with vigorous physical activity.
The operation can be performed under regional or general anesthesia. It should be delayed until childbearing is complete. The surgeon must be confident that there is no intrauterine neoplastic disease.
The purpose of the operation is to support the floor of the bladder, reinforce the pubovesicle cervical fascia, and reduce pelvic prolapse.
Pathophysiologic Changes: By providing greater support to the floor of the bladder and reinforcing the pubovesicle cervical fascia, recurrence of the cystourethrocele and pelvic prolapse should be rare, even in women who perform heavy manual labor.
Points of Caution: Care must be taken to thoroughly sample the endometrium prior to performing the operation to ensure against the presence of intrauterine neoplasia. We recommend surgical sterilization on women having this operation who are in the reproductive age group.
Technique
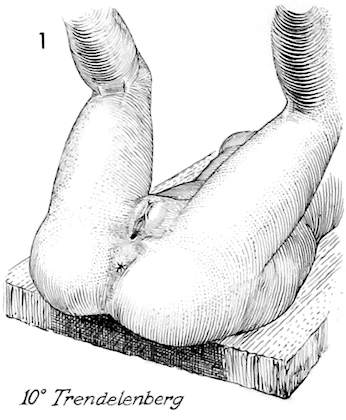
The operation is begun by placing the patient in the dorsal lithotomy position and surgically preparing the epithelium of the vulva, vagina, and perineum. The operating table is placed in approximately 10 degree Trendelenburg position.
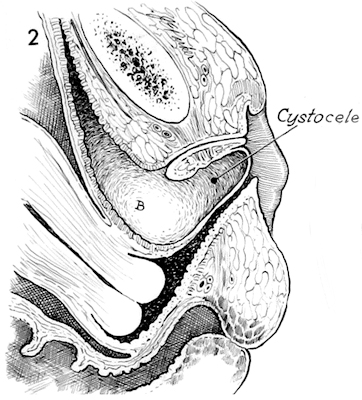
A sagittal section through the pelvis demonstrates the pathologic condition to be corrected, a large cystocele with descensus of the uterus.
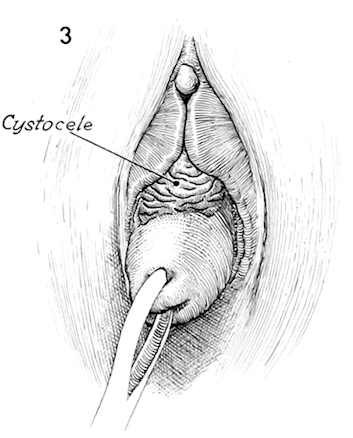
A perineal view showing a cystocele and prolapse of the cervix.
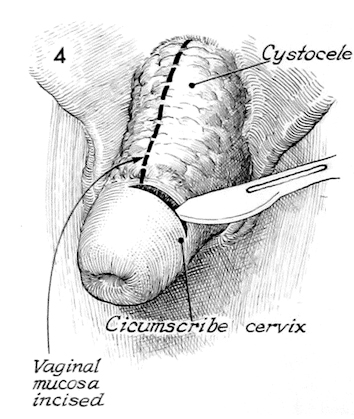
The operation is begun by making a transverse incision at the junction of the vaginal epithelium and the portio of the cervix. This transverse incision is extended until the entire cervix is circumscribed. Posteriorly, the cul-de-sac of Douglas is entered.
Anteriorly, the vaginal mucosa is opened after undermining the anterior vaginal mucosa with a curved Mayo scissors.
Allis clamps retract the anterior vaginal mucosa. The bladder is dissected off the lower uterine segment by blunt and sharp dissection.
