Uterus
Dilatation
and Curettage
Suction
Curettage
for Abortion
Management
of Major
Uterine Perforations
From Suction Curet or
Radium Tandem
Cesarean
Section
Myomectomy
Jones
Operation
for Correction of
Double Uterus
Hysteroscopic
Septal
Resection by Loop
Electrical Excision
Procedure (LEEP) for
Correction of a Double
Uterus
Manchester
Operation
Richardson Composite Operation
Total
Vaginal Hysterectomy
Total
Abdominal
Hysterectomy With
and Without Bilateral
Salpingo-oophorectomy
Laparoscopy-Assisted
Vaginal Hysterectomy |
Total Abdominal Hysterectomy
With and Without Bilateral
Salpingo-oophorectomy
Total abdominal hysterectomy is utilized for benign
and malignant disease where removal of the internal genitalia is indicated.
The operation can be performed with the preservation or removal of
the ovaries on one or both sides. In benign disease, the possibility
of bilateral and unilateral oophorectomy should be thoroughly discussed
with the patient. Frequently, in malignant disease, no choice exists
but to remove the tubes and ovaries, since they are frequent sites
of micrometastases.
In general, the modified Richardson technique of
intrafascial hysterectomy is used.
The purpose of the operation is to
remove the uterus through the abdomen, with or without removing the
tube and ovaries.
Physiologic Changes. The predominant physiologic
change from removal of the uterus is the elimination of the uterine
disease and the menstrual flow. If the ovaries are removed with the
specimen, the predominant physiologic change noted is loss of the ovarian
steroid sex hormone production.
Points of Caution. The predominant
point of caution in performing abdominal hysterectomy is to ensure
that there is no damage to the bladder, ureters, or rectosigmoid colon.
Mobilization
of the bladder with a combination of sharp and blunt dissection frees
the bladder from the lower uterine segment and upper vagina. This reduces
the incidence of damage to the bladder.
By exercising extreme care in
management of the uterine artery pedicle, the surgeon may minimize
the risk of injury to the ureter. The same is true of the management
of the cardinal and uetrosacral ligament pedicles.
If the vaginal cuff
is left open with the edges sutured, the incidence of postoperative
pelvic abscess is dramatically reduced.
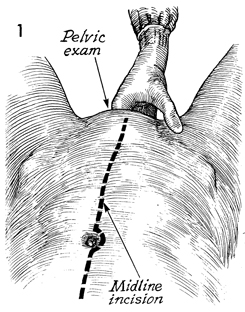
Technique
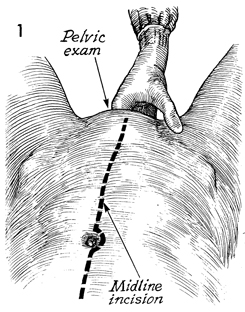
The patient is placed in the
dorsal lithotomy position, and an adequate pelvic examination
is performed with the patient under general anesthesia. This
is extremely important because it allows the surgeon to become
acquainted with the anatomy of the internal genitalia. This is
frequently impossible when the patient is examined in the gynecologic
clinic. The patient is then put in approximately a 15° Trendelenburg position. A Foley catheter is left in the bladder
and connected to straight drainage. In general, midline incisions
are preferred for malignant disease, since they allow accurate
staging and exposure to the upper abdomen and aortic lymph nodes.
If investigation of the upper abdomen and aortic lymph nodes
is needed, the midline incision should be extended around and
above the umbilicus for appropriate exposure.
For benign disease, the Pfannenstiel
incision is an adequate alternative to the midline incision.
After the abdomen is entered, it should be thoroughly explored; including the
liver, gallbladder, stomach, kidneys, and aortic lymph nodes. |
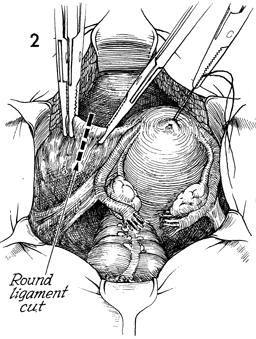
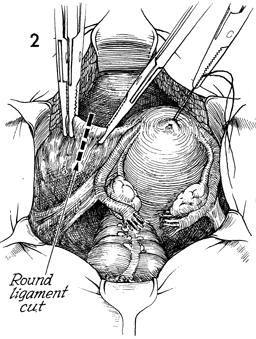
Self-retaining retractors are
placed in the abdominal incision, and the bowel is packed off
with warm, moist gauze packs. A 0 synthetic absorbable suture
is placed in the fundus of the uterus and used for uterine traction.
