|
Fimbrioplasty
Fimbrioplasty is one of several reconstructive procedures designed
to correct infertility.
The term fimbrioplasty is preferred over salpingostomy or simply opening
the Fallopian tube, since salpingostomy does not address the important
role of the fimbriae. Reconstruction, with care taken to preserve and
release the multiple delicate fimbriae, is vital to making pregnancy
possible. The operation should not be performed until a complete infertility
evaluation of the couple has been made.
The purpose of the operation
is to open the obstructed Fallopian tube and salvage enough function
of the fimbriae to allow successful entrapment and transport the oocyte.
Physiologic Changes. The Fallopian tube is opened,
and the fimbriae are restored.
Points of Caution. Meticulous
hemostasis is absolutely essential if this procedure is to succeed.
Care must be exercised not to jeopardize the vascularity of the Fallopian
tube by excessive dissection of the mesosalpinx from the ovary. In
addition, irrigation, suction, and needlepoint electrocautery should
be used to control hemostasis rather than sponging, clamping, and tying
of bleeding blood vessels.
Technique
Before fimbrioplasty, the surgeon should
perform a diagnostic laparoscopy.
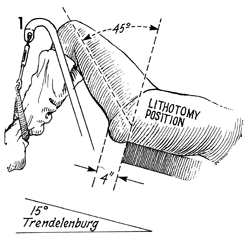
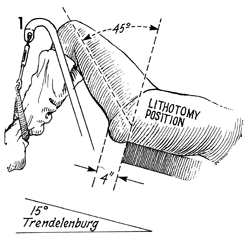
For diagnostic laparoscopy,
the patient is placed in the dorsal lithotomy position with the
hips flexed 45°, the knees flexed
at 90°,
and the buttocks extended at least 4 inches beyond the edge of
the operating table. The patient is placed in approximately a
15° Trendelenburg position. |
A thorough bimanual pelvic examination is
performed. |
The laparoscopic instruments are introduced
as recommended, under Laparoscopy Technique, and the pelvis is
thoroughly inspected. If there is gross hydrosalpinx or gross
damage to the Fallopian tubes on both sides, it may be wise to
abandon the procedure. The ideal patient for fimbrioplasty has
a Fallopian tube that is normal except for the fimbriae, which
are agglutinated or clubbed. The clubbed end of the tube is slightly
distended by the injection of indigo carmine solution through
the uterus during laparoscopy. The laparoscopic instruments are
withdrawn; the small umbilical incision is closed with a 3-0
subcuticular suture. |
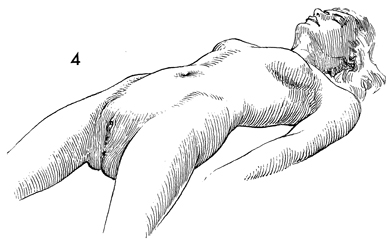
Two positions can be used for fimbrioplasty.
One, as shown here, is the dorsal supine lithotomy position in
which the legs are lowered in obstetrical stirrups so that the
hips are extended 10° rather than flexed and the knees
are flexed approximately 90°. The legs are abducted approximately
15°, exposing the vulva and perineum. This position is
preferable when a surgeon wishes to apply instruments to the
cervix and a cannula in the endometrial cavity during the procedure.