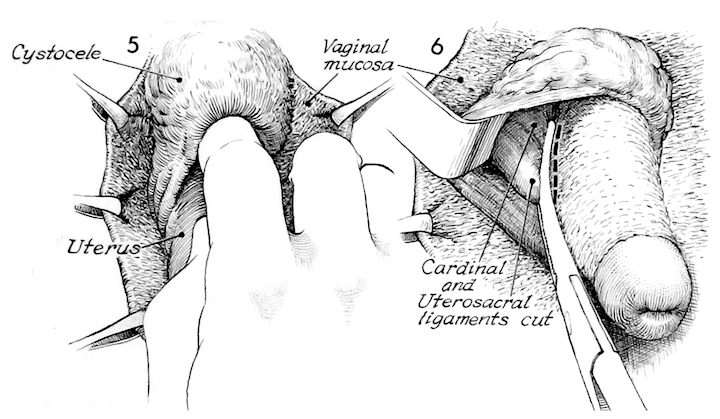
After the bladder is sufficiently mobilized, a right angle retractor is placed under the bladder to keep it out of the surgical field. A Haney clamp is placed across the cardinal and uterosacral ligaments. These ligaments are incised with curved Mayo scissors along the dotted line shown. This pedicle is tied with 1 synthetic absorbable suture.
The same procedure is performed on the opposite side thus preparing the cervix for amputation at the lower uterine segment.
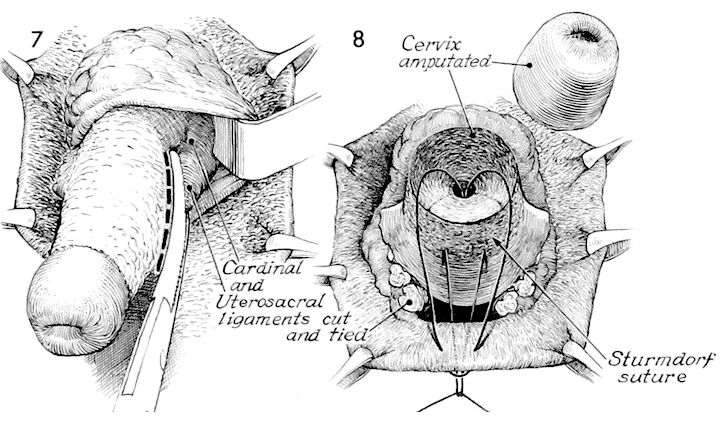
The cervix is amputated. The anterior and a portion of the posterior vaginal mucosa are held with Allis clamps. The pedicles of the uterosacral and cardinal ligaments are seen posteriorly.
The posterior lip of the lower uterine segment is covered with vaginal epithelium by bringing a Sturmdorf suture of 1 synthetic absorbable through the posterior vaginal mucosa and lower uterine segment exiting into the endocervical canal. The suture is passed twice through the margin of the vaginal mucosa. It is passed back through the endocervical canal exiting from the lower uterine segment and then out through the posterior vaginal mucosa adjacent to the initial suture.
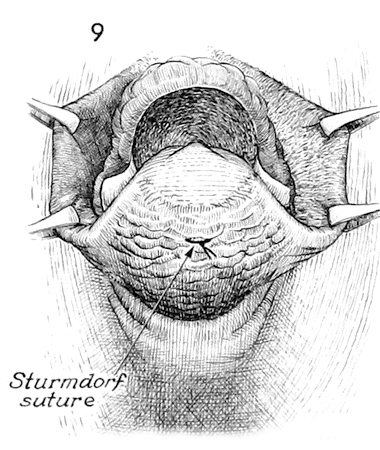
When this suture is tied, the edge of the posterior vaginal mucosa will be pulled up into the endocervical canal at the junction of the lower uterine segment. The entire posterior lip of the lower uterine segment is covered. The edges of the anterior vaginal mucosa are shown held in Allis clamps. The anterior stump of the lower segment is not covered with epithelium at this time.
