Abdominal
Wall
Pfannenstiel Incision
Maylard Incision
Panniculectomy
Incisional Hernia
Repair
Abdominal
Wound
Dehiscence and
Evisceration
Massive
Closure
of the Abdominal
Wall With a One-Knot
Loop Suture
Hemorrhage
Control Following Laceration
of Inferior Upper
Epigastric Vessels |
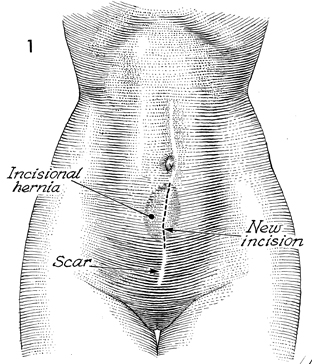
Incisional Hernia Repair
Although improved suture materials (stainless steel wire, monofilament
nylon, Prolene, etc.), in addition to improved techniques in closing
the rectus fascia, have significantly reduced the incidence of incisional
hernia, such hernias do occasionally occur.
They are, interestingly, rarely seen with the lower transverse Pfannenstiel-type
incision. The etiology of incisional hernia can range from wound infection
and subfascial hematoma to a disruption of the suture line secondary
to coughing during the immediate postoperative period.
The purpose of the operation is to close the hernia and reinforce the
fascia to reduce recurrence.
Physiologic Changes. The overall comfort of a patient
is increased by eliminating the incisional hernia. Although the incidence
of bowel obstruction is small, it can occur. The traditional physiologic
principles of hernia repair apply equally to incisional hernias and
inguinal hernias (i.e., high ligation and excision of the hernial sac
and double reinforcement of the rectus fascia).
Points of Caution. Care must be exercised in making
the initial incision to avoid lacerating a loop of bowel adherent in
the hernial sac.
Adequate mobilization of both fascia and subcutaneous tissue should
be made to allow tissues to come together without tension.
Technique
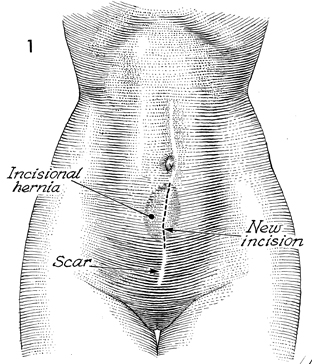
The patient is placed on the operating table
in a supine position. Palpation of the abdomen reveals the hernia.
No attempt is made to excise the cutaneous portion of the hernial
sac. A midline incision is made over the hernial area, excising
the previous scar. |
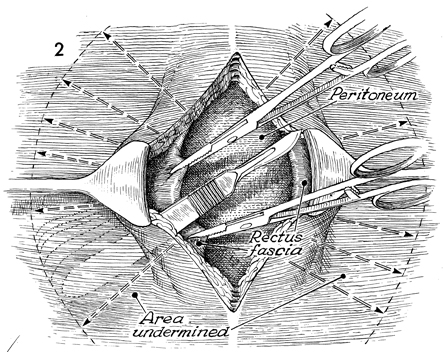
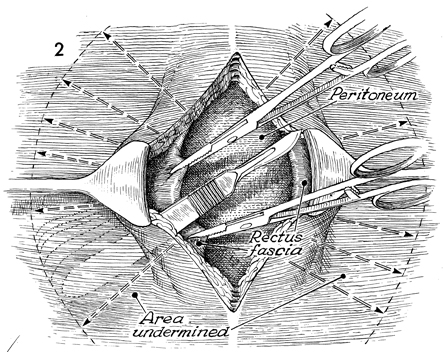
The incision is carried down to the hernial
sac, which generally represents the peritoneum or attenuated
rectus fascia. The hernial sac is located, a small hole is made,
the sac is completely explored with the finger, the peritoneal
incision is extended, and all contents are removed from the sac.
