Uterus
Dilatation
and Curettage
Suction
Curettage
for Abortion
Management
of Major
Uterine Perforations
From Suction Curet or
Radium Tandem
Cesarean
Section
Myomectomy
Jones
Operation
for Correction of
Double Uterus
Hysteroscopic
Septal
Resection by Loop
Electrical Excision
Procedure (LEEP) for
Correction of a Double
Uterus
Manchester
Operation
Richardson Composite Operation
Total
Vaginal Hysterectomy
Total
Abdominal
Hysterectomy With
and Without Bilateral
Salpingo-oophorectomy
Laparoscopy-Assisted
Vaginal Hysterectomy |
Total Vaginal Hysterectomy
Total vaginal hysterectomy is an excellent operation
when removal of the uterus is indicated in cases of either benign disease
or carcinoma in situ of the cervix. The technique described here is
simple and easy and can be accomplished with a minimum of operative
time. There are four basic steps involved in performing a vaginal hysterectomy:
(1) entrance into the anterior and posterior cul-de-sac to expose the
broad ligament, (2) progressive clamping of the broad ligament from
the uterosacral cardinal ligament to the tubo-ovarian round ligament,
(3) suspension of the vaginal cuff by suturing it to the uetrosacral
cardinal ligament, and (4) plication of the uterosacral ligaments in
the midline to obliterate the cul-de-sac and reduce the chances of
enterocele. The vaginal cuff can be progressively suspended as the
hysterectomy takes place rather than suspended separately at the end
of the hysterectomy. There are four separate sutures that help suspend
the vaginal cuff: (1) the initial suture into the uterosacral
cardinal ligaments, (2) the pursestring reperitonealization suture
that reinforces the uterosacral cardinal vaginal cuff suture, (3) the
vaginal cuff reefing suture, and (4) the uterosacral ligament sutures
tied across the midline at the end of the procedure.
The purpose of the operation
is to remove the uterus via the vagina.
Physiologic Changes. Removal
of the uterus results in the cessation of menstrual flow and causes
sterility. In addition, it eliminates any existing cervical or uterine
disease.
Points of Caution. Care must be taken to ensure that
entry into the anterior cul-de-sac is made before the uterus is totally
removed to avoid accidental entry into the bladder.
If the anterior and posterior cul-de-sacs can be entered, there is
a significant reduction in bleeding from the pedicles of the clamped
broad ligament.
The pedicles of the broad ligament should be retroperitonealized
before reefing the vaginal mucosa.
The vaginal mucosa should not be closed. the edges of the vaginal mucosa
should be reefed with a running locking 0 synthetic absorbable suture
and left open for drainage.
Technique
After appropriate general anesthesia,
the patient is placed in the dorsal lithotomy position with the
buttocks well off the end of the table. A thorough bimanual examination
is necessary prior to performing a hysterectomy. The vulva and
vagina are fully prepped with a surgical soap solution. The cervix
is exposed by placing a weighted posterior vaginal retractor into
the vagina. A small right-angle retractor is used to elevate the
anterior vaginal wall; a second right-angle retractor displaces
one lateral vaginal wall and exposes the cervix. Two Jacobs tenacula
are used to grasp the anterior and posterior lips of the cervix
and pull them into the vaginal introitus.
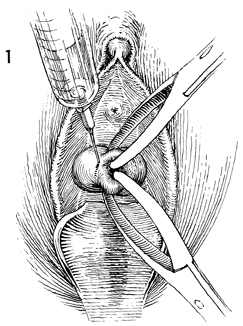
The vaginal mucosa at its junction
to the cervix is being injected with a dilute solution of Pitressin.
