Small
Bowel
Small Bowel Surgery
Small
Bowel Resection
With End-to-End
Anastomosis Using the Gambee Technique
Small
Bowel Bypass
With Ileoileal
Anastomosis and
Mucous Fistula
Small
Bowel Bypass
With Ileotransverse
Colostomy and Mucous
Fistula
Terminal
Ileectomy
With Right Colectomy
and Ileotransverse
Colostomy |
Small Bowel Resection
With End-to-End Anastomosis
Using the Gambee Technique
Small bowel resection is preferred over small bowel
bypass in situations where the pathologic condition is confined to
a segment of the small bowel that is not impacted in a dense irradiation
fibrotic pelvis or where a knuckle of small bowel is involved within
a pelvic tumor. Resection over bypass should also be performed in those
cases where extensive dissection of the small bowel to locate and mobilize
the pathologic segment is not required. If the surgeon insists on mobilization
and resection of all small bowel disease, the surgeon must be willing
to resect the ileum and right colon and perform a high ileotransverse
colostomy. The multiple enterotomies not only spill intestinal contents
into the wound but also are frequently overlooked at the time of repair.
In addition, those enterotomies that are repaired become adherent to
the dense irradiated fibrotic pelvic walls and break down at the suture
line to form recurrent enteric cutaneous and/or vaginal fistulae. In
summary, experienced pelvic surgeons have learned (usually the hard
way) that small bowel resection should be confined to those few cases
where the pathologic segment of the small bowel can be easily mobilized
and isolated. Otherwise, small bowel bypass should be performed.
The
pathologic segment of small bowel is removed, and the remaining small
bowel is reanastomosed to a healthy segment of intestine.
Physiologic Changes. Removal
of extensive segments of small bowel may produce postoperative diarrhea
and failure of fat-soluble vitamin absorption.
Points of Caution. The predominant point of caution
in resection of the small bowel is to ensure the vascular integrity
of the anastomosis. The vascular supply of the terminal 10 cm of small
bowel is unreliable. In heavily irradiated patients it is preferable
to perform an ileoascending colostomy rather than an ileoileostomy
for anastomosis in the terminal 10 cm of the ileum.
Technique
Small bowel resection with end-to-end anastomosis using
the Gambee technique is demonstrated here. Anastomosis using the surgical
stapler technique is shown in Bladder and Ureter - Intestinal Loop
Urinary Diversion.
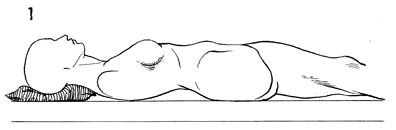
Patients for small bowel resection are placed
in the supine position. A Foley catheter is inserted into the
bladder. A sump-type nasogastric tube is passed into the stomach. |
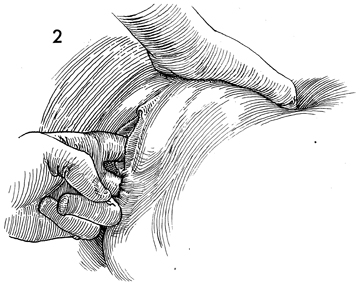
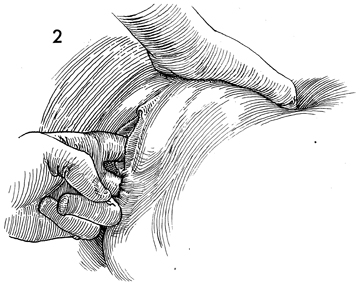
A thorough bimanual examination is performed
prior to the operation. |
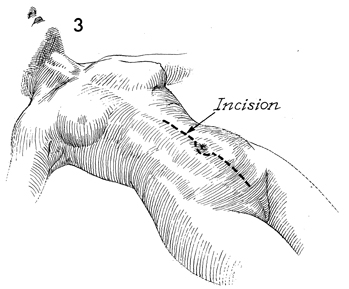
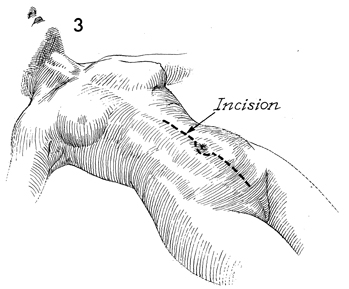
A midline incision is made,
usually extending around the umbilicus. The abdomen is entered
and explored. As previously stated, in the majority
of cases, small bowel disease associated with pelvic disorders
is located within 3 feet of the ileocecal bowel. This fact is
of significant value to the pelvic surgeon in that it allows
the surgeon to trace the small bowel back from the cecum rather
than trace the bowel down from the ligament of Treitz.
