Bladder
and Ureter
Insertion
of Suprapubic Catheter
Retropubic
Urethropexy:
Marshall-Marchetti-Krantz
and Burch Operations
Ureteroureterostomy
Ureteroneocystostomy
and Ureteroneocystostomy
With Bladder Flap
Transperitoneal
Ureteroureterostom
End-to-Side Anastomosis
Intestinal
Loop
Urinary Diversion
Percutaneous
Nephropyelostomy
Ureteroileoneocystostomy
Clam
Gastrocystoplasty |
Ureteroneocystostomy and
Ureteroneocystostomy
With Bladder Flap
Reimplantation of the ureter into the bladder is necessary in cases
of congenital anomaly or damage to the ureter secondary to pelvic surgery
or irradiation. If there is total obstruction of the ureter, a percutaneous
needle nephrostomy should be attempted, and surgical repair should
be delayed until ideal conditions for repair are achieved. Every hour
that the kidney remains totally obstructed, progressive damage to the
kidney occurs.
Important points in the procedure are (1) full mobilization of the
bladder to prevent tension on the anastomosis; (2) leaving a Silastic
ureteral stent catheter in the ureter for at least 10-14 days; (3)
adequate drainage of the implantation site to prevent urinary ascites;
and (4) thorough postoperative cystoscopic evaluation with intravenous
pyelogram.
Physiologic Changes. The
ureter is reimplanted into the bladder, if possible, and if not possible,
a flap of bladder can be developed into a tube that can be made and
anastomosed to the ureter at or near the pelvic brim.
The issue of
tunneling the ureter through the bladder wall to prevent reflux remains
an open question. In some cases, reflux of urine and its associated
urinary tract infection can produce pathologic changes of the upper
urinary tracts. Reflux is unusual, however, in adults who do not have
a congenital neuromuscular malformation within the walls of their ureter.
This problem is generally confined to children or young adults with
neuromuscular malformation in the ureter.
Points of Caution. The surgeon must be confident
that the ureter can be reimplanted without tension.
A mucosal-to-mucosal anastomosis should be performed. A Silastic catheter
stent should be inserted through the anastomosis and coiled into the
bladder, with the opposite end placed in the renal pelvis.
