Bladder
and Ureter
Insertion
of Suprapubic Catheter
Retropubic
Urethropexy:
Marshall-Marchetti-Krantz
and Burch Operations
Ureteroureterostomy
Ureteroneocystostomy
and Ureteroneocystostomy
With Bladder Flap
Transperitoneal
Ureteroureterostom
End-to-Side Anastomosis
Intestinal
Loop
Urinary Diversion
Percutaneous
Nephropyelostomy
Ureteroileoneocystostomy
Clam
Gastrocystoplasty |
Retropubic Urethropexy:
Marshall-Marchetti-Krantz
And
Burch Operations
The Marshall-Marchetti-Krantz (MMK) and Burch operations
for stress incontinence of urine are two of the retropubic urethropexy
"pin-up" operations that essentially return the urethrovesical angle
to its role as an intra-abdominal organ and change the focal points
of pressure applied through the abdomen during a Valsalva maneuver
(coughing, sneezing, etc.)
Unlike other stress incontinence operations,
the Marshall-Marchetti-Krantz and Burch operations do not, by themselves,
produce significant changes in intraurethral or intravesical pressure
to restore urinary continence.
The operations have evolved with several
alterations since their original introduction by Marshall-Marchetti-Krantz
and Burch. These procedures can be performed at the time of pelvic
surgery for uterine or adnexal pathology.
The purpose of these operations
is to eliminate stress incontinence of urine.
These operations do not correct a cystourethrocele. When this is present,
it should be surgically corrected through the vagina.
Physiologic Changes. The Marshall-Marchetti-Krantz
and Burch operations rarely change the relationship between intraurethral
pressure and intravesical pressure. They make the proximal urethra
and bladder neck and intra-abdominal organ and equalize intra-abdominal
pressures on the bladder wall that are precipitated by a Valsalva maneuver.
Points of Caution. To ensure the integrity
of the bladder and ureters, a cystotomy should be performed, and the
bladder should be inspected under direct vision.
When operating in
the space of Retzius, bleeding from the plexus of Santorini can be
difficult to control. Total hemostasis is essential before these operations
are completed.
Technique
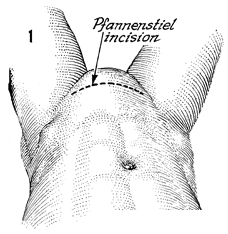
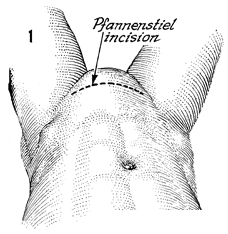
For the Marshall-Marchetti-Krantz
and Burch operations, the patient is placed in the supine lithotomy