Ten international units of Pitressin are diluted with 25 mL of
sterile saline solution, and 10 mL of this mixture are injected
into the vaginal mucosa to aid hemostasis. This solution should
not be used on patients with hypertension or cardiac arrhythmias
but is most useful in healthy premenopausal patients. |
After the injection of Pitressin into
the vaginal mucosa, the mucosa is incised with a scalpel around
the entire cervix. The incision should stay above the pubovesical
cervical fascia anteriorly and the perirectal fascia posteriorly. |
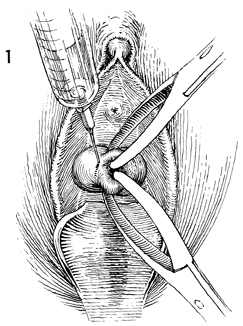
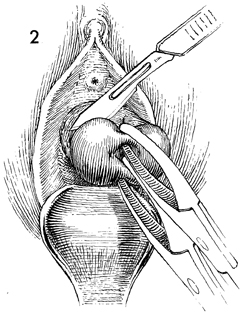
While downward traction is applied
on the Jacobs tenacula, the handle of the knife is used to dissect
the bladder off the anterior lower uterine segment. |
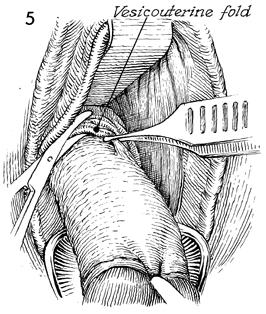
A sponge-covered finger dissects the
bladder all the way up to the peritoneal vesicouterine fold. This
step is frequently insufficiently performed for fear of entering
the bladder. If dissection is not carried up to the peritoneal
vesicouterine fold, entry into the anterior cul-de-sac is most
difficult. |
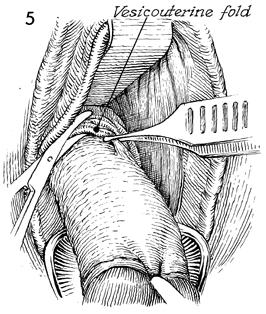
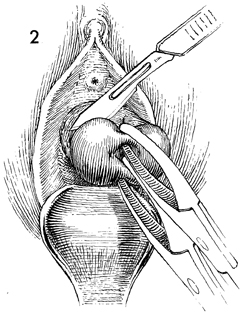
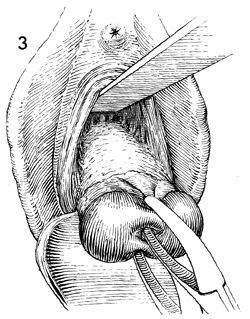
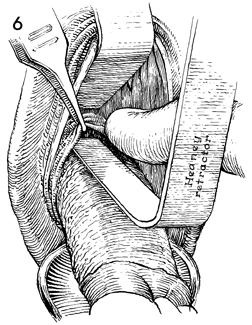
A right-angle retractor is placed
under the vaginal mucosa and bladder. It is used to elevate the
bladder. This maneuver aids in identifying the peritoneal vesicouterine
fold. The peritoneal fold appears as a white transverse line across
the lower uterine segment. Strong downward traction is applied
to the Jacobs tenacula on the cervix, and the peritoneal vesicouterine
fold is grasped with pickup forceps and incised with sharp curved
Mayo scissors. |
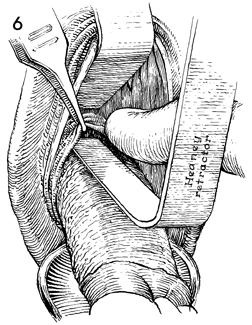
By elevating
the peritoneal vesicouterine fold with the pickup forceps, a
definite hole can be seen. It is advisable to insert a finger
in this hole and explore the area (1) to be sure one is in the
peritoneal cavity and not the bladder and (2) to uncover any
unsuspected pathologic condition that was not identified during
the examination. With the finger remaining in the hole, an anterior
Heaney right-angle retractor is placed into the defect underneath
the finger. |
