|
||||||||||
Appendectomy
Using End Sigmoid Colostomy With Hartmann's Pouch Anterior
Resection Low
Anastomosis Anterior
Resection |
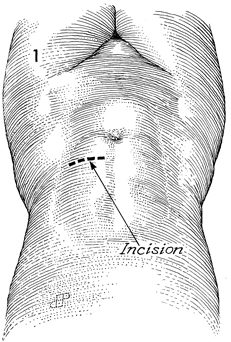
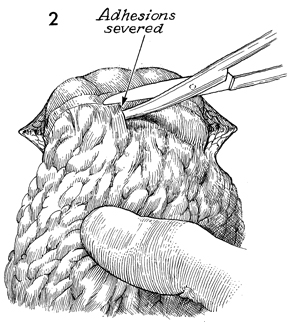
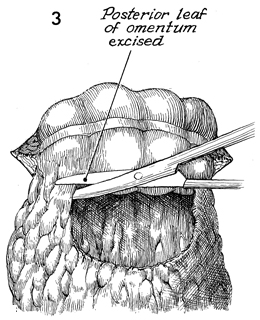
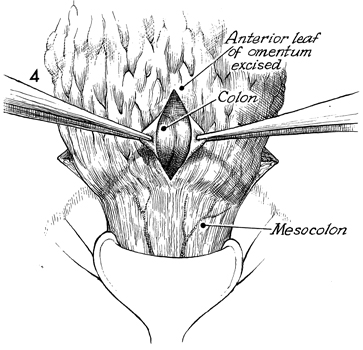
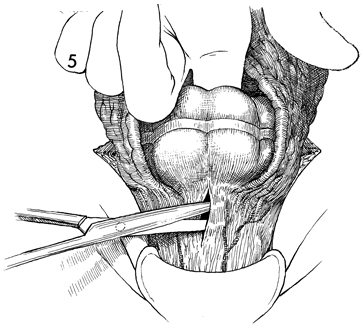
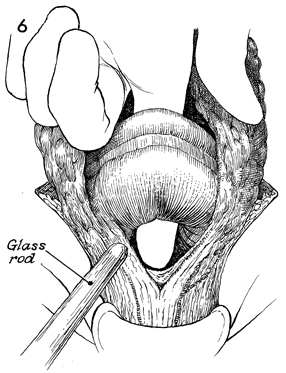
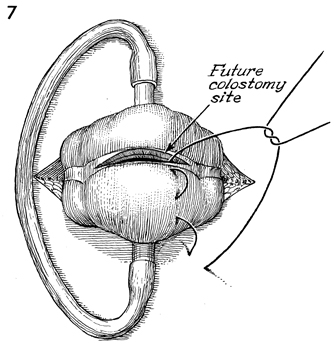
Transverse Loop Colostomy Transverse loop colostomy is a simple, fast, and relatively easy procedure used for those patients with pelvic disease in whom a temporary fecal diversion is needed and who are not candidates for an end sigmoid colostomy because of medical or technical reasons. In general, transverse colostomies related to gynecologic malignancies should be performed on the left rather than the right transverse colon. A left transverse colostomy has the advantage of additional length of colon for fecal fluid absorption and allows the right transverse colon to remain available for small bowel bypass if needed in the future. The purpose of the transverse loop colostomy is to divert the fecal stream. Physiologic Changes. The fecal stream is diverted. Stool from the transverse colostomy will contain a larger volume of water than stool from a sigmoid colostomy. Therefore, a transverse colostomy may be more difficult to regulate. Points of Caution. The incision for the colostomy should be well designed. The site for the stoma should be marked the night before surgery while the patient is in the standing position so that the stoma for the colostomy is not on the underside of the abdominal panniculus. The stoma site should be selected so as not to interfere with the waistline of clothing. The incision should be long enough to ensure adequate exposure of the bowel. The three anatomic characteristics of the colon should be identified prior to performing the operation: the teniae coli, haustral markings, and the colonic relationship to the omentum. Closure of the abdominal wall around the colostomy should be tight enough to prevent hernia but should allow enough space to prevent strangulation and ischemia of the colonic loop. Technique
|
|||||||||
Copyright - all rights reserved / Clifford R. Wheeless,
Jr., M.D. and Marcella L. Roenneburg, M.D.
All contents of this web site are copywrite protected.