The uterus is deviated to the patient's right. The left round
ligament is placed on stretch and incised between clamps. |
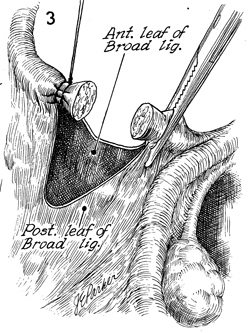
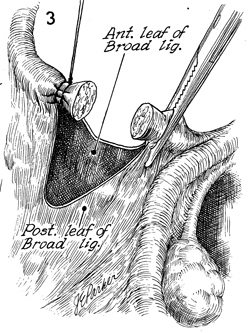
The distal stump of the round ligament is
ligated with 0 synthetic absorbable suture. The proximal stump
is held with a straight Ochsner clamp. At this point the leaves
of the broad ligament are opened both anteriorly and posteriorly.
This is performed by delicate dissection with the Metzenbaum
scissors. |
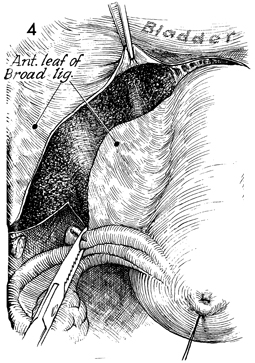
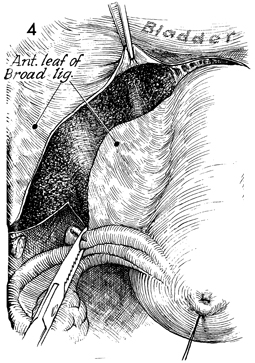
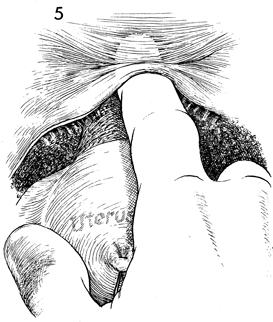
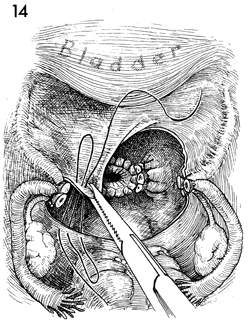
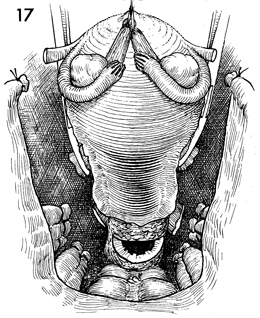
While retracting the uterus
cephalad, the surgeon opens the anterior lead of the broad ligament
to the vesicouterine fold. Steps 2-4 are carried out on the opposite
side. |
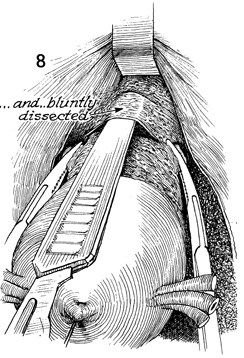
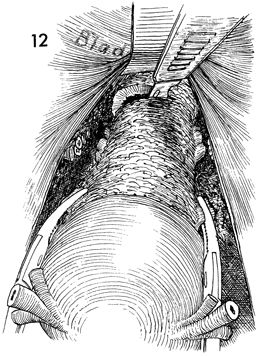
The vesicoperitoneal fold is elevated, and
the fine filmy attachments of the bladder to the pubovesical
cervical fascia are visible. The bladder can be dissected off
the lower uterine segment of the uterus and cervix by either
blunt or sharp dissection. If there has been extensive lower
segment disease, previous cesarean sections, or pelvic irradiation,
blunt dissection of the bladder off the cervix is dangerous,
and a sharp dissection technique should be performed. |
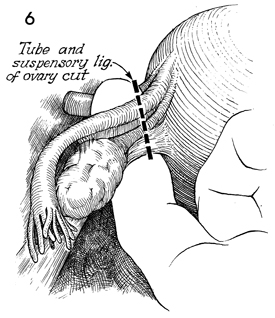
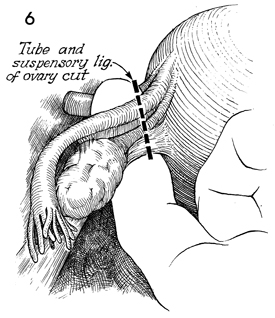
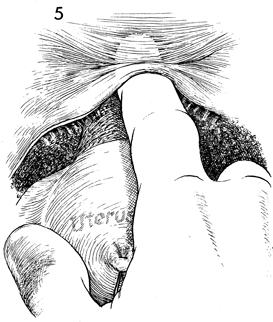
If the ovaries are to be
preserved, the uterus is retracted toward the pubic symphysis
and deviated to one side with the infundibulopelvic ligament,
tube, and ovary on tension. A finger should be inserted through
the peritoneum of the posterior leaf of the broad ligament under
the suspensory ligament of the ovary and Fallopian tube. The
tube and suspensory ligament are doubly clamped, incised, and
tied with 0 synthetic absorbable suture. The distal stump of
this structure is best doubly tied, first with a single tie of
0 synthetic absorbable suture and then with a ligature of 0 synthetic
absorbable suture. The same procedure is carried out on the opposite
side. |
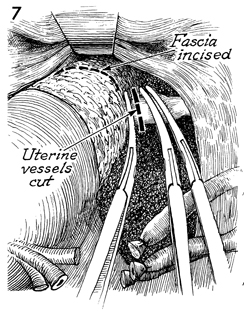