At this point, the decision
must be made to perform either a small bowel resection or small
bowel bypass. If the limits of the small bowel disease are identifiable
and can be mobilized without extensive dissection, small bowel
resection is the procedure of choice. If, however, as in the
majority of cases, the diseased segment of small bowel is embedded
deep in the true pelvis, particularly after heavy pelvic irradiation,
it is wiser to perform a small bowel bypass. |
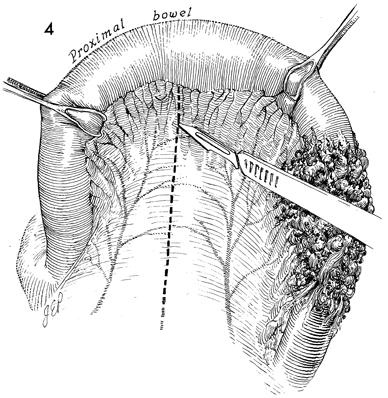
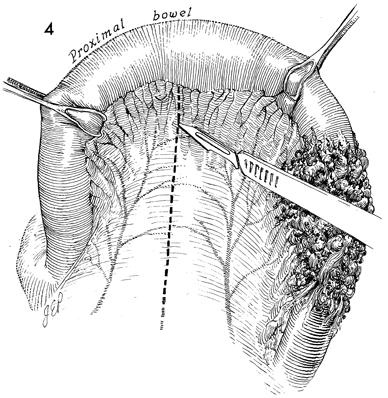
The small bowel to be resected
is mobilized, and the mesentery is carefully studied for vascular
arcades. A point of transection is selected sufficiently distant
from the diseased portion and in the immediate vicinity of a
healthy vascular arcade. The bowel should be suspended between
Babcock clamps or warm moist saline gauze held between the thumb
and first finger. The peritoneum of the mesentery is opened with
a scalpel, using a delicate technique that does not transect
the underlying blood vessels. |
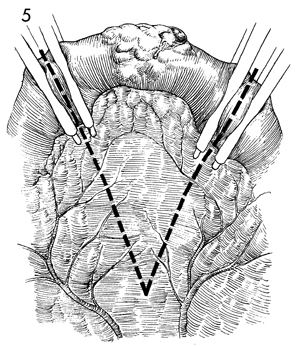
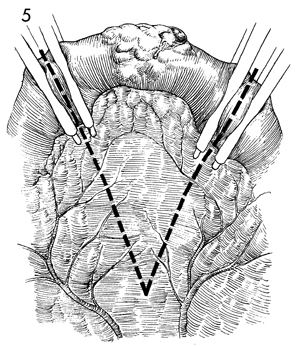
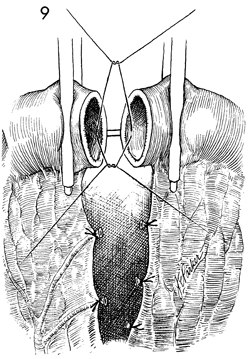
Linen-shod intestinal clamps are applied
proximal and distal to the point of transection. The mesentery
is opened in a V-shaped fashion. The small vessels crossing the
line of transection are clamped and tied. |
The bowel to be resected
is held by an assistant while the surgeon creates small openings
in avascular segments of the mesentery along the line of transection.
Small vessels are clamped and tied with Dexon suture.
