Ovarian cystectomy is performed in those benign conditions of the
ovary in which a cyst can be removed and when it is desirable to leave
a functional ovary in place. This is particularly true in women of
reproductive age. Pelvic surgeons continue to be amazed at how much
function remains in the smallest segment of healthy ovarian tissue.
Therefore, if it is technically feasible and where one is assured that
there is no malignant tissue present, it behooves those performing
pelvic surgery to attempt to perform ovarian cystectomy in preference
to oophorectomy, particularly in those patients who want to become
pregnant.
The purpose of the operation is to excise an ovarian cyst without removing
the ovary.
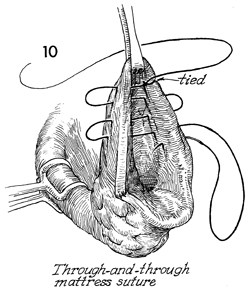
Meticulous hemostasis must be achieved to avoid ovarian hematoma. This
is best performed with a running mattress suture as shown in Figures
10-12.

Patients with an adnexal mass should be placed
on the operating table in the dorsal lithotomy position. A thorough
examination under anesthesia is performed prior to opening the
abdomen. The bladder should be emptied with a catheter. The surgeon
should not be surprised to see a patient who has been referred
for ovarian cyst who actually has a problem with urinary retention.
The abdomen, perineum, and vagina
are surgically prepared. Although hysterectomy is rarely required,
a malignancy can occasionally be encountered that will necessitate
removal of the uterus. For this reason, it is best to have previously
prepared the vagina with an aseptic soap solution. |
The patient can be changed to the supine
position or to the modified dorsal lithotomy position.
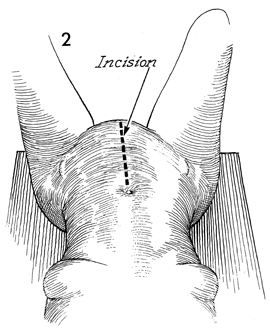
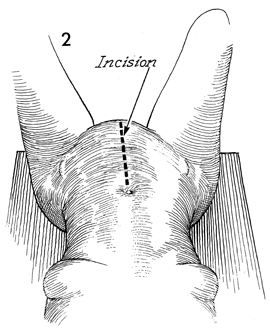
In general, a patient of menopausal
age or above should have a lower midline incision for adnexal
masses. The incidence of malignant disease is such that a lower
midline incision will be required in the course of surgery, and
this overrides the cosmetic advantages of a transverse incision.
It is extremely difficult to adequately explore the abdomen for
a malignant ovarian process through a Pfannenstiel or transverse
incision. For younger patients in whom the chance of a malignant
disease is quite low, a transverse incision or Pfannenstiel incision
is acceptable. If a malignant disease is encountered in this
younger age group, the transverse or Pfannenstiel incision can
be closed and a midline incision can be made. |
A
lower midline incision is made.