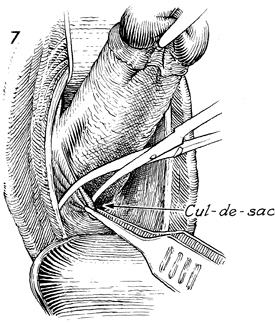
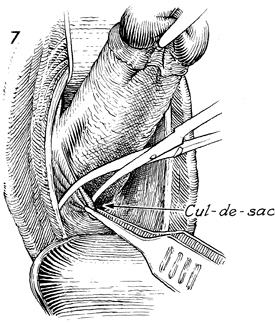
The Jacobs tenacula are brought acutely
up toward the pubic symphysis, exposing the cul-de-sac. Pickup
forceps are used to retract the posterior vaginal cuff, thereby
placing the peritoneum of the cul-de-sac on tension. The peritoneum
of the cul-de-sac is incised with curved Mayo scissors. |
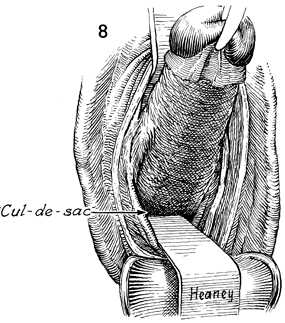
A finger is immediately placed
in the cul-de-sac, and the area is explored as in the exploration
of the anterior cul-de-sac. Approximately 75-100 mL of peritoneal
fluid may be seen upon opening the cul-de-sac. A second
right-angle Heaney retractor is placed into the posterior cul-de-sac. |
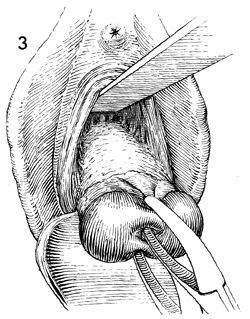
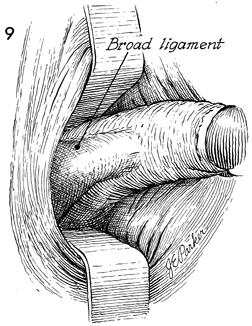
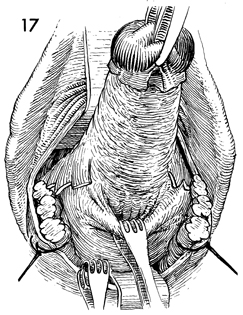
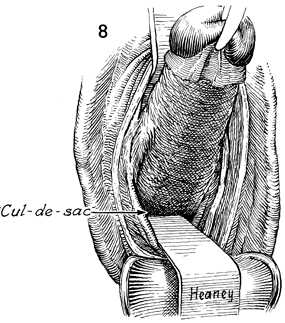
The weighted posterior vaginal retractor
is removed. With the two Heaney retractors the broad ligament is
exposed from the uetrosacral ligament to the tubo-ovarian round
ligament. A finger placed in the posterior cul-de-sac and moved
laterally reveals the uterosacral ligament as it attaches to the
lower uterine segment. |
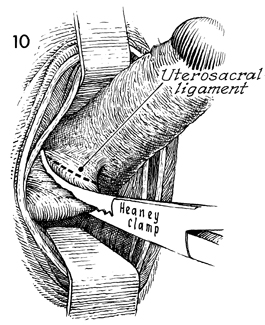
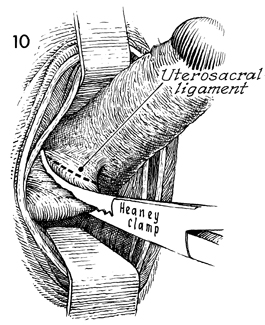
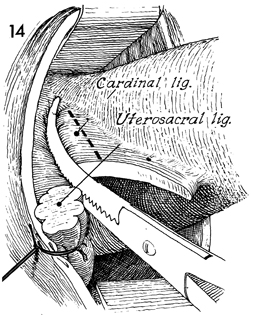
With the cervix on upward and lateral
retraction via the Jacobs tenacula, a curved Heaney clamp is placed
in the posterior cul-de-sac with one blade underneath the uterosacral
ligament and the opposite blade over the uterosacral ligament.
The clamp is placed immediately next to the uterine cervix so that
some tissue of the cervix is included in this clamp. This is done
to prevent possible ureteral damage from clamping the uterosacral
ligament in the lateral position. |
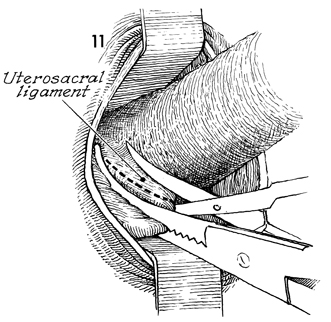
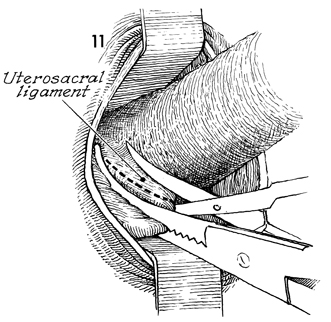
The uterosacral ligament is cut with
curved Mayo scissors. |
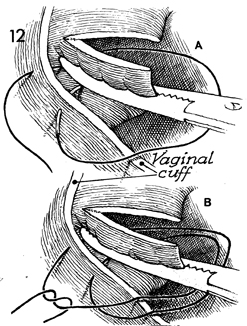
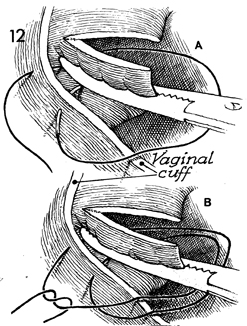
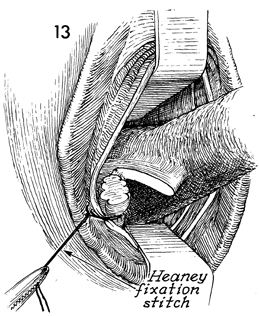
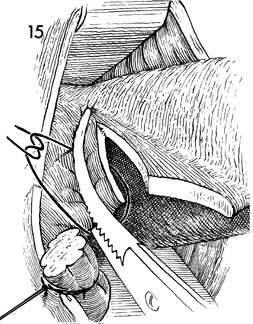
A Heaney fixation 0 synthetic absorbable
suture is used to suture-ligate the uterosacral ligament. In addition,
the first of four steps is initiated for vaginal cuff suspension.