The margins of the sac itself are identified and excised with
scissors. The margins of the rectus fascia are then identified,
and the skin and subcutaneous fat overlying the rectus fascia
are sufficiently mobilized to allow the rectus fascia to be developed
as two overlying flaps similar to a double-breasted coat. This
is initiated by placing a retractor under the skin margin, applying
two Kocher clamps to the margin of the rectus fascia, and dissecting
the skin and subcutaneous tissue from the rectus fascia with
sharp dissection. The same procedure is carried out on the opposite
side. The peritoneum is closed with a running 0 synthetic absorbable
suture. |
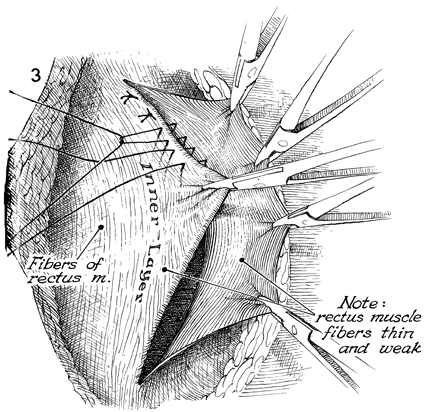
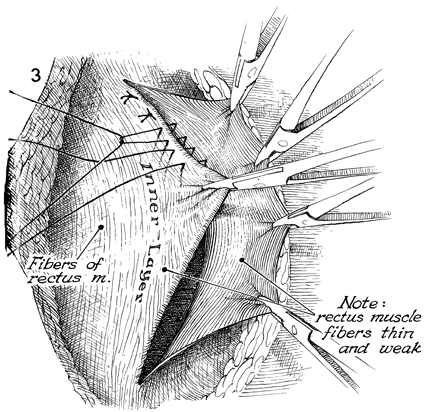
A row of 28-gauge stainless steel wire or
0 nylon sutures is placed in the base of one flap and through
the margin of the opposite flap as interrupted mattress sutures.
These are tied in progression. The margin of the overlying flap
is elevated by traction with small hemostats. |
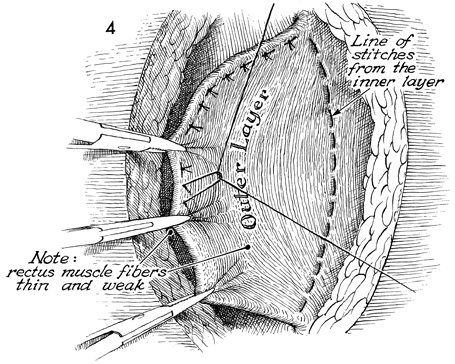
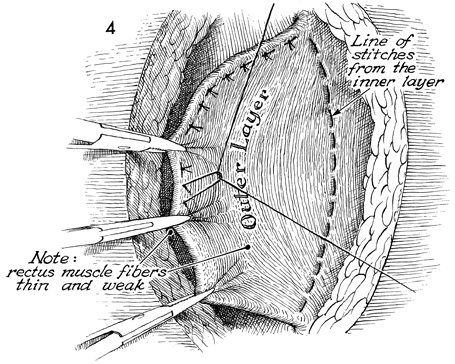
The line of sutures from the
inner flap is completed. The outer layer of rectus fascia is
pulled over the inner layer and sutured with interrupted 28-gauge
wire or 0 nylon mattress sutures. |
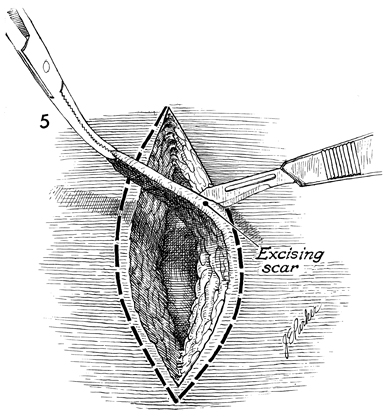
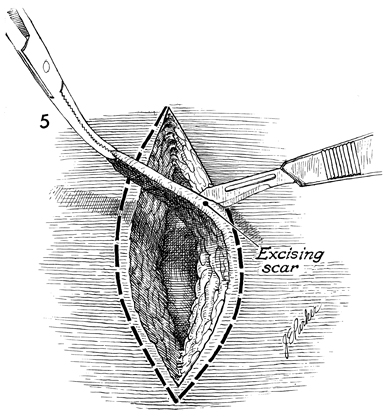
Any existing scar tissue in the skin and
subcutaneous incision is surgically excised. |
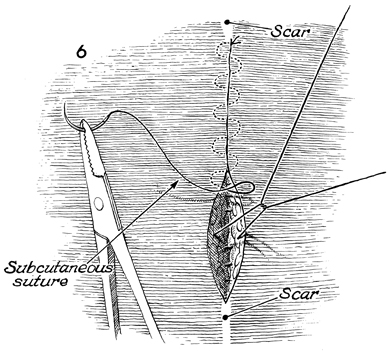
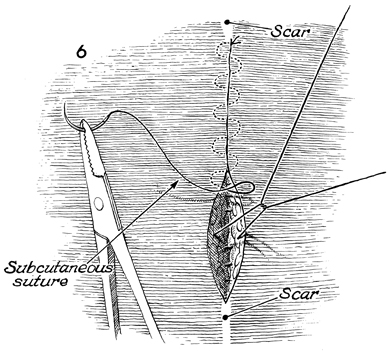
The subcutaneous tissue is
closed with interrupted 2-0 synthetic absorbable suture, and
the skin is closed with a subcutaneous 3-0 Dexon suture. |
|