|
||||||
Small
Bowel Resection Small
Bowel Bypass Small
Bowel Bypass Terminal Ileectomy |
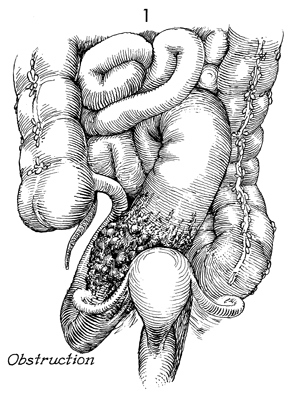
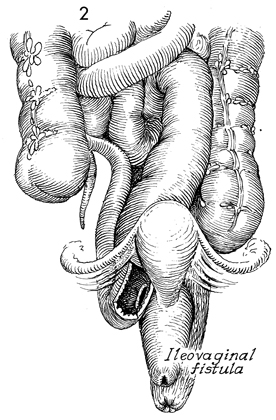
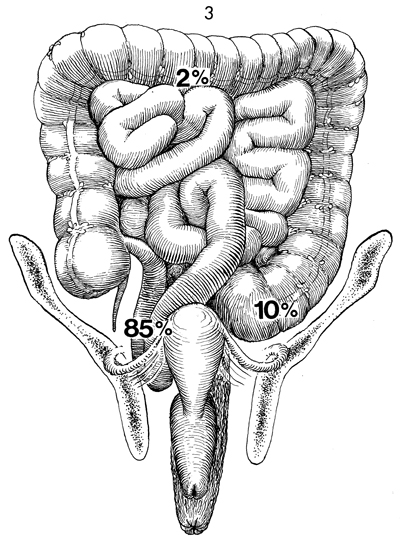
Small Bowel Surgery In cases of extensive gynecologic or pelvic malignancy, particularly those associated with previous irradiation, the efficacy of small bowel bypass for obstruction, fistula formation, and stenosis is well established. Recently, the efficacy of terminal ileectomy with right colectomy and Ileotransverse colostomy has also been demonstrated. Segmental intestinal resection and anastomosis often result in numerous incidental enterotomies, with the spillage of intestinal contents increasing the danger of postoperative pelvic sepsis. The dissection required for intestinal resection leaves large, raw, irradiated areas where the new intestinal anastomoses may adhere, necrose, and produce recurrent fistulae formation. This procedure has been shown to have an abnormally high operative mortality and, therefore, should be avoided if possible. The decision to reexplore the patient 4 to 5 months after the small bowel bypass, take down the bypass segment, and eliminate the abdominal wall intestinal mucous fistula stoma is one that requires sound, mature surgical and oncologic judgment. When in doubt, the mucous fistula stoma should be left in place. The two most common pathologic events related to pelvic disease that occur in the small bowel are obstruction and fistula formation in the terminal ileum. These are demonstrated in Figures 1 and 2. Figure 3 shows the percentages of injuries as related to the intestine, secondary to pelvic surgery and/or disease. Approximately 85% of all intestinal problems related to pelvic disease or obstetric and/or gynecologic surgery are located in the terminal ileum. This is probably because the terminal ileum generally remains in the true pelvis and, therefore, is readily accessible to irradiation injury and/or pelvic adhesion formation. In contrast, only about 10% of intestinal injuries are in the rectum or the sigmoid colon, and less than 2% involved either the transverse colon, jejunum, or other parts of the intestine. This is an important surgical fact in that it assists the surgeon at exploratory laparotomy, when multiple dilated loops of bowel are encountered too rapidly, to identify the diseased segment of small bowel. After identifying the cecum, the surgeon can trace the terminal ileum back for 3 feet and find the pathologic problem in 85% of cases. This is far easier than identifying the ligament of Treitz and tracing the small bowel distally toward the cecum. Figures 1 and 2 illustrate the anatomic condition of the small bowel associated with obstruction and combinations of obstruction and fistula formation. The small intestine proximal to the obstruction will be dilated 2-3 times the diameter of intestine distal to the disease. This is helpful in identification of efferent and afferent loops of bowel. The purpose of these operations is to radically resect or bypass a point of disease in the small bowel. Physiologic Changes. The terminal ileum is responsible for absorption of fat-soluble vitamins plus vitamin B12. Patients who have extensive loss of the ileum can be left with what has been referred to as short bowel syndrome. This consists of diarrhea, failure to absorb the fat-soluble vitamins (A, D,E, K) plus vitamin B12, and difficulty in absorption of high-molecular-weight fats. Many of these patients need postoperative assistance from a medical gastroenterologist to adjust their diet, control diarrhea, and generally help them to adapt to the rearrangement of their anatomy. Points of Caution. The most important aspect of performing a small bowel resection or bypass is to ensure the vascular integrity of the bowel to be anastomosed. This is aided by keeping trauma to the bowel wall at a minimum. All open mesenteric areas must be closed. Internal hernia and obstruction are serious and can be fatal complications in these heavily irradiated patients. The advantage of small bowel bypass over small bowel resection is that it avoids extensive dissection in a heavily irradiated fibrotic pelvis. Only that dissection needed to perform the bypass should be made and, the remainder of the diseased bowel should be left impacted in the heavily irradiated pelvis. Since both procedures, resection and bypass, are required at different times in pelvic surgery, however, both are illustrated in this section.
|
|||||
Copyright - all rights reserved / Clifford R. Wheeless,
Jr., M.D. and Marcella L. Roenneburg, M.D.
All contents of this web site are copywrite protected.