
![]()
Suction Curettage for Abortion
Management of Major Uterine Perforations From Suction Curet or Radium Tandem
Jones Operation for Correction of Double Uterus
Richardson Composite Operation
Total Abdominal Hysterectomy With and Without Bilateral Salpingo-oophorectomy
Richardson Composite Operation
The Richardson composite operation is indicated in those patients with severe third degree uterine prolapse. The principle behind the operation is to remove the cervix and the fundus of the uterus, while leaving the lower uterine segment in place. This gives a structure to which the supporting ligaments of the uterus (uterosacral, cardinal and round) can be sutured.
Contraction, one of the physiologic principles of wound healing, frequently is an undesirable aspect of the surgical wounds. The power of contraction and epithelization needs little explanation as it is amply demonstrated in the grotesque contractures that can occur following burns.
Contraction of the remaining lower uterine segment after fundal and cervical amputation and ligament replacement firmly pulls the vagina upward. The Richardson composite operation utilizes this principle to the advantage of the patient.
The purpose of the operation is to correct third degree uterine descensus with cystocele and rectocele.
Pathophysiologic Changes: The predominant pathophysiologic changes in this procedure are those associated with contraction and wound healing. The denuded but vascular lower uterine segment following fundectomy and cervicectomy undergoes contracture and thereby provides midline pelvic support for the uterosacral and cardinal ligaments.
Points of Caution: The anterior and posterior cul-de-sacs must be entered early.
Care must be taken not to clamp and tie all vessels leading to the lower uterine segment.
The cervix should be amputated in a cone fashion.
The fundus should be amputated in a cone fish-mouth fashion that will facilitate its closure.
Hemostasis must be intact prior to reversing the rotation of the lower uterine segment after the fundectomy.
Technique
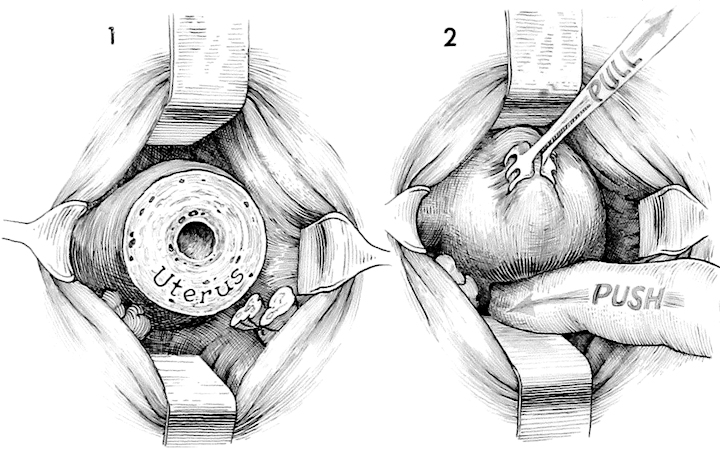
The initial steps in the Richardson composite are the same as those in the Manchester procedure. The junction of the vagina and cervix is circumscribed; the anterior and posterior cul-de-sacs are entered and retracted with right angle Haney retractors; the cardinal and uterosacral ligaments on each side are clamped, incised and tied with one absorbable suture; and the cervix is amputated slightly below the lower uterine segment.
With the right angle Haney retractors underneath the bladder and ureter anteriorly, and depressing the rectum posteriorly, thyroid clamps are utilized to grasp the anterior wall of the uterus and "walk down it" hand over hand. It is helpful to have an assistant push the lower uterine segment posteriorly with a finger, bringing the funds into the vaginal canal.
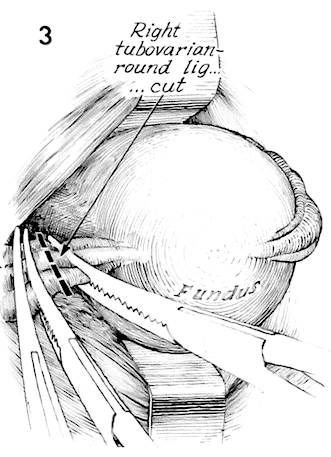
A thyroid clamp on the funds is used to deviate it to one side, exposing the tubo-ovarian round ligaments. They are triple clamped with Haney clamps and incised. Two suture ligatures are placed distal to the uterus behind each of the two clamps. The clamp proximal to the uterus on the stump of the incised tubo-ovarian round ligament can be left for traction if desired.
The opposite tubo-ovarian round ligament on the left side is handled in a similar fashion.
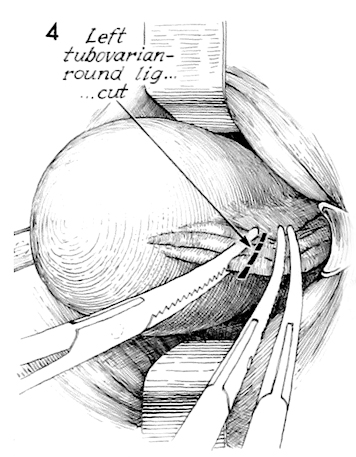
Additional Haney clamps are placed down the broad ligament, and each is incised and tied until the general area of the uterine artery is reached.