It allows injection of indigo carmine solution through the cervix
by means of a cervical cannula. In addition, the uterus can be
elevated into the appropriate operative position without using
traction sutures on the fundus or packing the cul-de-sac with
gauze. |
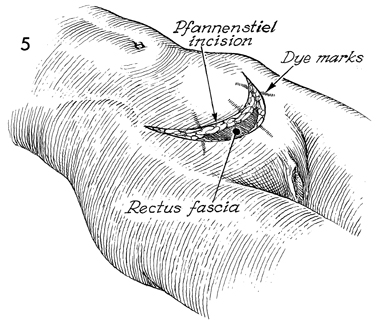
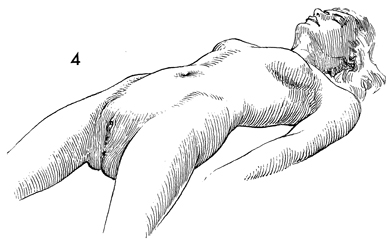
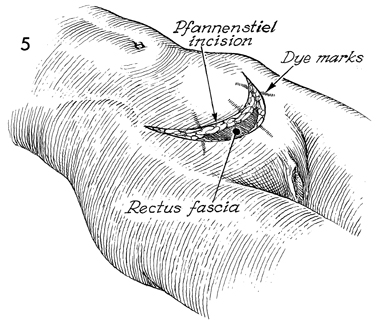
A Pfannenstiel incision is generally preferred
in these cases. Dye marks have been placed to aid closure of
the abdomen for a better cosmetic appearance. |
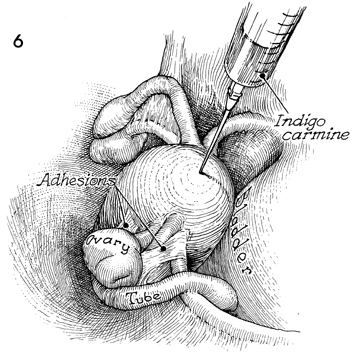
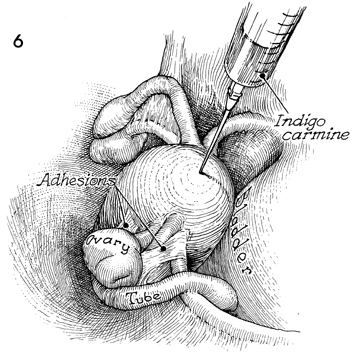
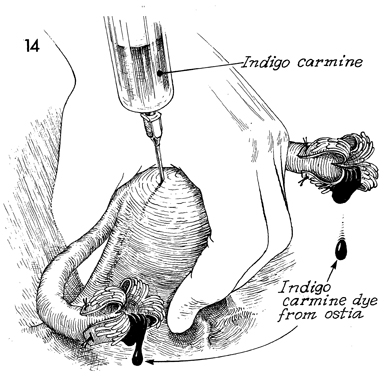
The abdomen has been opened
through the Pfannenstiel incision. Adhesions are found between
the Fallopian tube, ovary, and round ligament. The bladder is
on the right; the fundus is in the middle. An occlusive Buxton-type
clamp is applied to the lower uterine segment, and a 21-gauge
needle on a 10-mL syringe filled with indigo carmine solution
is inserted through the fundus. The endometrial cavity is filled
with the dye. This dye should spill into the Fallopian tubes
slightly distend the clubbed ends of the Fallopian tube that
requires a fimbrioplasty. |
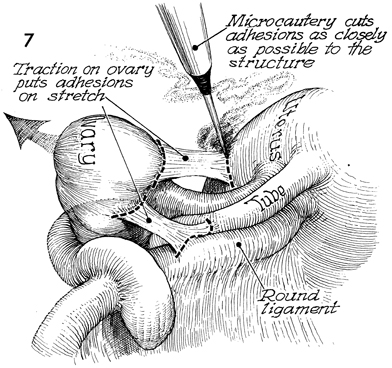
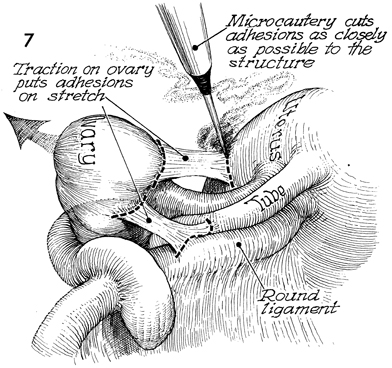
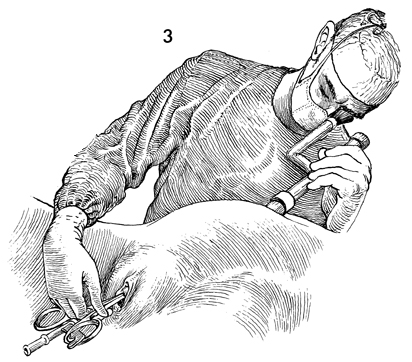
Moist packs have been placed in the cul-de-sac
to elevate the uterus, tubes, and ovaries into the incision.