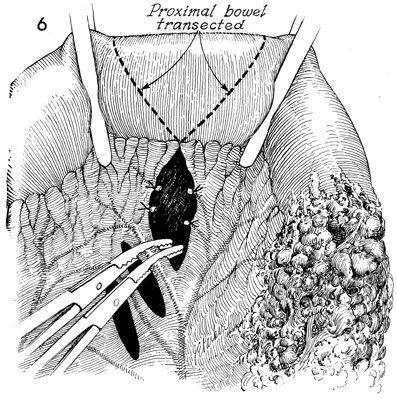
Note that the line of transection
in the bowel is oblique rather than perpendicular. The blood supply
to the small bowel is such that the antimesenteric border of the
bowel can become ischemic if the vascular arcade supplying the
edge of the resected bowel is transected perpendicularly. A second
reason for transecting the bowel in an oblique rather than a perpendicular
line is that an oblique transection will give a larger anastomosis
and reduce the incidence of stricture formation. |
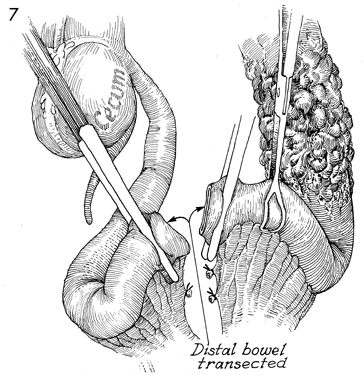
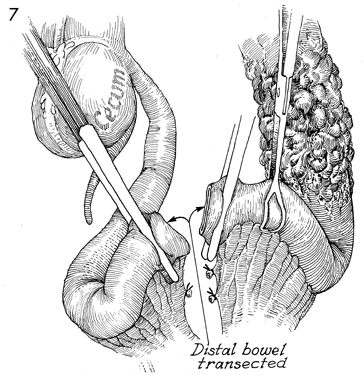
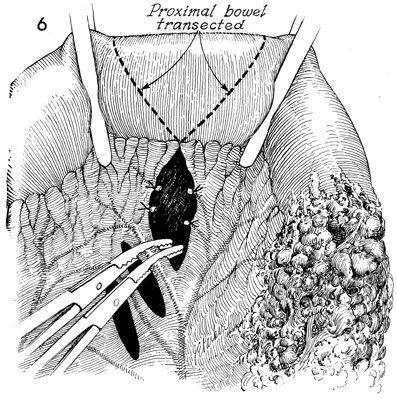
The bowel has been transected, and the diseased
portion has been stapled off with the TA-55 surgical stapler
and separated from the health terminal ileum and cecum. |
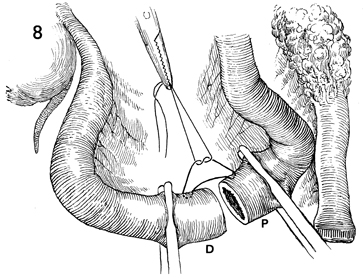
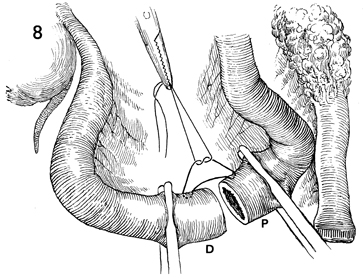
The diseased portion of bowel has been removed
to the side, and a healthy segment of the proximal ileum (P)
is brought down to anastomose to a healthy segment of the distal
ileum (D).