|
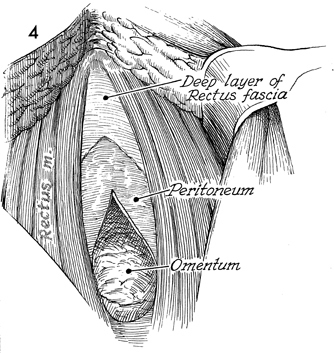
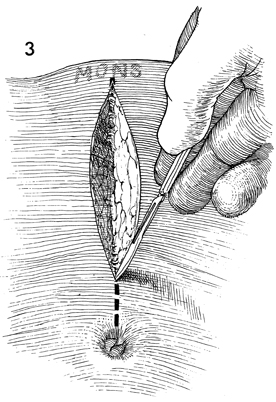
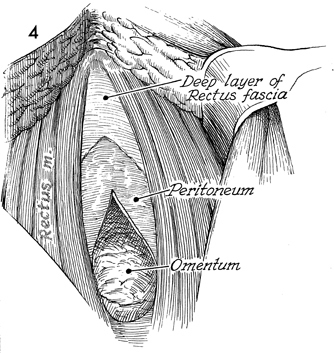
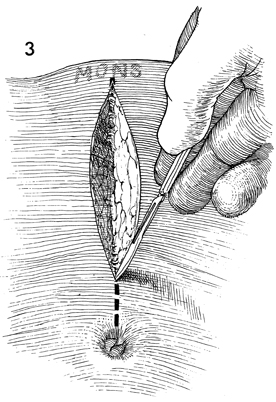
The peritoneum is opened. The
abdomen is thoroughly explored. Any suspicious tissue in the
upper abdomen or along the aortic lymph nodes should be sent
for a frozen section pathologic analysis. |
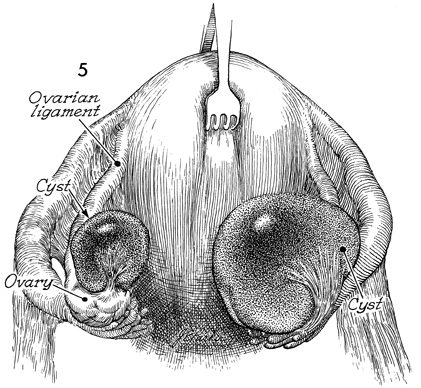
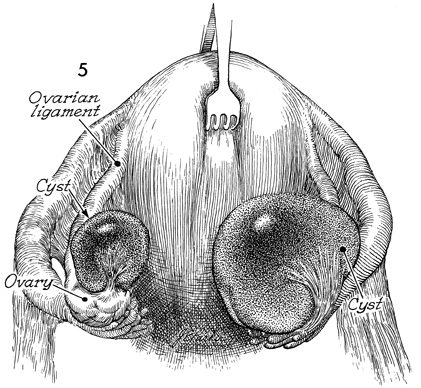
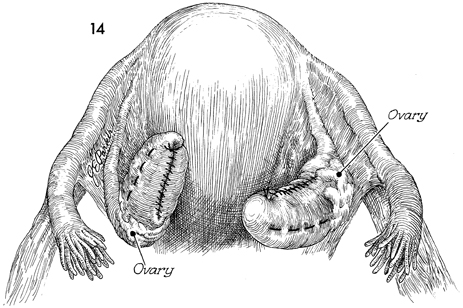
A uterine elevator or a suture is placed
in the fundus of the uterus to retract it anteriorly. Bilateral
cysts are shown here: the one on the left appears to be more
polypoid; the one on the right appears to be involved with significant
amount of ovarian tissue. |
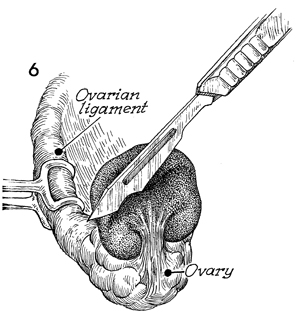
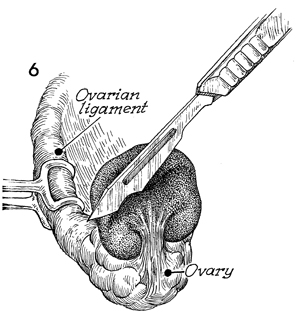
The ovary is anchored by
placing Babcock clamps on the suspensory ligament of the ovary.