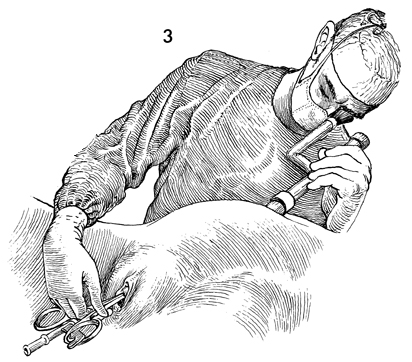
The microtip cautery is used to remove adhesions. Visual magnification
and a source of excellent light are essential if this step is
to be performed. The principle of traction/countertraction on
the structure is essential to safely demonstrate the adhesions. |
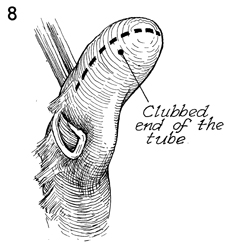
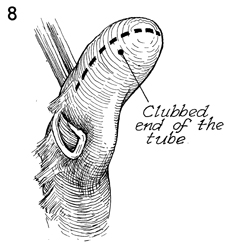
When the adhesions have been completely removed,
the clubbed end of the Fallopian tube can be identified; it should
be opened with the cautery on a low setting. Bright light and
visual magnification will aid the surgeon in performing this
delicate task. |
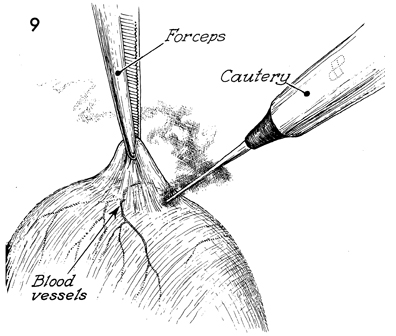
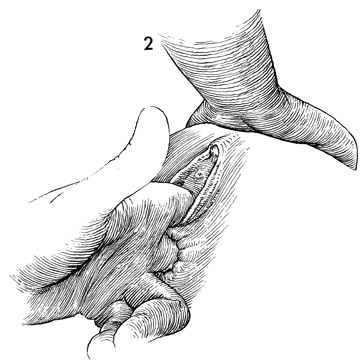
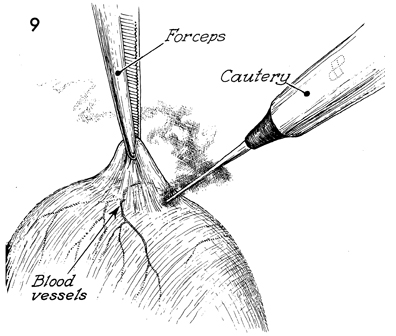
A microforceps is used to elevate the serosal
layer over the end of the clubbed Fallopian tube. Small vessels
are coagulated prior to opening the clubbed end of the fimbriae
with the microtip electrical cautery. When the scar tissue over
the clubbed end of the tube has been transected, indigo carmine
dye will be observed spilling from the Fallopian tube. |
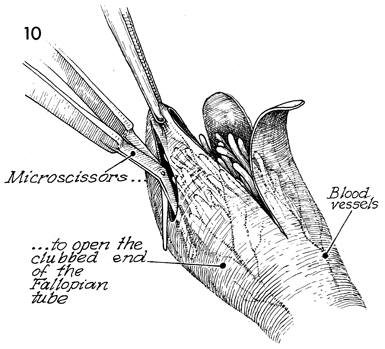
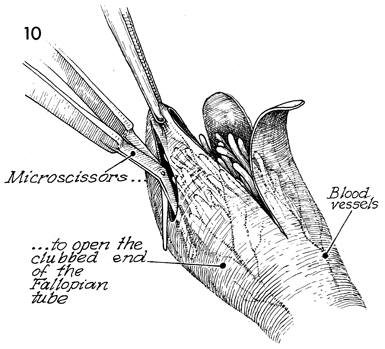
Microforceps and microscissors
are used to pick up the scar tissue and transect the scarred
serosal layer covering the fimbriae beneath. It is important
to identify the fine blood vessels in the scarred covering
of the fimbriae; the incisions into scarred serosa should be
tailored to transect as few of the blood vessels as possible.
Hemostasis is controlled with the microelectrode.