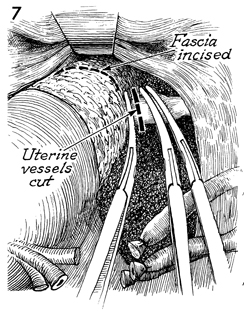
The uterus is then retracted cephalad and
deviated to one side of the pelvis with the lower broad ligament
on stretch. The filmy tissue surrounding the uterine vessels
is skeletonized by elevating the round ligament and dissecting
the tissue away from the uterine vessels. Three curved Ochsner
clamps are placed at the junction of the lower uterine segment
on the uterine vessels. This is best performed by placing the
tips of the curved Ochsner clamps onto the uterus and allowing
them to slide off the body of the uterus, thus ensuring complete
clamping of the uterine vessels. An incision is made between
the upper Ochsner clamp and the two lower Ochsner clamps. This
is suture-ligated with two 0 synthetic absorbable sutures, placing
the first suture at the tip of the lower Ochsner clamp and tying
the suture behind the base of the clamp. The middle Ochsner clamp
is left in place and is similarly suture-ligated by a second
ligature placed at the tip of the Ochsner clamp and tied behind
the base of the clamp. No attempt is made to place a suture in
the middle of the pedicle, since it contains blood vessels and
a pedicle hematoma can be created.
The same procedure is carried
out on the opposite side.
A delicate, transverse, curved
incision is made in the pubovesical cervical fascia overlying
the lower uterine segment. The separation of the pubovesical
cervical fascia from the underlying cervical stroma is facilitated
by placing traction on the uterus in the cephalad position. |
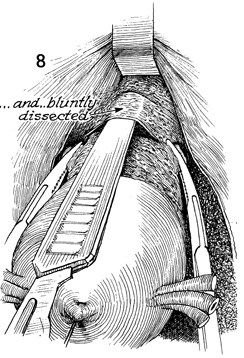
The uterus is held in traction in the cephalad
position, and the handle of the knife is used to dissect the
pubovesical cervical fascia inferiorly. This step mobilizes the
ureter laterally and caudally. |
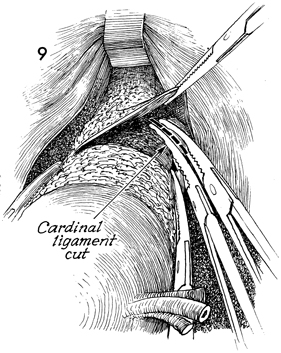
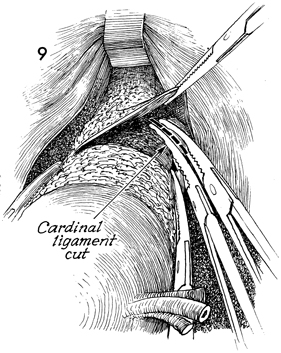
Two straight Ochsner clamps are applied to
the cardinal ligament for a distance of approximately 2 cm. The
cardinal ligament is incised between the two clamps, and the
distal stump is ligated with 0 synthetic absorbable suture. The
suture is tied at the base of the clamp; no attempt is made to
place this suture within the body of the pedicle because vessels
can be torn and hematomas created.