In A, the suture has been placed from the inside
of the uterosacral ligament at the tip of the Heaney clamp through
the uterosacral ligament and brought out through the vaginal mucosa.
In B, the suture is brought back through the vaginal
mucosa and through the midportion of the uterosacral ligament underneath
the Heaney clamp. This plicates the uterosacral ligaments to the
angle of the vagina and aids hemostasis as well as vaginal cuff
suspension. |
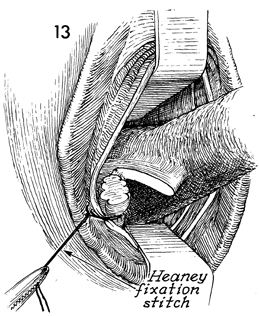
When tied, the suture is held with
a Kelly clamp for traction. This suture not only ligates the uterosacral
ligament but plicates that pedicle to the vaginal cuff. |
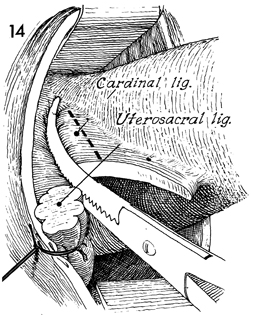
With the uterus on upward and lateral
retraction via the Jacobs tenacula on the cervix, the cardinal
ligament is clamped adjacent to the lower uterine segment and incised. |
The cardinal ligament is suture-ligated
with 0 synthetic absorbable suture. No fixation suture is used
here for fear of producing a hematoma in the vascular cardinal
ligament. Before proceeding farther up the broad ligament, the
lateral retractor and cervix are moved to the opposite side, exposing
the opposite uterosacral and cardinal ligaments, and they are likewise
clamped and suture-ligated. |
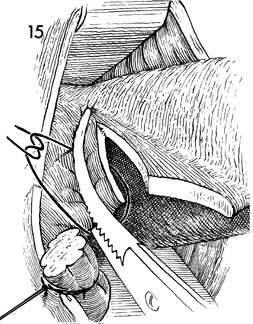
When the uterosacral and cardinal
ligaments on each side have been clamped, incised, and suture-ligated,
the remaining portion of the broad ligament attached to the lower
uterine segment containing the uterine artery is clamped adjacent
to the cervix. Use of a single clamp in the vaginal hysterectomy
reduces the chance of damage to the ureter, whereas using two clamps
will allow this portion of the broad ligament to be clamped in
its lateral position, thus increasing the chance of ureteral injury. |
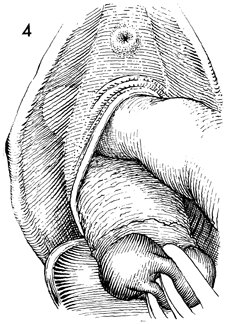
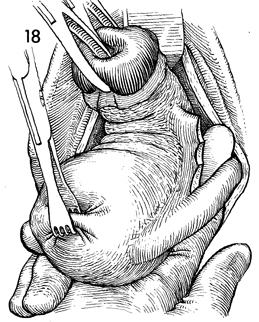
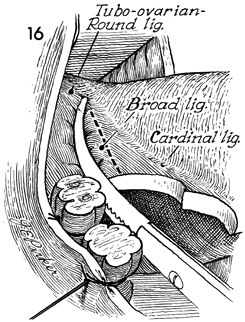
With the uterosacral ligament, the
cardinal ligament, and the uterine artery pedicle on both sides
now clamped, incised, and suture-ligated, the cervix is retracted
upward in the midline via the Jacobs tenacula. Thyroid clamps are
used to grasp the posterior uterine wall, and with a hand-over-hand
"walking out" technique the fundus is delivered posteriorly. |
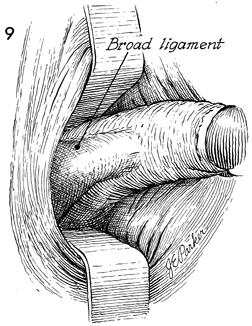
The Jacobs tenacula and the thyroid
clamp are held in one hand, and the finger of the opposite hand