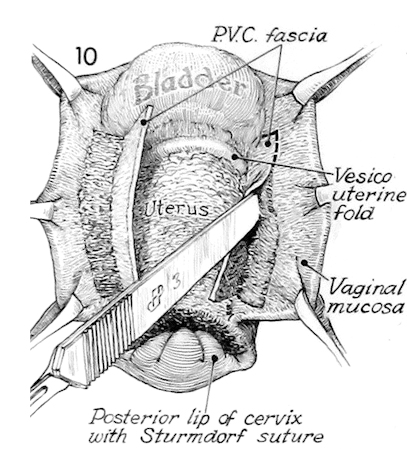
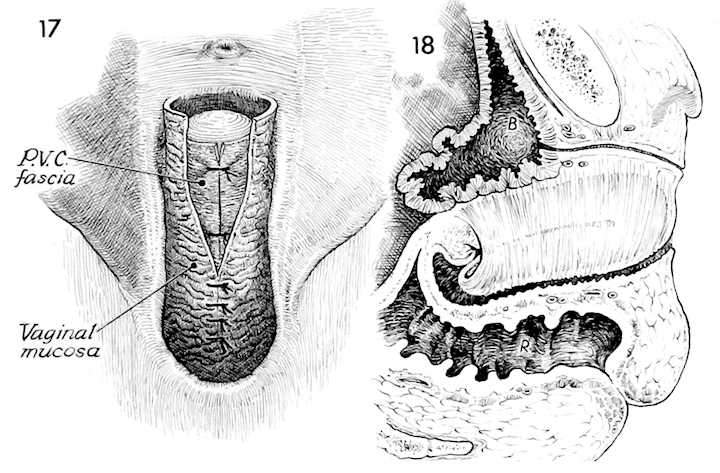
The bladder has been dissected off the uterus revealing the vesicouterine peritoneal fold. The pubovesicle cervical fascia is dissected off of the anterior vaginal mucosa. This is performed in the same manner as if one were performing an anterior repair. This dissection can be started with a scalpel and completed with blunt dissection or scissors. The pubovesicle cervical fascia should be sufficiently mobilized so that it will close over the entire uterus which will be interposed between the bladder and vaginal mucosa. The posterior lip of the cervix is shown covered with vaginal mucosa from the previously placed Sturmdorf suture.
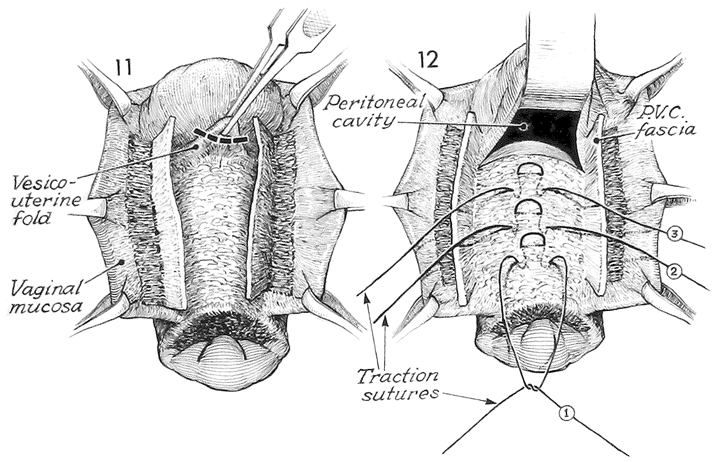
The vesicouterine fold is elevated with thumb forceps and opened.
The opening into the peritoneal cavity can be confirmed by exploring the anterior cul-de-sac with a finger. A right angle retractor is placed under the bladder. The pubovesicle cervical fascia has been mobilized.
At this point 5 number 1synthetic absorbable mattress sutures, numbered 1, 2, 3, etc. are placed in the body of the uterus and held on hemostats without tying.
These number 1 synthetic absorbabe sutures placed in the body of the uterus are also used for traction to bring it progressively forward until the fundus is seen emerging through the anterior cul-de-sac. The bladder is held with a right angle retractor. The last 1 synthetic absorbable suture is placed in the fundus. Note the position of the pubovesicle cervical fascia in this drawing. The anterior vaginal mucosa is held with Allis clamps.