The bladder flap must have sufficient width to its base to provide
an adequate blood supply at the tip of the flap.
Technique
URETERONEOCYSTOSTOMY

A thorough bimanual and speculum
examination of the pelvis should be performed prior to ureteroneocystostomy. |

Two mL of indigo carmine solution are injected
intravenously prior to the procedure to provide a urinary marker
for fast identification of the ureter in the distorted pelvic
anatomy. If there is confusion as to whether a tubular structure
is a ureter or a blood vessel, aspiration with a 21-gauge needle
and a 5-mL syringe will yield the blue dye from the indigo
carmine if the structure is the ureter. |
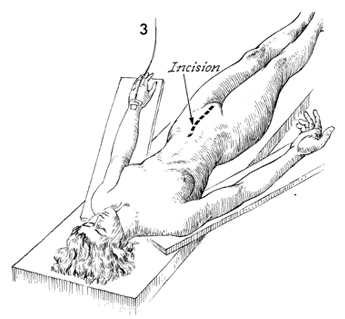
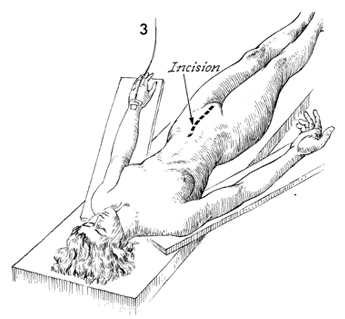
The patient is operated on in the supine
position. A lower midline incision is made. |
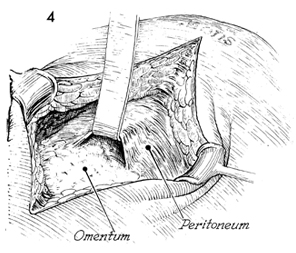
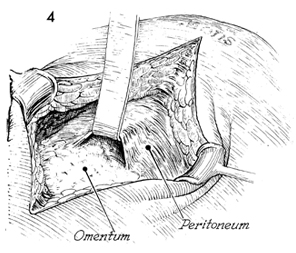
The peritoneum is entered, and the omentum
and intestinal contents are dissected out of the pelvic cavity. |
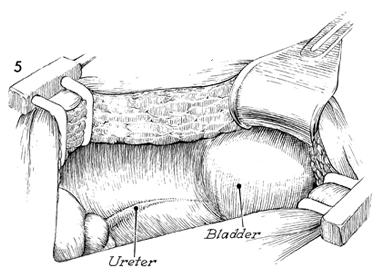
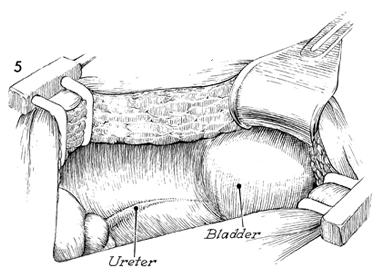
The peritoneum over the ureteral area is
incised at the bifurcation of the common iliac artery, and the
dissection is continued into the pelvis until the damaged portion
of the ureter is exposed. |
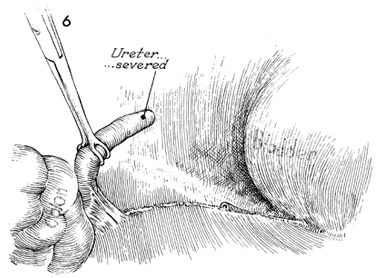
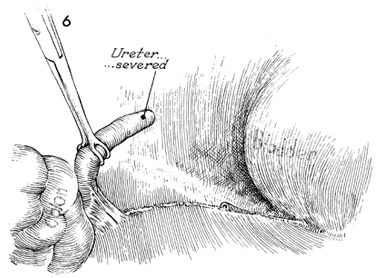
The ureter is transected
above the damage, and the distal end is tied with 0 synthetic
absorbable suture. The proximal portion is dissected out of its
bed with careful surgical technique to ensure the continuity
of the ureteral sheath that is so important for adequate blood
supply to the ureter. |
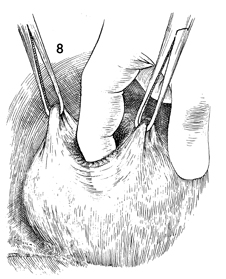
The bladder is mobilized by
entering the space of Retzius behind the pubic symphysis and
dissecting the bladder cephalad so that a portion of posterior
bladder wall meets the proximal portion of ureter to be implanted.
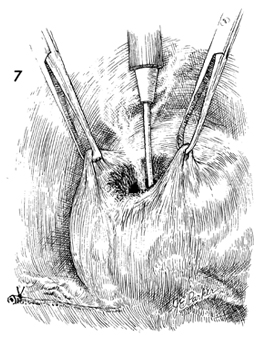
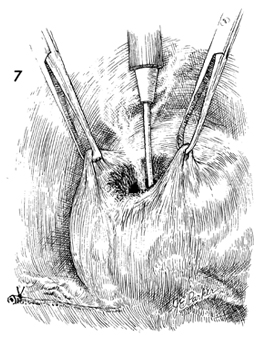
The dome of the bladder is picked up with Allis clamps, and a
cystostomy is made by cautery. |
The defect is expanded by
blunt dissection with the finger to reduce bleeding. |
The bladder is brought into position adjacent
to the proximal portion of the ureter to ensure that there is
