Colon
Appendectomy
Appendectomy
Using
the Linear Dissecting
Stapler
Transverse
Loop
Colostomy
End
Sigmoid Colostomy With Hartmann's Pouch
Closure
of a Loop
Colostomy
Anterior
Resection
of the Colon With Low
Anastomosis Using
the Gambee Suture
Technique
Low
Anastomosis
of Colon to Rectum
Using the End-to-End
Surgical Stapler
Technique
Anterior
Resection
of the Colon With
Low Anastomosis via
the Strasbourg-Baker
Technique |
Low Anastomosis of Colon
to Rectum Using the End-to-End
Surgical Stapler Technique
There are two techniques for low anastomosis of colon
to rectum: the suture technique and the EEA (end-to-end anastomosis)
stapler technique.
The EEA stapler technique has allowed very low anastomoses
to be performed that were previously thought to be extremely difficult
with suture. Suture anastomoses below 7 cm have been associated with
a high incidence of anastomotic leaks. The stapler technique offers
a clean, vascular, and safe method for very low anastomoses of colon
to rectum with a resultant fecal incontinence rate of less than 5%
and anastomotic leak rate of less than 7%.
In gynecologic oncology,
it is wise to protect these very low anastomoses with a proximal colostomy
if the patient (1) has previously been irradiated, (2) has significant
diverticular disease, or (3) has had no bowel preparation.
The purpose
of the operation is to establish continuity of the colon and rectum.
Physiologic Changes. The low anastomosis preformed
with the EEA surgical stapler has a superior blood supply. It is associated
with less tissue trauma and has a lower incidence of leaks from the
anastomosis. Therefore, we feel it is a superior anastomosis, particularly
in scarred ischemic bowel following irradiation therapy to the pelvis.
Points of Caution. Adequate mobilization
of the descending colon must be made. Frequently, the splenocolic ligament
must be transected and the transverse colon must be adequately mobilized
to ensure that there is no tension on the anastomosis. If complete
mobilization requires sacrificing the inferior mesenteric artery, extreme
care must be taken to ensure that the blood supply from the middle
colic artery is intact along with the marginal artery of the colon.
Care
must be taken in placing the pursestring sutures. They should not be
placed more 0.5 cm from the margin of the bowel. Otherwise, too much
tissue will be gathered into the anvil and jam the stapling mechanism
of the EEA stapler. This will result in a defective anastomosis. The
size of the EEA stapler must be carefully selected to conform with
the diameter or the colon and rectum. Forcing a stapler that is too
large will only split the colon and result in ischemia and necrosis.
After the EEA stapler has been fired and before the
stapler is removed, it may be efficacious to place interrupted Lembert
sutures with synthetic absorbable material north, south, and west around
the stapled bowel to relieve tension on the staple suture line and
improve wound healing.
The last step in the operation involves three
tests: inspection of the anastomosis, observation of the "O" rings
from the stapler, and the "bubble test." The last of these, the so-called
"bubble test," is of maximum importance. Most anastomotic leaks can
be diagnosed at the time of surgery, and therefore, the surgeon should
not wait until the fifth to seventh postoperative day to learn that
the anastomosis is leaking.
Technique
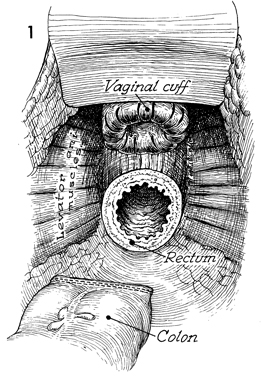
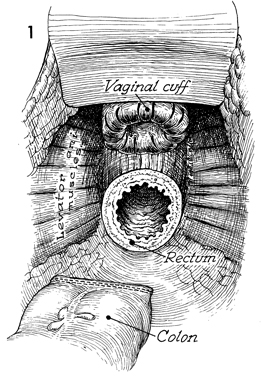
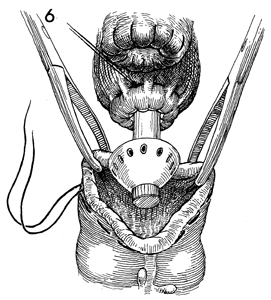
In this view into the pelvis after anterior
resection of the colon and complete hysterectomy have been performed,
the vaginal cuff can be seen to be reefed with absorbable suture.
The rectal stump is shown at the level of the levator ani muscles.