is inserted under the tubo-ovarian round ligament, exposing the
ligated portion of the lower broad ligament. |
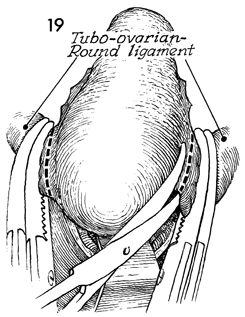
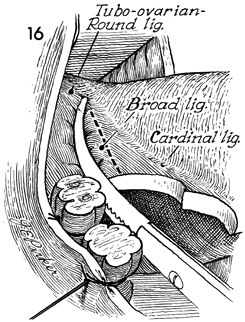
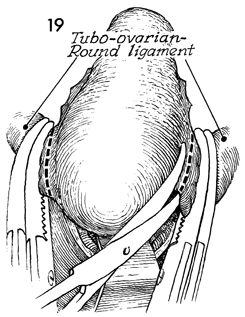
Two Heaney clamps are applied to the tubo-ovarian
round ligament, and it is incised close to the fundus. |
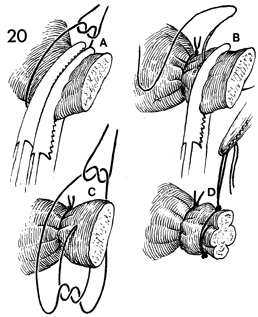
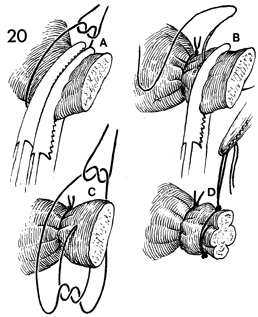
The tubo-ovarian round ligament
is tied twice. In A, a tie of 0 synthetic absorbable
suture is placed behind the second clamp. The tubo-ovarian round
ligament is tied with a simple 0 synthetic absorbable suture.
After the clamp at the rear of the pedicle is removed, the forward
clamp is "flashed" (i.e., slightly opened and immediately closed),
to allow the suture to securely ligate all the structures in
this pedicle.
In B, a second
suture ligature is tied in a fixation stitch, placing the suture
in the midportion of its pedicle. In C, the
suture is tied in front of and behind the pedicle prior to removing
the first clamp. In D, the pedicle is tied,
and the second suture is held in a straight clamp for traction. |
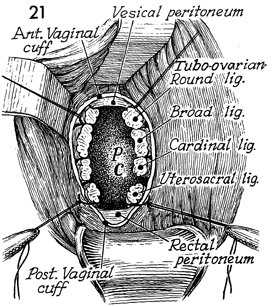
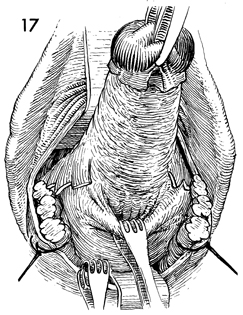
The anterior and posterior Heaney right-angle
retractors are removed, and the weighted posterior vaginal retractor
is placed in the vagina. The anterior vaginal wall is elevated
with a short-angle retractor. This allows better vaginal cuff
exposure. The entire broad ligament and its respective pedicles
are exposed from the tubo-ovarian round ligament anteriorly to
the uetrosacral ligament posteriorly. A free sponge is pushed
into the peritoneal cavity to displace the ovaries, tubes, and
bowel and give better exposure to the broad ligament structures.
The tail of the sponge is used to wipe the pedicles of each of
these ligaments to check for hemostasis. If there is bleeding
from any pedicle or portion thereof, the bleeding points can
be clamped with a curved Heaney clamp and suture-ligated. It
is preferable that the suture be brought through the tip of the
Heaney clamp and out through the vaginal mucosa. If the surgeon
encounters a wide area of bleeding, the entire broad ligament
can be suture-ligated by a running 0 synthetic absorbable suture
plicating the pedicles of the broad ligament to the lateral vaginal
mucosa. Care should be taken not to go deeper than the original
ties on the broad ligament pedicles to prevent damage to the
ureter.