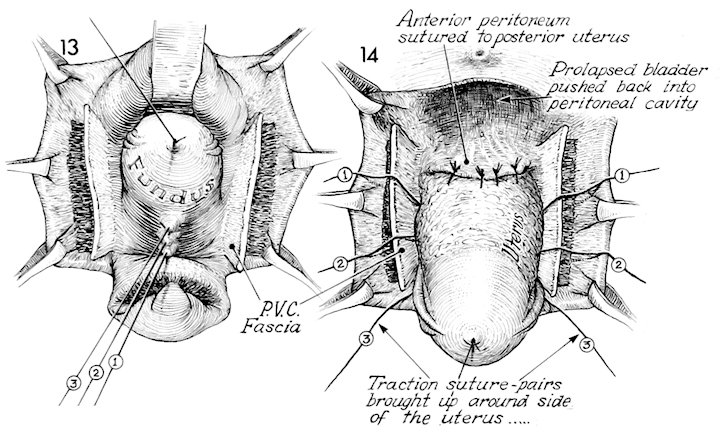
The traction sutures have been used to pull the fundus through the anterior cul-de-sac. In this drawing the posterior wall of the uterus is shown. Reperitonealization of the pelvic floor is performed by suturing the vesicle peritoneum to the posterior wall of the uterus with 3 or 4 interrupted 2/0 synthetic absorbabe sutures. To achieve this, the prolapsed bladder has to be pushed back into the peritoneal cavity with the right angle retractor until the peritoneum can be seen. Note in this drawing the previously placed 1 synthetic absorbable sutures in the anterior wall of the uterus held on traction with hemostats are marked 1, 2, 3.
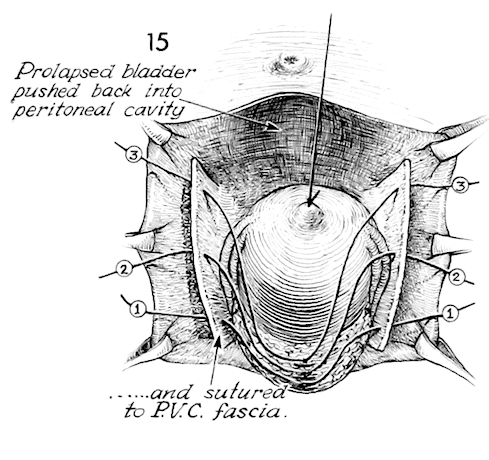
The traction suture in the fundus is now brought cephalad reversing the axis of the uterus. The anterior uterine wall and the previously placed traction sutures 1, 2, and 3 are seen. In a progressive manner each of these 1 synthetic absorbable traction sutures in the anterior uterine wall is threaded upon a small curved Mayo needle and passed through the pubovesicle cervical fascia as shown in the drawing.
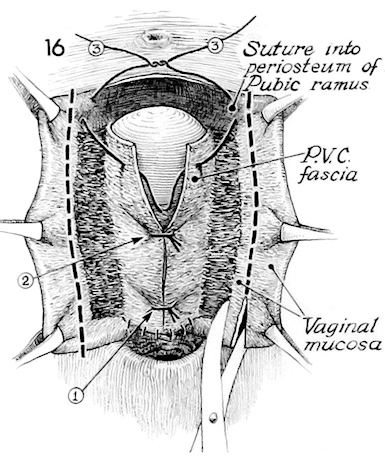
The sutures passed from the anterior uterine wall through the pubovesicle cervical fascia are progressivey tied thus bringing the pubovesicle cervical fascia over the anterior surface of the uterus. Note suture #3; it is placed through the pubovesicle cervical fascia and through the periosteum of the pubic ramus.
Excess vaginal mucosa is trimmed away. Note the interrupted sutures placed between the inferior margin of the vaginal mucosa and the anterior stump of the lower uterine segment re-epithelializing the anterior lip with anterior vaginal mucosa.
The pubosvesicle cervical fascia can be seen beneath the closure of the anterior vaginal mucosa. This closure is carried to the top of the incision near the urethral meatus.
A sagittal section through the pelvis shows the interposition of the uterus between the vaginal mucosa and the floor of the bladder and urethra thus reinforcing the pubovesicle cervical fascia. The uterus has been used as a prosthesis over deficient fascia in a hernia repair.
Note that the endometrial cavity is open for drainage of either blood or mucus. Entry into the endometrial cavity, while difficult, can be made.
A Foley catheter is left in the bladder for several days; no packing is left in the vagina.