The same procedure is carried
out on the opposite cardinal ligament. |
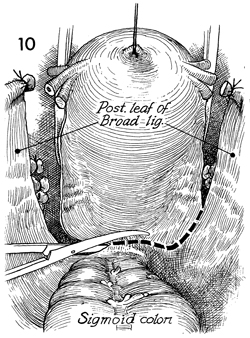
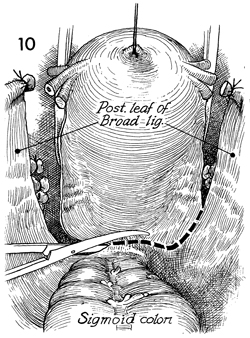
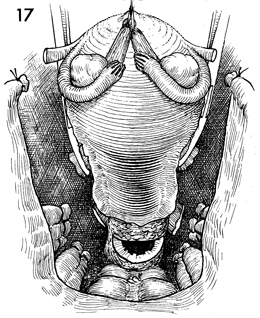
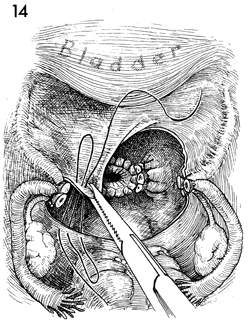
The posterior leaf of the broad ligament
is incised down to the uterosacral ligaments and across the posterior
lower uterine segment between the rectum and cervix. |
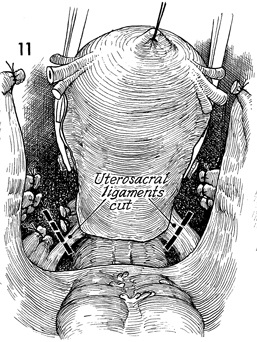
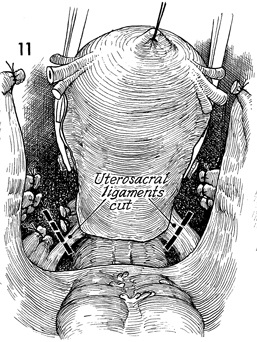
The uterosacral ligaments on both sides are
clamped between straight Ochsner clamps, incised, and ligated
with 0 synthetic absorbable suture. |
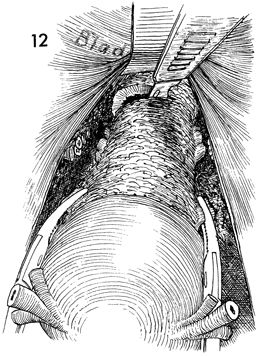
The uterus is placed on traction
cephalad, and the lower uterine segment and upper vagina are
palpated between the thumb and first finger of the surgeon's
hand to ensure that the ligaments have been completely incised.
The vagina is entered by a stab wound with a scalpel and is cut
across with either a scalpel or scissors. The uterus is removed.
The edges of the vagina are picked up with straight Ochsner clamps
in a north, south, east, and west direction. |

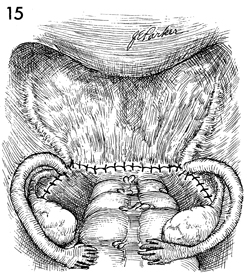
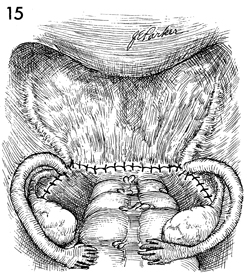
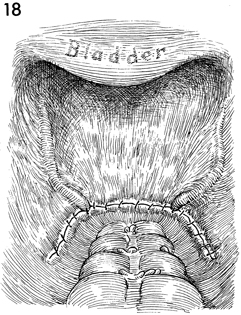
a. The vaginal cuff is never
closed in our clinic. This alone has accounted for a radical
decrease in postoperative febrile morbidity and abscess formation.