adequate mobilization of the bladder and that the anastomosis
will be free from tension. |
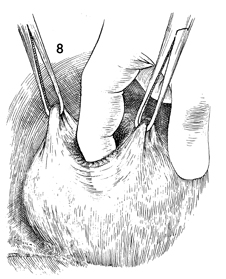
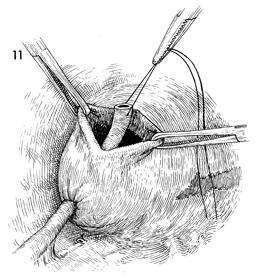
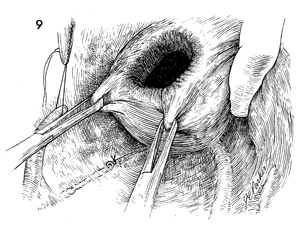
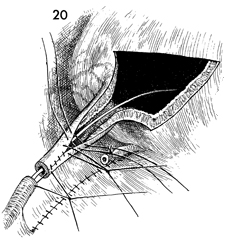
A Kelly clamp is inserted in the bladder
through the cystostomy and pressed against the bladder wall at
a point adjacent to the ureter to be implanted. The Kelly clamp
is advanced through the bladder wall and opened sufficiently
to allow at least a 2-cm defect. The tip of the ureter is sutured
with a 3-0 suture and grasped with the Kelly clamp. |
The ureter is drawn into the bladder through
the cystostomy. |
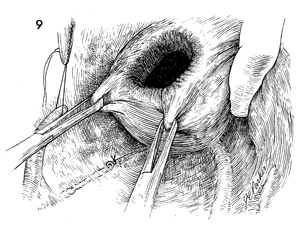
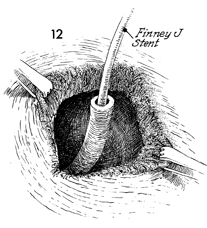
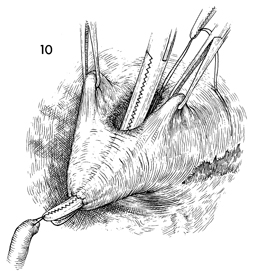
A No. 8 French Silastic double-J
urethral stent catheter is inserted into the ureter and advanced
to the renal pelvis. A small fish-mouth incision is made at the
3 o'clock and 9 o'clock positions in the ureter with scissors
or a scalpel to prevent iris contracture at the anastomosis. |
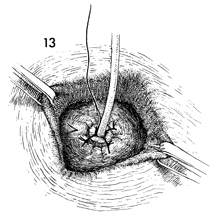
Under direct vision the ureter is anastomosed
mucosa to mucosa to the bladder with interrupted 4-0 synthetic
absorbable suture. |
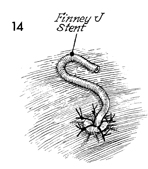
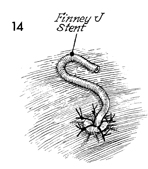
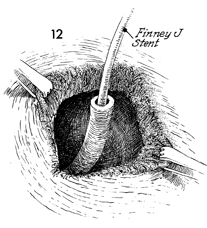
A Finney "J" catheter stent
is inserted up into the ureter. The J catheter stent is designed
to prevent peristalsis from pushing the catheter out of the ureter
and into the bladder. We prefer to leave the catheter in the
bladder for a minimum of 12 days and, in irradiated patients,
for approximately 3 weeks. |
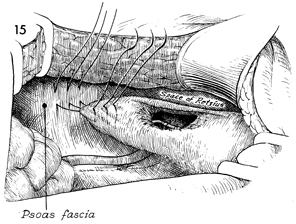
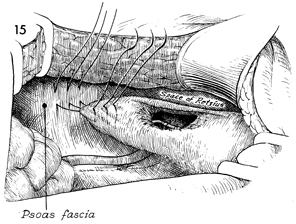
To ensure that the anastomosis will be free
of tension, a site on the psoas fascia is located, and the dome
of the bladder is sutured to it with multiple interrupted 0 synthetic
absorbable sutures. The bladder is mobilized by entering the
space of Retzius. |
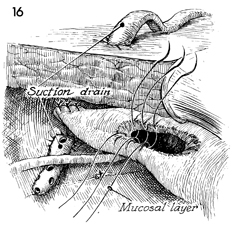
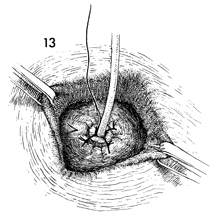
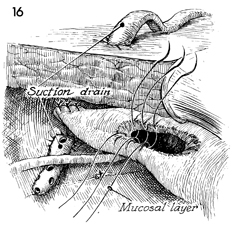
A soft closed suction drain is placed through
the lower quadrant of the abdomen adjacent to the ureteroneocystostomy.