The vesical peritoneal edge
can be identified by grasping the anterior vaginal wall with
tissue forceps. By using a hand-over-hand technique, the surgeon
can progressively pull the bladder wall down into the vagina
and easily identify the peritoneal edge. |
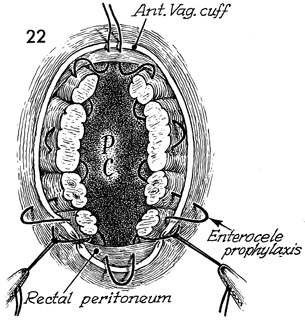
The reperitonealization of the
pelvis, carried out with pursestring sutures, provides the second
of four steps in suspension of the vaginal cuff. The suture is
started on the anterior peritoneal edge and brought through the
stump of the tubo-ovarian round ligament. After the stump of
the tubo-ovarian round ligament is sutured, the suture ligature
held for retraction can be cut. The pursestring is continued
down through one or more of the pedicles and is finally brought
through the uterosacral cardinal ligament pedicles and the vaginal
mucosa, plicating these pedicles to the vaginal mucosa to provide
additional suspension of the upper vagina. The suture is continued
posteriorly across the peritoneum of the cul-de-sac with one
or two stitches. The traction sutures in the uterosacral ligaments
should not be cut, as they are needed in a later step. The suture
is brought from the inside of the opposite uterosacral ligament
out through the vaginal mucosa and carried up the pedicles of
the opposite side until the tubo-ovarian round ligament on the
opposite side has been sutured. The traction suture on this pedicle
can be cut. The suture is passed through the anterior vesicoperitoneal
edge. When this suture is tied, the pelvis is reperitonealized,
and the stumps of the broad ligament are retroperitonealized. |
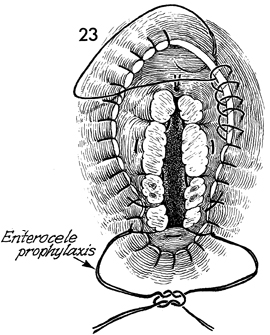
The vaginal cuff is never closed
and is left open for drainage to prevent postoperative pelvic
abscesses. A running locking 0 synthetic absorbable suture is
started at the 12 o'clock position on the anterior vaginal cuff
and is carried around the entire edge of the vagina until the
cardinal and uterosacral ligaments are reached. At that point,
the suture is brought through the cardinal and uterosacral, and
the surgeon again plicates these ligaments to the vaginal cuff,
completing the third of four steps in vaginal suspension. The
same is done for the uterosacral and cardinal ligaments on the
opposite side. The running locking suture is continued until
the entire cuff has been sutured. The two retraction sutures
held by Kelly clamps on the uterosacral ligaments are tied in
the midline. This aids in obliterating the cul-de-sac and reduces
the incidence of enterocele. |
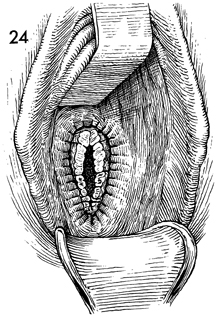
The final step is to observe the upper vaginal
area for hemorrhage. We prefer to catheterize the bladder at
the end rather than at the beginning of the procedure because
there may be less chance of injuring a bladder that is partially
filled with urine than one that is empty. No vaginal pack is
left in the vagina, and no Foley catheter is placed in the bladder.
All patients undergoing vaginal hysterectomy are given antibiotics
preoperatively.
VAGINAL BILATERAL SALPINGO-OOPHORECTOMY
DURING TOTAL VAGINAL HYSTERECTOMY
Under certain conditions the
Fallopian tubes and ovaries may be removed at the time of vaginal
hysterectomy. Salpingo-oophorectomy can be performed during the
hysterectomy, although it is easier to perform immediately after
the uterine specimen has been removed.