The descending colon has been closed with the automatic surgical
stapler. |
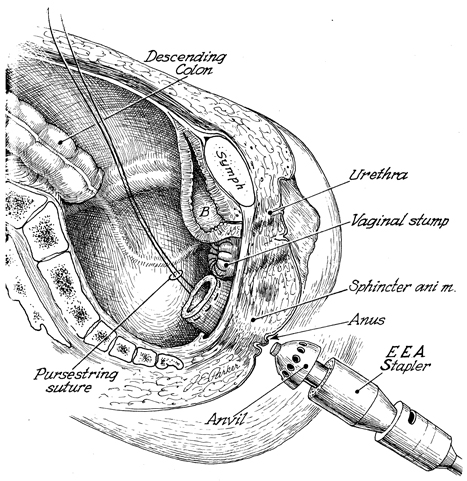
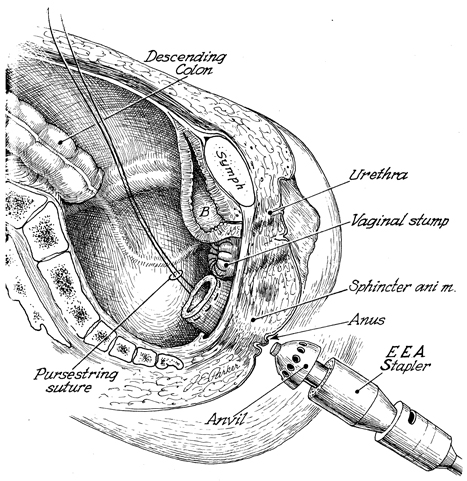
In this sagittal section of the female pelvis
following removal of the uterus and lower rectosigmoid colon,
note that the vaginal vault has been reefed with interrupted
absorbable sutures. The EEA stapler is in position to be inserted
through the anus. The rectal stump has a pursestring suture of
2-0 nylon in place. The descending colon is noted at the pelvic
brim. B indicates bladder; and Symph, pubic
symphysis. |
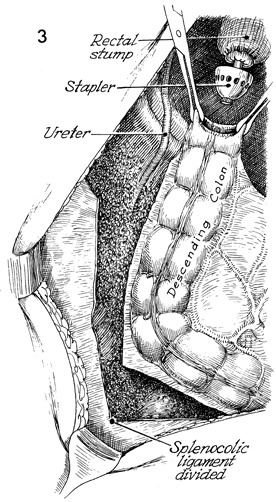
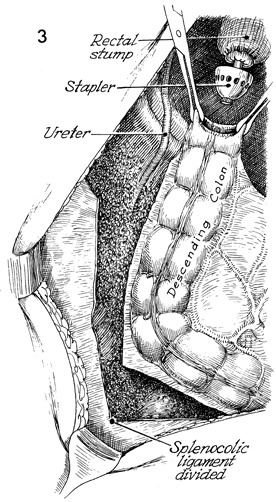
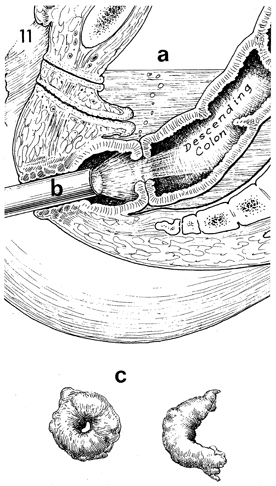
Mobilization of the descending colon is illustrated.
The peritoneum in the left lateral gutter has been incised up
to the splenocolic ligament. The splenocolic ligament has been
clamped and divided. When the colon can be placed into the pelvis
adjacent to the rectal stump without tension, mobilization will
be considered complete. Note the identification of the left ureter,
which must be kept in view at all times. At the top, the EEA
stapler has been placed through the rectal stump. The pursestring
suture has been tied around the central rod, and the anvil of
the stapler has been opened. Allis clamps are used to guide the
descending colon over the anvil. |

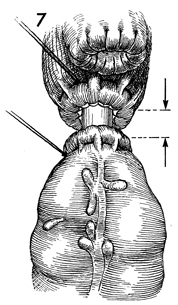
A pelvic view shows the vaginal
cuff reefed with synthetic absorbable suture. A pursestring suture
has been placed in the rectal stump and tied around the central
rod of the EEA stapler. The anvil of the stapler has been advanced,
and the descending colon has been mobilized from above. At this
point, the descending colon contains two rows of surgical staples
that prevent spillage of its contents into the wound. |
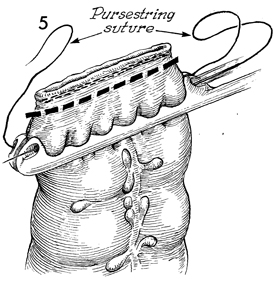
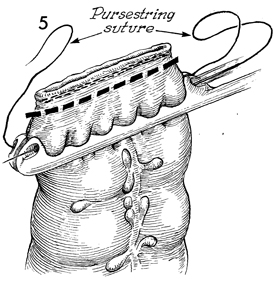
In this view, a 2-0 nylon suture on a Keith
needle passes through the eye of the special pursestring-applying
clamp on the opposite side; the suture exits at the heel of the
clamp, reenters the eye on the proximal side, and exits the eye
at the toe of the clamp. Thus, a pursestring suture is placed
3 mm from the margin of the dotted line for transecting
the descending colon. The colon is now transected beneath the
double row of stainless steel surgical staplers at the level
of the dotted line. |
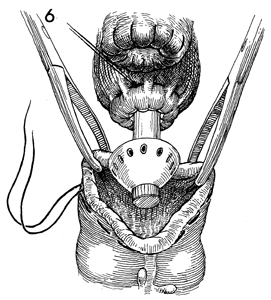
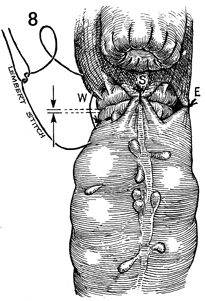
The lumen of the descending
colon is held open with Allis clamps. The anvil of the EEA stapler