The cystostomy in the dome of the bladder is closed with interrupted
3-0 synthetic absorbable sutures in two layers. Three of the
first layer sutures are shown. |
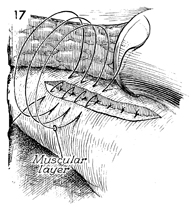
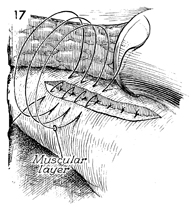
A running 3-0 synthetic absorbable suture
is used to close the bladder musculature and serosa. |
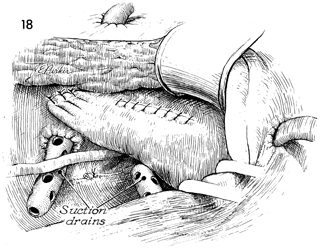
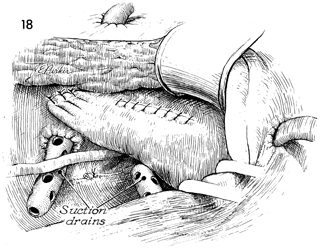
An additional closed suction drain is placed
through the opposite lower quadrant and brought adjacent to the
anastomosed area. These drains should remain in place until no
urinary drainage is noted. |
BLADDER FLAP |
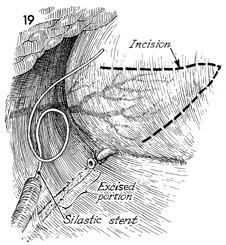
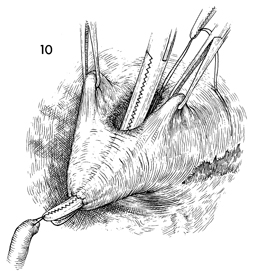
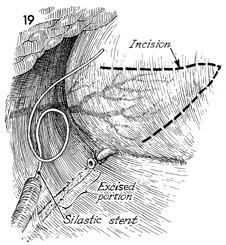
Occasionally, the excised portion of ureter
is so great that anastomosis with the bladder cannot be made
without tension. This is frequently the case in ureteral stricture
resulting form irradiation. Rather than chance placing the ureteroneocystostomy
under tension that will result in retraction of the ureter, stenosis,
and eventually hydronephrosis, it is preferable to create a bladder
flap from the dome of the bladder that can extend to the transected
ureter. This is begun by measuring the distance between the bladder
wall and the proximal portion of the ureter. This distance, usually
8-9 cm, is marked off on the posterior bladder wall with brilliant
green in the area of insertion of the superior vesical artery.
The flap is incised out of the bladder wall by use of scissors
or scalpel. The base of the flap should be wider than the length.
A No. 8 French Silastic ureteral catheter is inserted into the
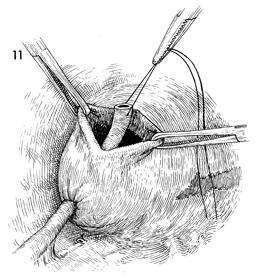
ureter to the renal pelvis. |
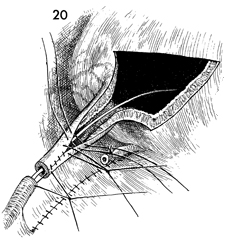
The flap is raised and brought
into a position adjacent to the proximal portion of the ureter.
Care must be taken at this point to ensure that there is no
tension on the anastomosis. If an inadequate flap has been
developed, the flap incisions may be extended at the base of
the flap. The flap is rolled in a tubular fashion and closed
with interrupted 4-0 synthetic absorbable suture over the catheter.
An end-to-end anastomosis
between the proximal ureter and the tube flap is made with
interrupted 4-0 synthetic absorbable suture. A single layer
of through-and- through 4-0 synthetic absorbable suture is
used for closure of the tube flap, rather than the two-layer
technique normally used on the bladder wall. This alteration
in technique guards against stenosis in the bladder flap that
could result from a two-layer closure. |
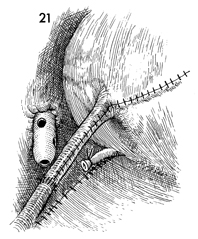
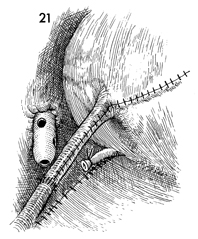
The bladder wall is closed by using the two-layer
technique, the first on the bladder mucosa and the second layer
on the muscle and serosa (as in Figs. 16 and 17). A closed suction
drain is brought into the anastomosis site through the lower
quadrant of the abdomen. The ureteral catheter is left in place
for a minimum of 2 or 3 weeks. It is removed by water cystoscopy. |
|
|