![]()
Directed Biopsy of the Cervix at Colposcopy
Endocervical Curettage at Colposcopy
Conization of the Cervix by the Loop Electrical Excision Procedure (LEEP)
Abdominal Excision of the Cervix Stump
Correction of an Incompetent Cervix by the Shirodkar Technique
Correction of an Incompetent Cervix by the McDonald Operation
Conization of Cervix
The indications for conization of the cervix are: (1) an abnormal Papanicolaou smear when the limits of the lesion either cannot be completely defined by colposcopy and directed biopsy or when the lesion is noted to extend up into the cervical canal and, therefore, is inaccessible to histologic examination by directed biopsy, and (2) severe cervical intraepithelial neoplasia or in situ carcinoma in young patients for whom hysterectomy is initially contraindicated because of age.
The purpose of conization of cervix is to remove a cone-shaped piece of cervical tissue that will encompass the squamocolumnar junction and, therefore, be diagnostic as well as therapeutic.
Pathophysiologic Changes: This operation does remove endocervical glands and, in some instances, has been associated with infertility because it may reduce the production of cervical mucus. In addition, it sometimes weakens the internal os of the cervix and is therefore associated with second trimester abortion or it can be associated with scarring of the cervix causing a failure to progressively dilate with labor and therefore be associated with an increased risk of Cesarian section.
Points of Caution: The surgical specimen should be adequate to provide an accurate diagnosis and, in addition, remove the entire area of cervical intrepithelial neoplasia.
Hemostasis is essential.
These patients should be informed there is a small incidence of persistent cervical intraepithelial neoplasia following conization. Follow up visits are essential.
Technique
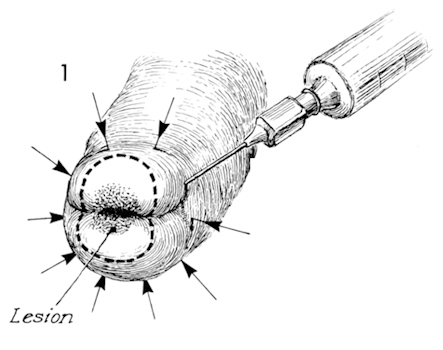
The patient is given general anesthesia and adequate exposure of the cervix is obtained. The cervix is then stained with Lugol's solution to completely define all areas failing to take up the iodine agent and, thereby, demarcate zones of glycogen depletion. Xylocaine 1% with epinephrine is injected around the entire surface of the cervix. Vascular constriction and blanching of the cervix will be noted. This technique may be contraindicated in patients with cardiovascular disease and / or hypertension.
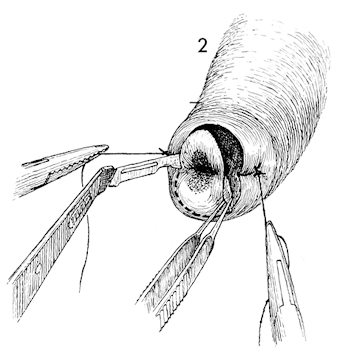
Hemostatic retraction sutures are placed at 3 and 9 o'clock at the junction of the portio and the vagina, deep enough to suture ligate the descending cervical branch of the uterine artery. These sutures are held on traction to eliminate the need for placing tenaculae on the cervix which may disrupt the continuity of the cervical epithelium. A scalpel mounted on a knife handle bent at a 45 degree angle is used to excise the cone-shaped biopsy. The initial stab of the knife blade should be made between 5 and 6 o'clock to allow blood to run down into the vagina and not obscure the line of incision. Fine-toothed forceps are used to elevate the cone away from it's incised bed to avoid damaging the cervical epithelium. Contrary to some authorities in the field, we feel that a "jigsaw cutting technique" is superior to a continuous cutting. All too often cutting leads to accidental slippage and laceration of the cervix and vagina.
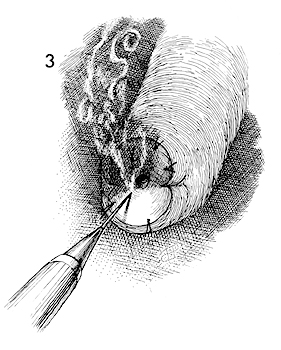
We do not use the Sturmdorf suture technique as we feel this may cover up cervical intraepithelial neoplasia left in some patients. Instead, we have preferred individual suture ligatures to control bleeding and occasional electrocoagulation of small bleeders.
Postoperative hemorrhage rarely occurs with this technique. However, when it does, a collagen hemostatic with a gauze pack placed against the cervix is used.
After the cone has been removed, it is opened at 12 o'clock and mounted on a cork block with the epithelial side up. It is dropped into formalin solution to allow fixation of the cervical epithelium and orientation of the specimen by the pathologist.