|
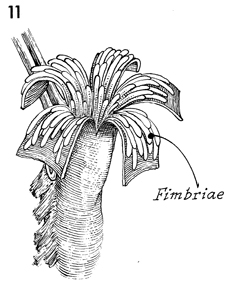
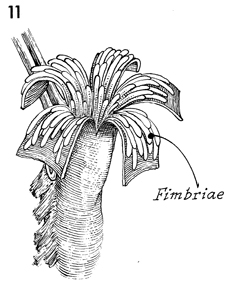
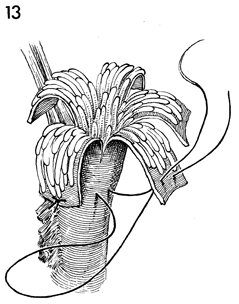
The scarred serosal covering of the clubbed
Fallopian tube has been opened, and when it is folded back, the
fimbriae should prolapse out of the Fallopian tube. |
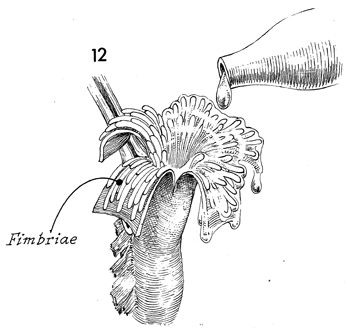
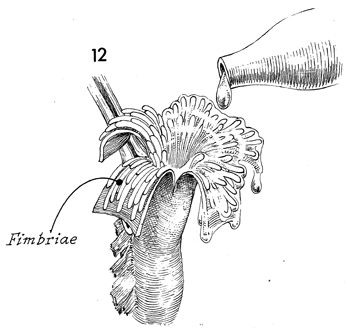
Irrigation with warm saline solution can
be used to separate the fimbriae and identify the lumen of the
ampullar portion of the Fallopian tube. |
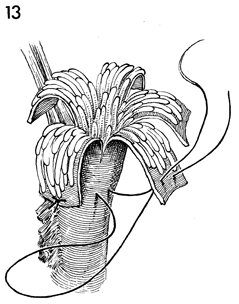
With 7-0 Prolene suture on a microneedle,
the scarred serosa is sutured back to the serosa of the Fallopian
tube in such a manner as to free the fimbriae and keep the Fallopian
tubes patent. |
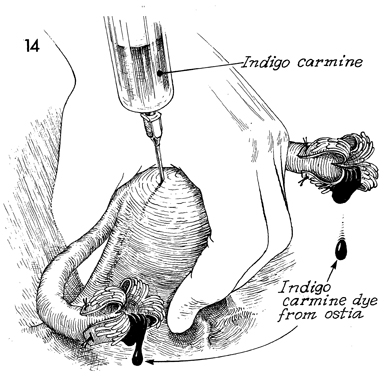
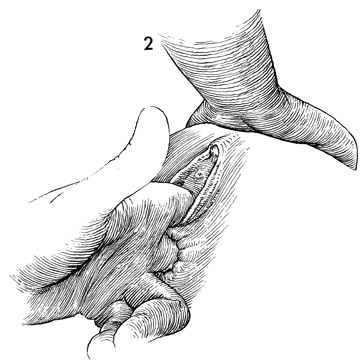
To check the patency of the Fallopian tubes,
the lower uterine segment is pinched between the thumb and first
finger or held with an atraumatic clamp, and a 10-mL syringe
on a 21-gauge needle is inserted through the fundus to inject
10 mL of indigo carmine into the endometrial cavity. The dye
should fill the Fallopian tubes and spill from the fimbriae. |
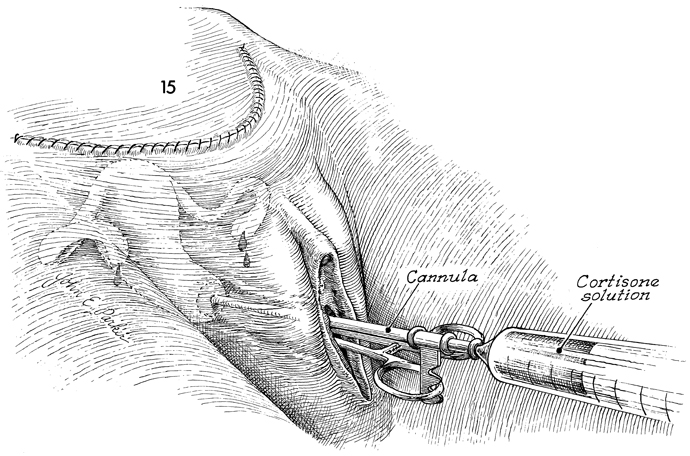
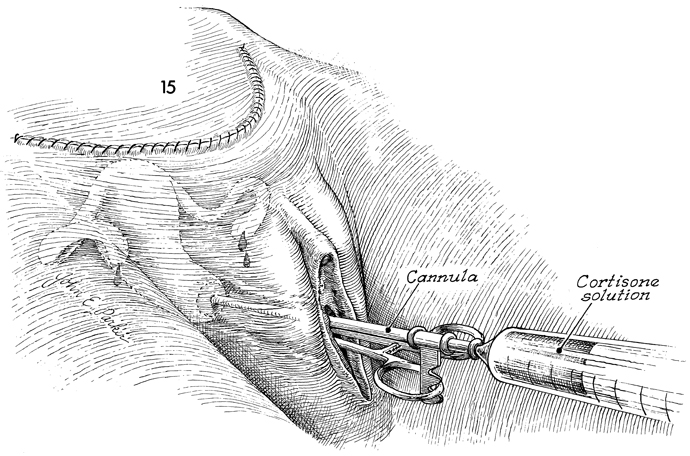
Hydrotubation should be performed every other
day for 2 weeks. A solution containing a broad spectrum antibiotic,
cortisone, and saline is injected through the cervix with a Rubin
cannula. |
|