Fallopian
Tubes
and Ovaries
Laparoscopy
Technique
Diagnostic
Uses
of Laparoscopy
Demonstration
of Tubal Patency
via Laparoscopy
Laparoscopic
Resection
of Unruptured
Ectopic Pregnancy
Ovarian
Biopsy
via Laparoscopy
Electrocoagulation
of
Endometriosis via
Laparoscopy
Lysis
or Adhesions
via Laparoscopy
Control
of Hemorrhage
During Laparoscopy
Fallopian
Tube
Sterilization
Sterilization
by
Electrocoagulation and
Division via Laparoscopy
Silastic
Band Sterilization
via Laparoscopy
Hulka
Clip Sterilization
via Laparoscopy
Sterilization
by the
Pomeroy Operation
Sterilization
by the
Modified Irving Technique
Sterilization
by the
Minilaparotomy Technique
Sterilization - Ucheda Technique
Salpingectomy
Salpingo-oophorectomy
Fimbrioplasy
Tuboplasty
-
Microresection
and Anastomosis
of the Fallopian Tube
Wedge
Resection
of the Ovary
Torsion
of the Ovary
Ovarian
Cystectomy |
Sterilization by Electrocoagulation
and Division via Laparoscopy
Electrocoagulation and division of peritoneal structures via the laparoscope
are facilitated if the surgeon achieves adequate displacement of the
intestine out of the pelvis, maintains a clear pneumoperitoneum free
of smoke, and ensures that the installation of the electrocoagulating
instrument is advanced sufficiently to prevent contact between the
instrument and the tip of the laparoscope. These principles are valid
whether performing sterilization, fulguration of endometrial implants,
biopsy of the ovary, or lysis of adhesions.
The purpose of the operation is to provide a simple method of female
sterilization by electrocoagulation of the Fallopian tube via the laparoscopic
technique.
Physiologic Changes. After the electrofulgurated
and divided tube heals, migrating spermatozoa should not be transported
through the Fallopian tube. Oocytes entering the distal end of the
tube should not pass the point of obstruction.
Points of Caution. The surgeon must
adhere to the points of caution noted for the laparoscopy technique
described in the section on Ovarian Biopsy by Laparoscopy.
There is
the additional risk with electrocoagulation of inadvertently burning
the intestine. Even with utmost care and attention to detail, the surgeon
cannot always prevent some electrocoagulation burns of the bowel. Care
should be taken, however, to ensure that the insulation on the grasping
forceps is well beyond the point of the metal trocar or laparoscope.
In addition, the structure being electrocoagulated should be moved
well away from the adjacent bowel or bladder.
Technique
Sterilization by electrocoagulation can be
achieved by either extensive electrocoagulation of the tube alone
or electrocoagulation and division. Experience has shown a lower
failure rate when the tube is electrocoagulated and divided.
Use of electrocoagulation and division increases the possibility
of hemorrhage from the mesosalpinx, however, if sufficient electrocoagulation
has not been performed prior to division of the tube. The uterus
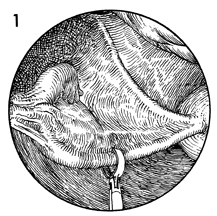
is markedly anteflexed and deviated to one side, placing the
tube on a slight stretch. The tube is grasped in the ischemial
portion approximately 3 cm from the cornua of the uterus. |
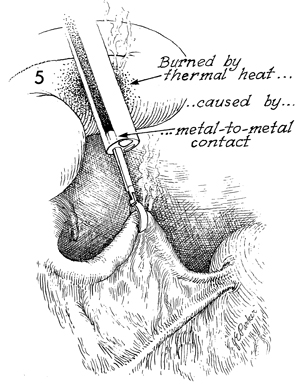
The tube is elevated and placed in a position
that is free from contact with bowel or bladder. |
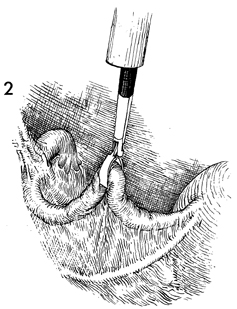
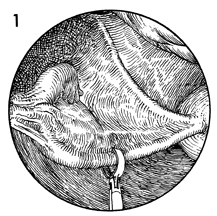
The electrocoagulation forceps is checked
to be sure that insulation is clearly visible and that the metal
grasping jaws of the coagulation forceps are not in contact with
the laparoscope or the trocar sleeve of the second-incision instrument.
The current is turned on, and the tube is thoroughly electrocoagulated
for at least 5 full seconds. Frequently, the tube will swell
and make a popping noise, indicating that fluid within the lumen
of the tube and tubal cells has reached the boiling point. The
burn will spread over a finite area, usually 3-4 cm along the
tube and 2 cm into the mesosalpinx. The burn will not spread
farther because burned tissue has greater resistance to the flow
of electrical current than does normal tissue. When the tube
has collapsed from its swollen state, it has been coagulated
sufficiently. |
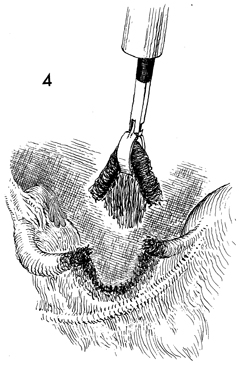
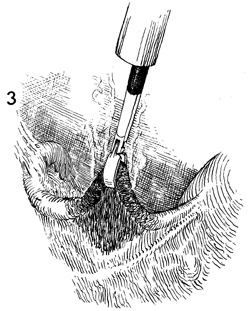
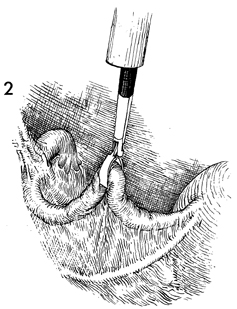
At this point, the tube is
avulsed off the mesosalpinx and from its connection to the proximal
and distal tube. This is facilitated by shearing the tube against
the operative port of the laparoscope. The reduced tensile strength
of the burned tube has little resistance to the tearing motion
of the grasping forceps.
|
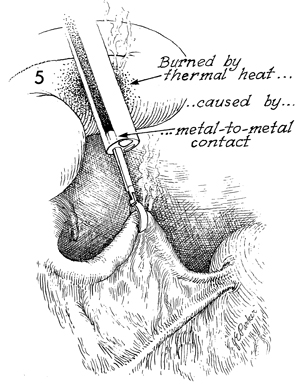
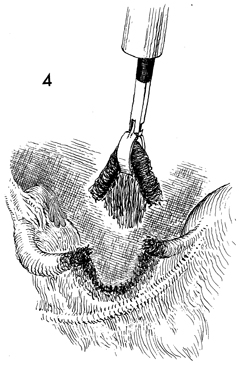
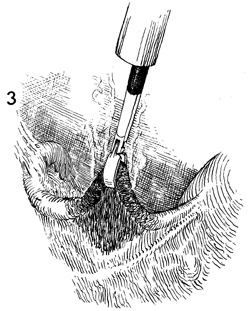
Care should be taken to ensure that insulation
is showing through the laparoscope at all times. It is a mistake
for the metal of the grasping forceps to make contact with the
metal end of the laparoscope. This may allow the electrothermal
energy to flow up the shaft of the laparoscope and may produce
a burn of the intestine higher in the abdomen. |
|
|