is inserted through the open lumen. Note the pursestring on the
left side of the colon. |
The pursestring suture is tied around the
central rod. By closing the wing nut on the handle of the automatic
surgical stapler, the surgeon mechanically approximates the two
ends of the bowel. |
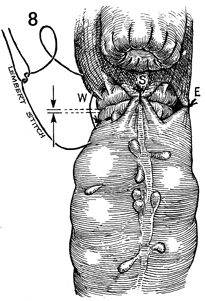
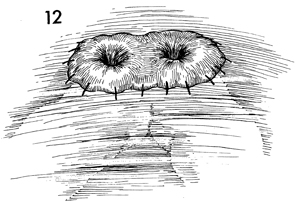
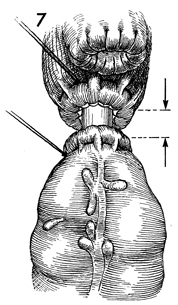
When the mechanical approximation of the
two ends of bowel is satisfactorily completed, four synthetic
absorbable Lembert sutures are placed north, east (E), south
(S), and west (w) to relieve tension on the suture line and to
give added support to the anastomosis. |
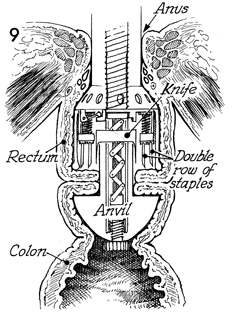
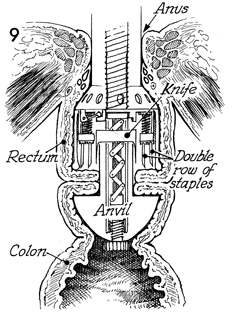
In this sagittal section showing the approximated
rectum and colon, the EEA stapler is loaded with a double row
of staples that have passed through the inverted margins of the
intestine. At the same time, the circular scalpel within the
stapler cuts away excessive inverted bowel.
The surgeon reopens the stapler
by turning the wing nut on the handle. The stapler is slowly
brought through the fresh anastomosis with a twisting motion
and is removed from the patient. |

If adequate omentum is available,
a J flap is made and brought into the pelvis to cover the anastomosis
(see Omental Pedicle "J" Flap). |
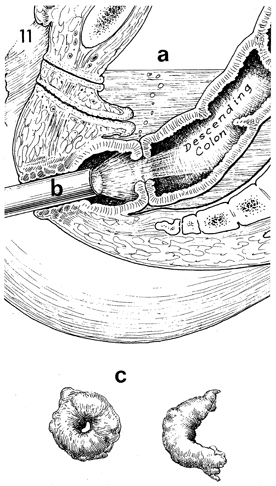
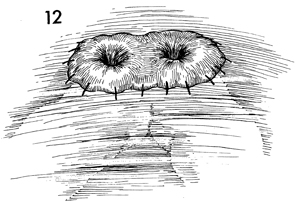
In this sagittal section of
the pelvis after the EEA stapler anastomosis has been completed,
the pelvic cavity is filled with sterile saline solution (a),
and a sterile sigmoidoscope is advanced through the anus up to
the level of the anastomosis (b). The entire
anastomosis is observed. If points of hemorrhage are noted, they
are coagulated. If defects are present, they are noted. A small
volume of air is pumped into the rectum. The stapled anastomosis
should be airtight. If there is a defect, bubbles will rise to
the surface of the saline solution and can be observed by the
surgeon. The EEA stapler is dismantled, and the two pieces of
bowel, rectum and colon (c), are removed from
the stapling device. In all cases they should be complete circles.
If they are not complete circles, a defect in the anastomosis
is indicated, and the anastomosis should be taken down and repeated,
or the defect should be appropriately closed with suture. |
In cases where the pelvis has been previously
irradiated, a protective diverting transverse loop colostomy
is performed at a convenient location. |
|