
![]()
Anterior Repair and Kelly Plication
Site Specific Posterior Repair
Sacrospinous Ligament Suspension of the Vagina
Excision of Transverse Vaginal Septum
Correction of Double-Barreled Vagina
Incision and Drainage of Pelvic Abscess via the Vaginal Route
Transposition of Island Skin Flap for Repair of Vesicovaginal Fistula
McIndoe Vaginoplasty for Neovagina
Marsupialization of a Suburethral Diverticulum by the Spence Operation
Suburethral Diverticulum via the Double-Breasted Closure Technique
Urethrovaginal Fistula Repair via the Double-Breasted Closure Technique
Goebell-Stoeckel Fascia Lata Sling Operation for Urinary Incontinence
Transection of Goebell-Stoeckel Fascia Strap
Rectovaginal Fistula Repair via Musset-Poitout-Noble Perineotomy
Site Specific Posterior Repair
A posterior repair is generally performed in conjunction with a perineorrhaphy to correct a rectocele and to reconstruct the perineal body. A rectocele is a hernia which develops when the rectovaginal fascia is insufficient to support the anterior rectal wall and the rectum prolapses through the levator sling. The strength of the posterior vaginal mucosa is insufficient to prevent prolapse of the anterior rectal wall.
The purpose of the site specific posterior repair is to reattach the torn rectovaginal fascia to its orginial position.
Physiological Changes: The anterior rectal wall is reduced to its normal anatomic position and is prevented from prolapsing into the vagina. In severe cases, this prolapse can be of such magnitude that defecation becomes incomplete and difficult.
Points of Caution: The new technique of site specific posterior repair re-establishes the rectovaginal fascia and no longer plicates the levator ani in the midline as was demonstrated in previous editions of this atlas. The surgeon must be careful not to enter the rectum during the dissection.
Technique

Figure 1 shows a cross section of the pelvis with the patient in a dorsal lithotomy position. The rectocele is demonstrated.
A bimanual examination under anesthesia is performed to differentiate between an enterocele and a rectocele. Observation of the perineal body is made to determine the extent of reconstruction needed.

Figure 2 shows a vaginal view of the rectocele protruding out of the vagina. The labia are retracted with interrupted sutures if needed. Allis clamps are applied to the posterior vaginal mucosa at the upper extent of the rectocele.