The first step in this anastomosis
is to place a Lembert suture of 3-0 Dexon through the mesenteric
border approximately 1 cm from the edge of the mucosa. The purpose
of this stitch is to take tension off the future suture line
and to hold the intestine in appropriate approximation for the
remainder of the anastomosis. |
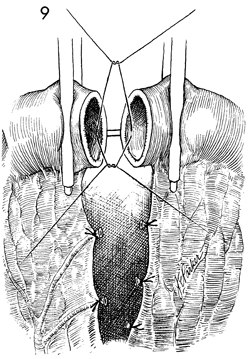
The intestine is now available for the Gambee
technique of single-layer through-and-through suture anastomosis. |
|
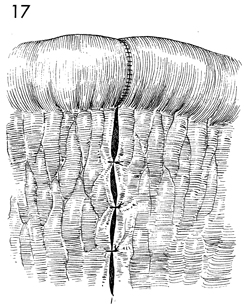
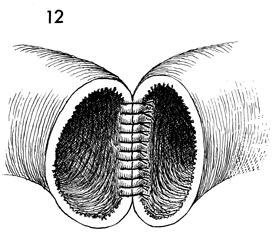
GAMBEE
TECHNIQUE The steps of the Gambee technique are outlined
in Figures 10-17. |
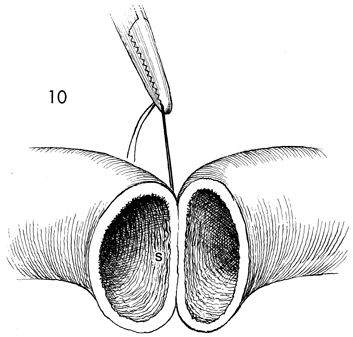
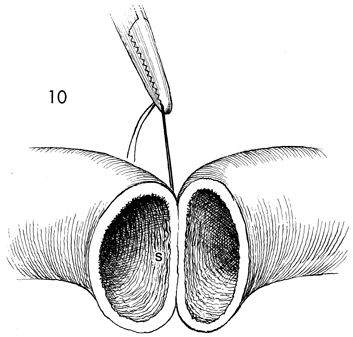
The first step in the Gambee technique is
to place the suture, previously noted in Figure 8, on the mesenteric
border of the intestine. This is referred to here as the south
(S) suture. |
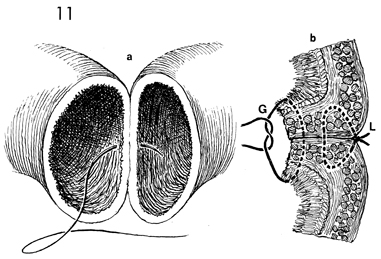
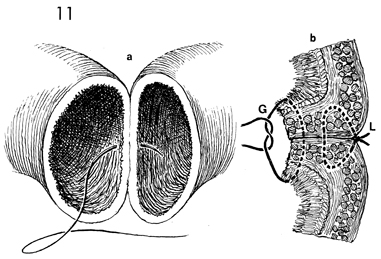
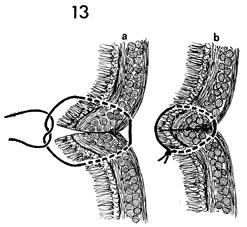
The Gambee technique is a single-layer through-and-through
anastomosis; all knots are tied within the lumen of the bowel. b is
a cross section of a. Note that the initial
Lembert suture (L) placed at the mesenteric border of
the bowel has been tied and thus tends to invert the edges of
the mucosa. The Gambee suture (G) has been placed through
the mucosa; the entire wall of the bowel exits the serosa, enters
the serosa of the bowel on the opposite side, passes the bowel
wall, and emerges from the mucosa. When tied, it further inverts
the edge of the bowel. |
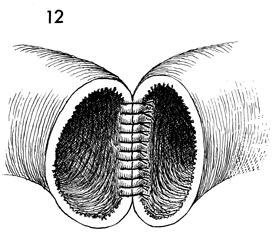
Each successive Gambee suture is placed approximately
3 mm apart around the entire circumstance of the bowel. |
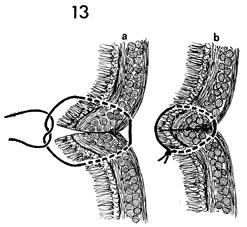
A cross section of the Gambee suture reveals
the path of the suture. In a, the suture enters
the bowel through the mucosa, passes through the entire wall
of the bowel, exits from the serosa, passes back through the
serosa of the opposite segment of bowel, penetrates the entire
bowel wall, and exits the mucosa. In b, the
Gambee suture is tied with the knot on the lumen side of the