position, i.e., the ski position. There are two acceptable incisions,
the lower midline incision and the transverse incision. Each
has its advocates. It is difficult to demonstrate superior results
with either incision. The supine lithotomy position (ski) with
a transverse incision is preferred unless the patient is undergoing
surgery for a gynecologic oncologic problem.
The patient is prepped
and draped, and a Foley catheter with a 30-mL bag is inserted. |
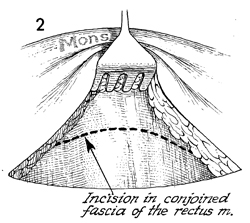
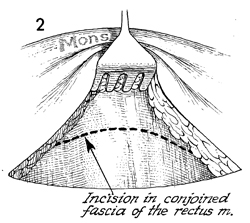
The incision is made in the rectus fascia.
The fascia is excised. |
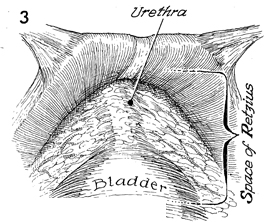
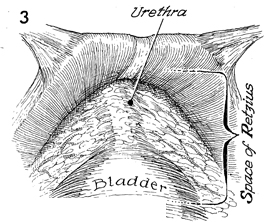
The space of Retzius is entered. The bladder
and the urethrovaginal angle are identified with the aid of the
Foley catheter. |
|
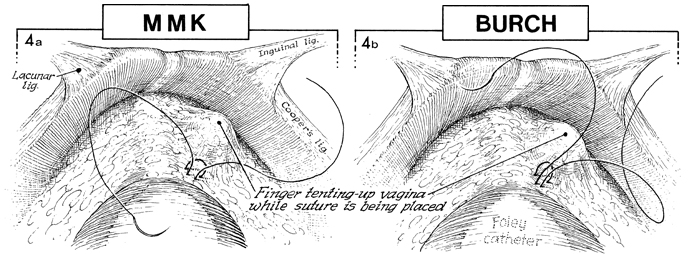
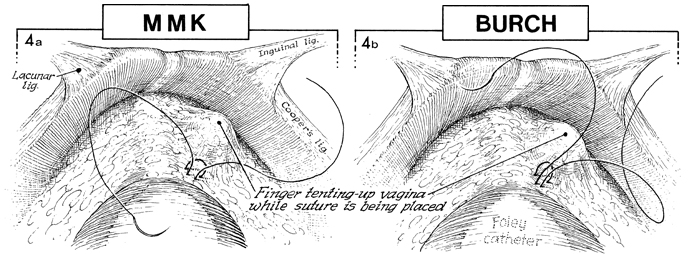
A finger is inserted in the
vagina to identify the perivaginal and periurethral areas for
placement of 0 Prolene suture. We prefer permanent monofilament
suture. A small, curved Mayo needle is used, and the position
of the suture is confirmed by palpating the bladder and inserting
a finger in the vagina before making each suture. Notice blanching
of the blood vessels in the plexus of Santorini. The blood vessels
should be avoided in placing the sutures in the periurethral
tissue. |
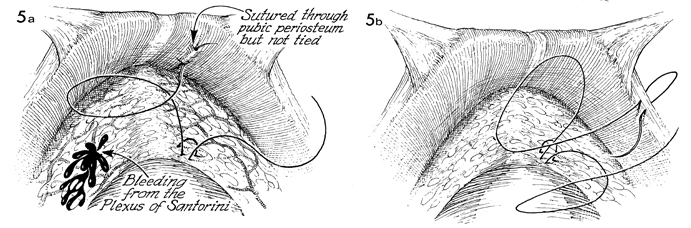
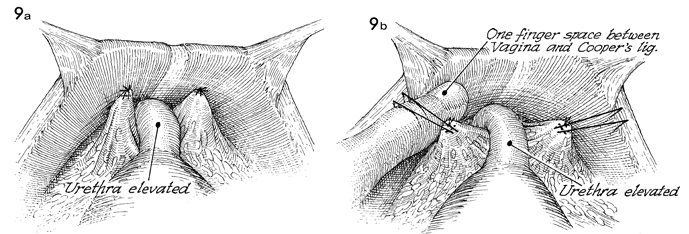
In a, showing
the MMK operation, the suture that has been placed in the periurethral
tissue is tied to the periosteum of the pubic symphysis. In b,
showing the Burch operation, the suture that has been placed
in the periurethral tissue has been brought through the conjoined
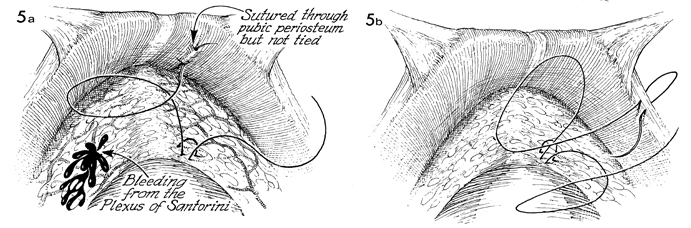
tendon or Cooper's ligament. In a, bleeding
has been produced from the vessels in the plexus of Santorini. |
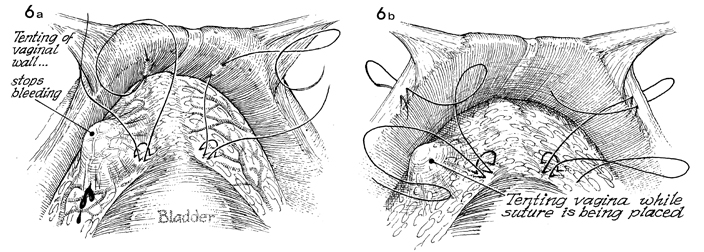
The bleeding produced from
the plexus of Santorini can be easily stopped by elevating the
finger in the vagina. This allows for fulgurating or grasping
and tying each of the bleeders specifically. The blood vessels
form the plexus of Santorini and are difficult to control if
elevation of the vagina is not used to slow the bleeding process.