The operation is begun by making a transverse incision at the hymenal ring. The length of this incision is determined by the degree of tightening required at the forchette. It is sometimes helpful to grasp the apices of this incision with Allis clamps and pull them together to be able to judge the ultimate caliber of the introitus at the end of the repair and adjust accordingly. An additional Allis clamp is placed in the midline at the top of the rectocele. In large rectoceles, a series of midline clamps may be necessary to provide traction for dissection and to keep the operator's incision in the midline.
A Kelly clamp or Metzenbaum scissors is inserted under the posterior vaginal mucosa, dissecting the posterior mucosa off the rectovaginal fascia. By opening the jaws of the instrument, dissection occurs and blood vessels are pushed aside. A midline incision is then made in the mucosa. This process is repeated until the superior apex of the rectocele is reached.
An additional incision is made in the perineal body, removing a triangular section of perineal skin which is outlined by the dotted line. This will expose the aponeurosis of the bulbocavernosus muscle. Care should be taken to only remove the skin.
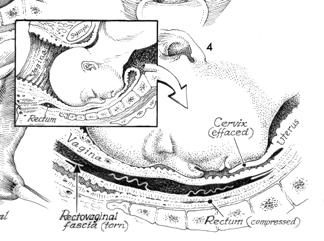
The inset shows the obstetrical etiology of the rectocele as the fetal head is coming through the pelvis, the rectovaginal fascia can be torn in several places. One can see the rectovaginal fascia torn and the rectum compressed against the sacrum.
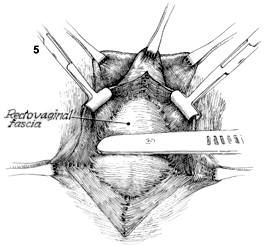
The vertical incision in the posterior vaginal mucosa has been made, and the edges are held with Allis clamps. The rectovaginal fascia is dissected off the posterior vaginal mucosa. The apex of the rectocele is held in an Allis clamp. The dissection of the rectovaginal fascia off the vaginal mucosa is started with a scalpel but completed with a Metzenbaum scissors or open sponge. It is helpful to place your index finger behind the vaginal mucosa as you dissect to prevent "button-holing" of the vaginal mucosa.
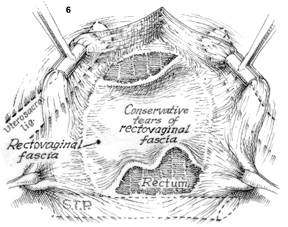
With exposure one can find the torn edges of the rectovaginal fascia. The most common cause of a rectocele is the transverse tear of the rectovaginal fascia off the superficial transverse perinei muscle. Tears off the uterosacral ligaments and peri-cervical ring are seen with enteroceles. The edges of the fascia can be grasped with Allis clamps and brought down into position. One should notice that the superficial transverse perinei muscle is shown intact. It must be reapproximated if it is also torn. One can visualize the rectum through one of the tears in the rectovaginal fascia inferiorly.
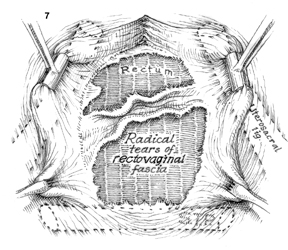
Figure 7 demonstrates an extreme tearing of the rectovaginal fascia. A simple suture repair is not adequate for this severe degree of tearing, and this patient is a good candidate for a graft.
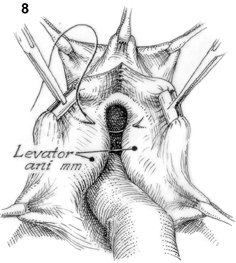 Plicating the levator ani in the midline over the rectum as was previously described in traditional descriptions is an example of what not to do during a posterior repair procedure. Plication of the levator ani muscles increases postoperative pain and risk for de novo dyspareunia.
Plicating the levator ani in the midline over the rectum as was previously described in traditional descriptions is an example of what not to do during a posterior repair procedure. Plication of the levator ani muscles increases postoperative pain and risk for de novo dyspareunia.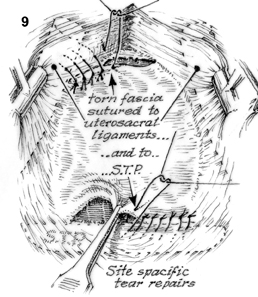
The rectovaginal fascia is identified and reapproximated to the uterosacral ligaments at the top of the vagina and sutured inferiorly to the superficial transverse perinei muscle.
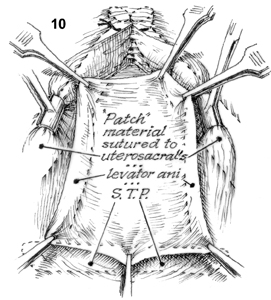
When the rectovaginal fascia is severely torn or almost nonexistent, an autologous graft of fascia lata or rectus fascia is sutured to the uterosacral ligaments, the rectovaginal fascia overlying the levator ani, and the perinei muscle creating a new "rectovaginal fascia."

The vagina is then closed over this repair leaving the tail of the suture marked "a" a rather long piece of the suture. Note the denuded aponeurosis of the bulbocavernosus in the midline. It is necessary to reapproximate it with interrupted sutures if it is not intact. Do not trim or over trim the vaginal mucosa before closing as this may lead to narrowing of vaginal tube and dyspareunia.
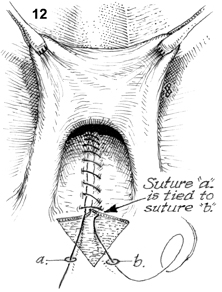
The suture line in the posterior vaginal wall is brought down to the hymeneal ring. Suture "a" is attached to the top of the vagina. Suture "b" is at the hymeneal ring. Suture "a" is tied to suture "b" and suture "a" is trimmed.
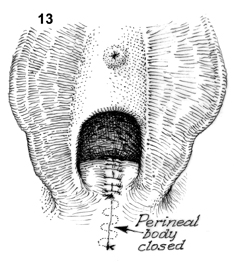
The perineal body is repaired by a subcuticular stitch with suture "b" from the hymeneal ring down to the anus.
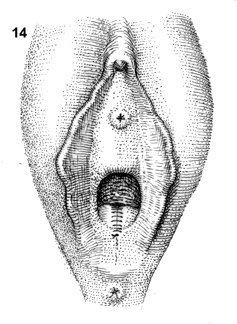
The complete repair is shown. A vaginal exam should be performed to assure adequate width of the vagina remains, and a rectal exam should be performed to ensure there are no sutures in the rectum.
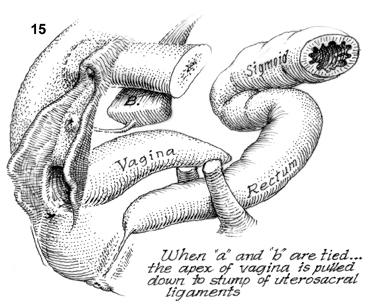
When sutures "a" and "b" from figure 12 are tied, the apex of the vagina is pulled down to the stumps of the uterosacral ligaments leaving a more normal anatomical position of the vagina by pulling it posteriorly.