bowel, tending to invert the anastomosis. |
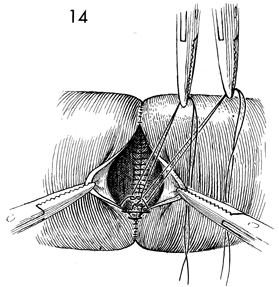
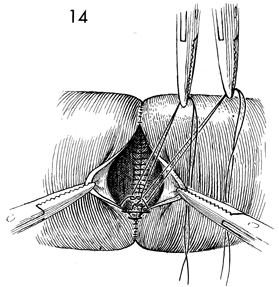
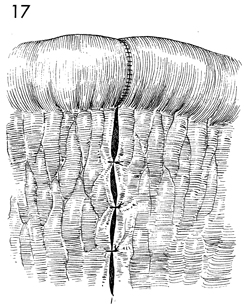
The process has been almost completed around
the entire circumference of bowel. |
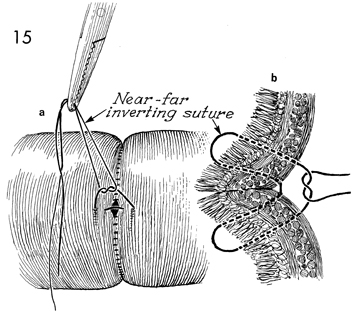
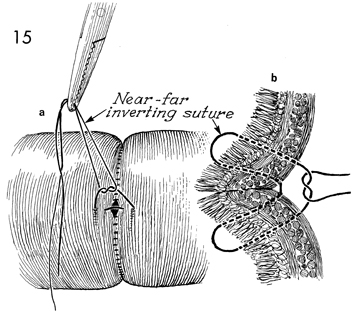
When all but a 5-mm defect in the bowel remains,
the near-far inverting suture can be applied. a shows
the near-far inverting suture in place. When tied, it will dramatically
invert the entire suture line. b is a cross
section of the near-far inverting suture, outlining the details
of the technique. Note that the near-far inverting suture is
the only stitch in the Gambee technique that is tied on the serosa
of the bowel rather than the mucosa of the bowel. The stitch
is started by placing the suture through the serosa of one segment
of bowel approximately 1 cm from the edge. It penetrates the
entire surface of bowel and exits the mucosa approximately 1
cm from the edge. The suture is immediately reversed and is passed
back through the mucosa of the same segment of bowel 3 mm from
the edge, penetrates the entire wall of the same segment of bowel,
and exits the serosa. This is the near and the far aspect of
this stitch. The suture is then placed through the near edge
of the opposite segment of bowel 3 mm from the edge through its
serosa to penetrate the entire wall of the intestine and exit
from the mucosa. The needle is immediately placed back through
the mucosa approximately 1 cm from its edge, penetrates the entire
wall of the bowel, and exits from the serosa approximately 1
cm from its edge. Tying the suture dramatically inverts the entire
anastomosis. |
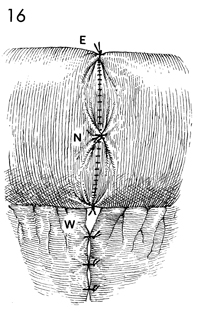
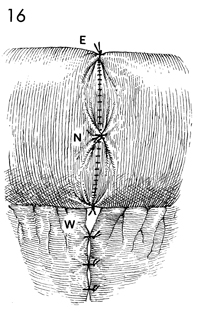
Four tension-relieving Lembert sutures of
3-0 Dexon are placed north (N), east (E), and west (W) of the
bowel. These sutures further invert the anastomosis and take
tension off the suture line to improve healing. |
The mesentery of the small intestine is closed
with interrupted 3-0 synthetic absorbable sutures to prevent
internal hernia. |
|