A scalpel is used to incise the ovarian capsule near the base
of the cyst. |
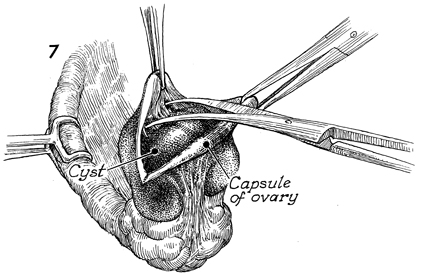
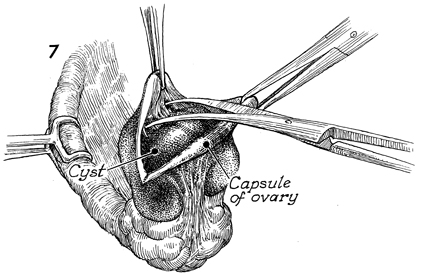
After incising the ovarian capsule with a
scalpel, the surgeon uses delicate tissue forceps to elevate
the capsule and small Metzenbaum scissors to dissect the alveolar
tissue between the cyst and the ovarian capsule. |
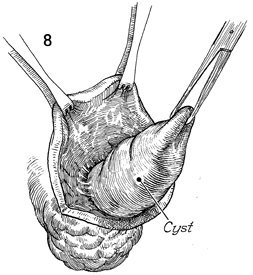
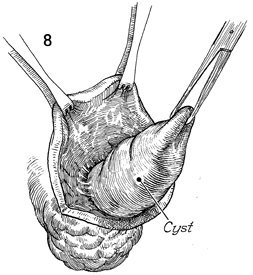
The margins of the ovarian capsule
are held with Allis clamps. An adhesion on the cyst can be used
to provide retraction, and the remaining cyst can be dissected
out of the ovary with Metzenbaum scissors. |
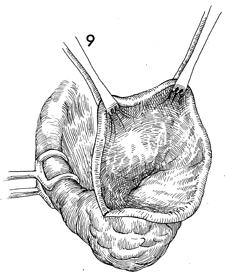
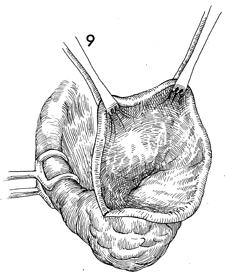
The ovarian capsule and base of the ovary
are shown after the cyst has been removed. Hemostasis within
the bed of the ovary can be controlled by clamping and electrocoagulating
small bleeders. |
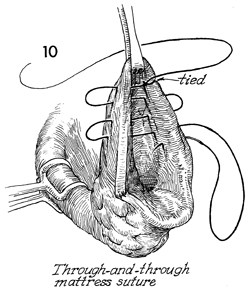
The hemostatic running mattress suture is
placed with a 3-0 synthetic absorbable suture starting at the
upper pole where the suture is tied. |
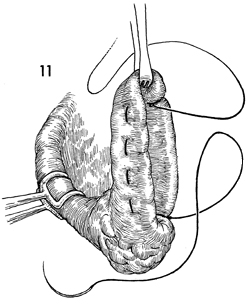
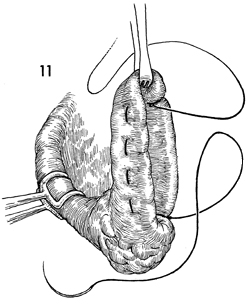
The mattress suture of the ovary has been
completed. |
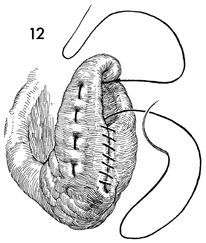
When the lower pole of the ovary has been
reached, the same suture is used to suture the edges of the ovary
in a running Connell inverting suture. |
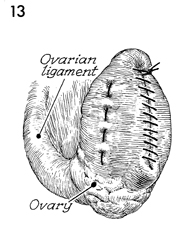
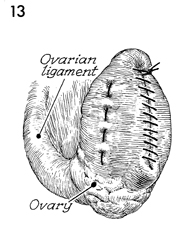
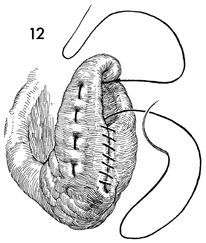
The completed operation is shown. |
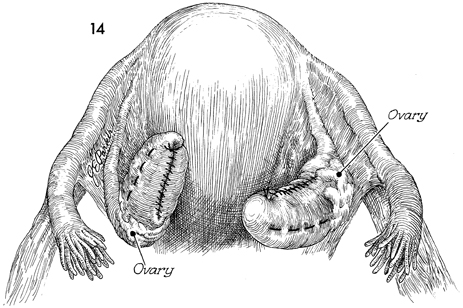
Both ovarian cysts have been removed with
the ovaries intact. The abdomen is closed in layers. |