The suture placed in the periurethral tissue is tied, respectively,
to either the periosteum (MMK) (a) or Cooper's
ligament (Burch) (b). |
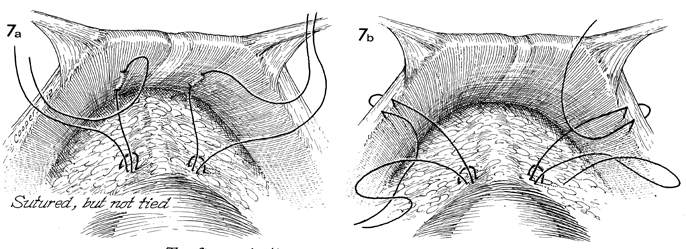
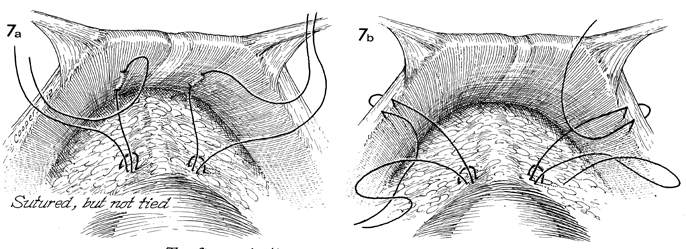
The sutures have been completely
placed but not tied. |
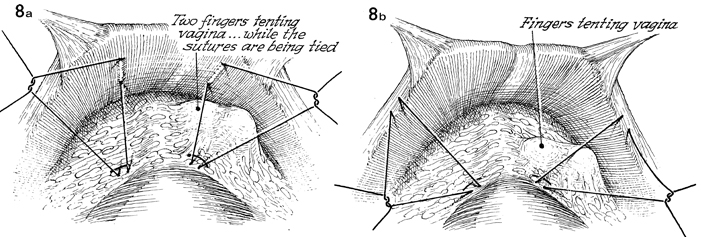
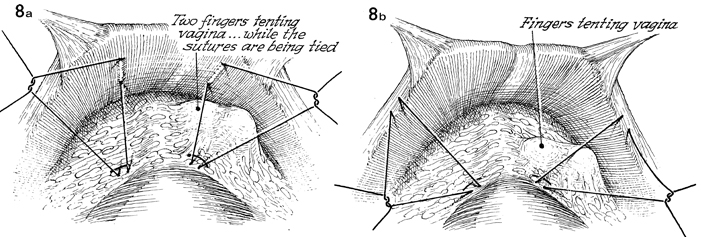
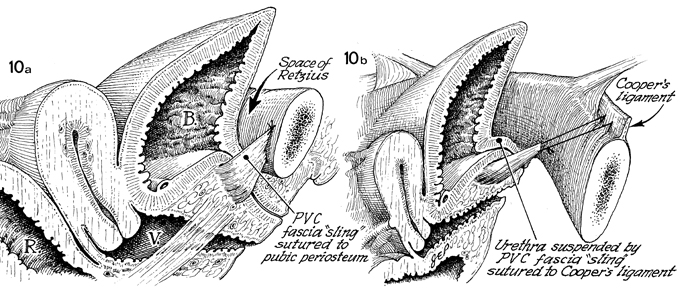
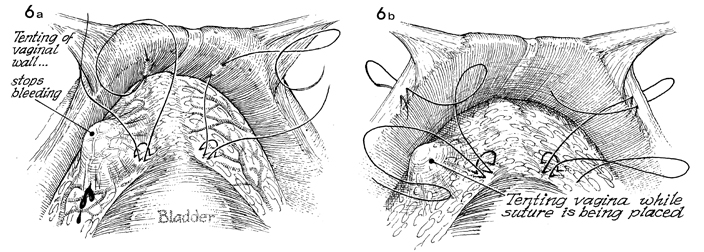
In a (MMK),
two vaginal fingers are used to tent up the anterior wall of
the vagina while the sutures are being tied. The same is noted
in b (Burch),
as the sutures are tied to Cooper's ligament. |
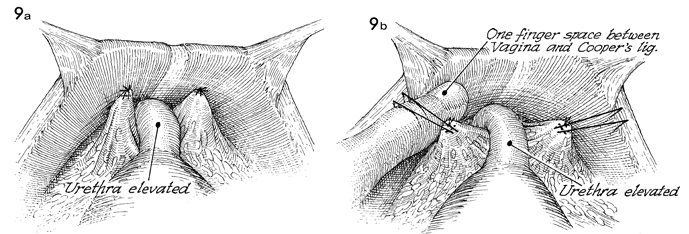
In a (MMK),
the sutures are completely tied to the periosteum of the symphysis
pubis. An additional one or two sutures can be placed if desired.
In b (Burch),
a finger is inserted between the conjoined tendon or Cooper's
ligament and the suture in the periurethral tissue. A 2-cm space
(1 fingerbreadth) is desirable to prevent total occlusion of
the urethra and postoperative urinary retention. |
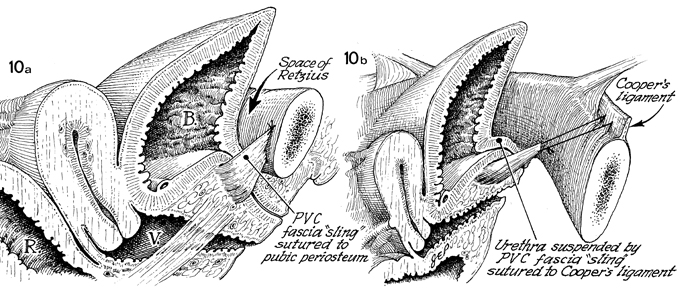
In a (MMK),
the periurethral tissue with the adjacent pubovesical cervical (PVC) fascia
sling is sutured to the periosteum of the symphysis pubis. The
bladder (B) and proximal urethra have been brought back
into the abdomen where intraurethral and intravesical pressures
can be stabilized. In b (Burch), the urethra
has been suspended by the pubovesical cervical fascia sling sutured
to Cooper's ligament. In reality, the pubovesical
cervical fascia in both operations has been made into a sling
to bring the proximal one-third of the urethra and the neck of
the bladder back into the abdomen. This new position allows even
disposition of external pressures on all surfaces of the bladder
and proximal urethra. The rectum (R) and vagina (V) are
shown in a. |
|