The edges of the vaginal mucosa are sutured with a running locking
0 synthetic absorbable suture starting at the midpoint of the
vagina underneath the bladder and carried around to the stumps
of the cardinal and uterosacral ligaments, which are sutured
into the angle of the vagina.
b. The running
locking suture is carried around the posterior wall of the vagina
ensuring that the rectovaginal space is obliterated.
c. The cardinal
and uterosacral ligaments of the opposite side have been included
in the running locking 0 synthetic absorbable suture, and the
reefing process has been completed to the midpoint of the anterior
vaginal wall. At this point, meticulous care should be taken
to ensure that the lateral angle of the vagina is adequately
secured and that hemostasis is complete between the lateral angle
of the vagina and the stumps of the cardinal and uterosacral
ligaments. This can be a site of hemorrhage.
At this point,
the pelvis is thoroughly washed with sterile saline solution.
Meticulous care is taken to ensure that hemostasis is present
throughout the dissected area. |
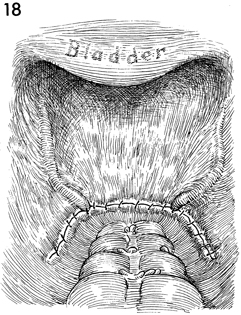
The pelvis is reperitonealized with running
2-0 synthetic absorbable suture from the anterior to the posterior
leaf of the broad ligament. The stumps of the tubo-ovarian round,
suspensory ligament of the ovary, and the cardinal and uterosacral
ligaments are buried retroperitoneally. |
Drains are rarely needed. If they are indicated,
they are placed through the open vaginal cuff and carried along
the lateral pelvic wall retroperitoneally. |
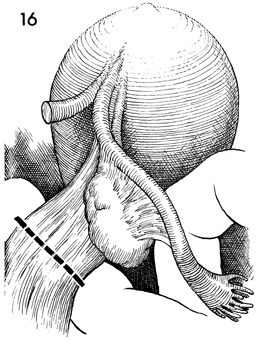
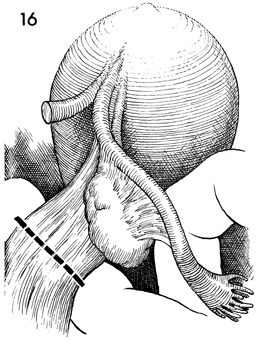
If the tube and ovary are to be removed,
they are removed at Step 6 in the operation. Instead of placing
a finger underneath the tube and suspensory ligament of the ovary,
a finger is placed under the infundilbulopelvic ligament on that
side. Care is taken to ensure that the ureter is not included.
In various forms of pelvic disease (endometriosis, pelvic inflammatory
disease, etc.), the ureter can be deviated close to the infundibulopelvic
ligament.
The infundibulopelvic ligament
is doubly clamped and incised, and the distal stump of the ligament
is doubly ligated with a tie of 0 synthetic absorbable suture
plus a ligature of 0 synthetic absorbable suture.
For a bilateral
salpingo-oophorectomy, the same procedure is carried out on the
opposite infundibulopelvic ligament. |
The tube and ovary have been mobilized medially
with the uterine specimens. The remainder of the operation is
carried out as described in Steps 7-13. |
The peritoneum of the pelvis has been reestablished
with the tube and ovary removed. The stump of the infundibulopelvic
ligament is buried retroperitoneally.
Postoperatively, no vaginal packing is left in
the vagina, and no Foley catheter drainage of the bladder is indicated.
The open vaginal cuff closes without
difficulty. Rarely, a small bit of granulation tissue is noted
in the upper vagina and is adequately treated by application of
silver nitrate 4 weeks postoperatively in the clinic or office.
The patient is allowed to resume sexual intercourse 4 weeks after
examination in the clinic and is allowed to resume work 5 weeks
postoperatively. |
|