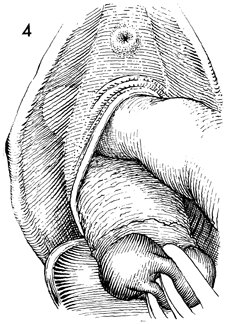
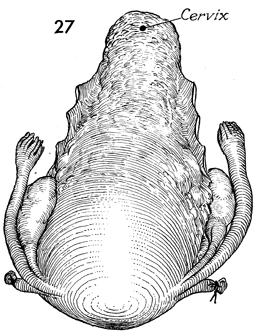
If the tubes and ovaries are to be removed with the specimen, the uterus is delivered
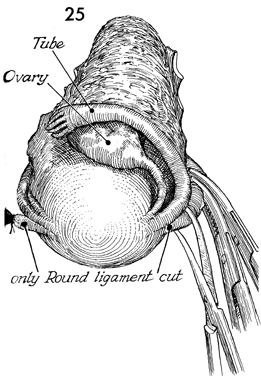
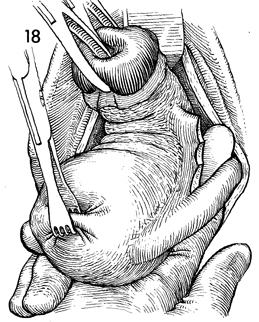
into the vagina as in Figure 18. |
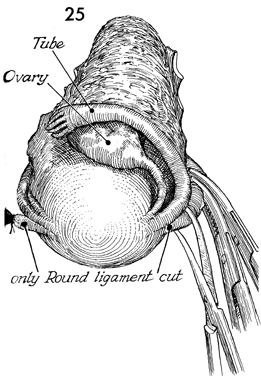
Exposure is facilitated by clamping and cutting
the round ligament on each side. The thyroid clamp on the fundus,
which has been placed on traction (Fig. 18), is removed to expose
the anatomy. |
 |
 |
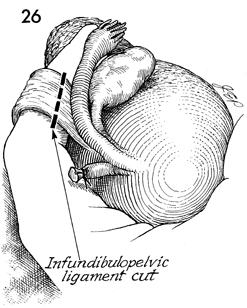
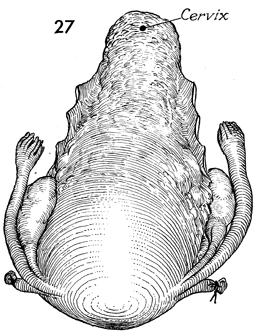
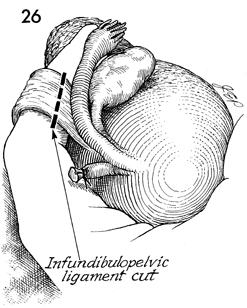
After
the round ligament has been cut and tied on each side, additional
traction on the uterine fundus delivers the fundus into the vagina
and places tension on the infundibulopelvic ligament. A finger
can be inserted up and under this ligament. Two Heaney clamps
are placed across the ligament. It is cut and doubly tied with
0 synthetic absorbable suture as demonstrated in Figure 20. The
second suture on this pedicle is held in a straight clamp as
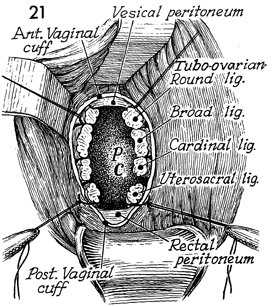
seen in Figure 21 (on the tubo-ovarian round ligament). Reestablishing
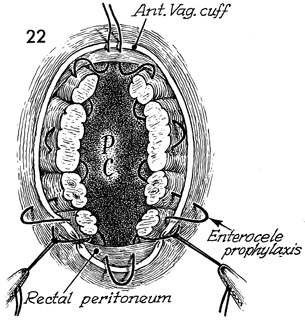
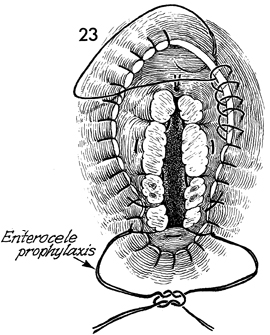
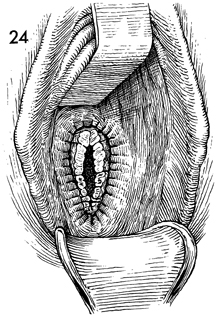
the peritoneum and vaginal cuff suturing are performed as in
Figure 22 and 23. The infundibulopelvic ligament pedicle is used
for establishing the peritoneal lining, as was the tubo-ovarian
round ligament pedicle in Figure 22. The vaginal cuff is sutured
with a running locking stitch and left open. |
|