With traction on the fundus via the Haney clamps placed on the tubo-ovarian round ligament, amputation of the fundus is begun in a wedge-shaped fashion. The blade is angled into the lower uterine segment, producing a concave wedge-out wound.
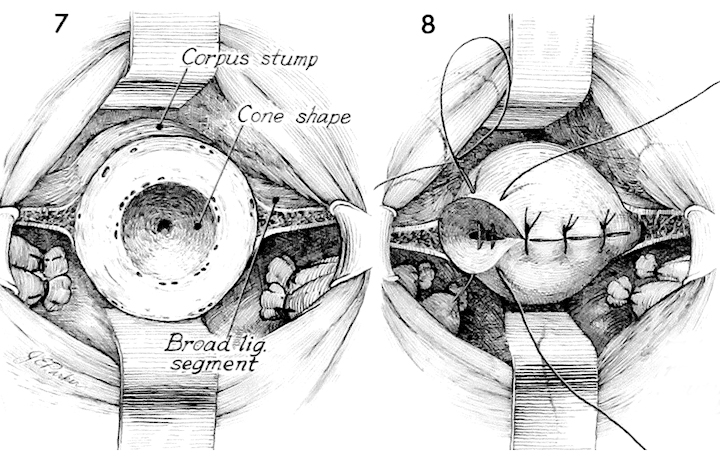
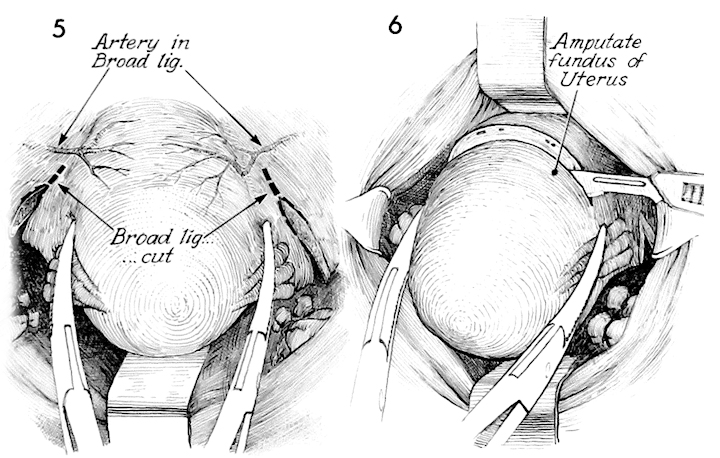
The cone-shaped wedged-out wound is demonstrated. Any major bleeders are clamped and tied. The broad ligament is thoroughly inspected for hemostasis.
The fundal wound is closed with interrupted 1 absorbable suture. At this point a subtotal vaginal hysterectomy and amputation of the cervix has essentially been completed. The lower uterine segment is left in place and viable.
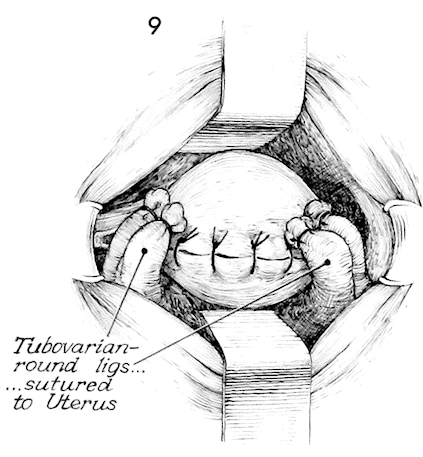
After closing the fundal incision, the tubo-ovarian round ligaments are sutured to the angles of the uterus by interrupted 1 absorbable sutures.
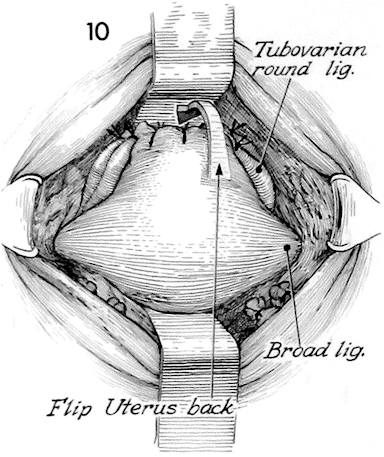
The lower uterine segment is maneuvered back into its normal position by placing an Allis clamp on the fundal suture line and pushing the fundus back into the pelvic canal under the bladder. Care must be taken not to rotate the lower uterine segment posteriorly as this would strangulate its blood supply and possibly shear off vessels causing hemorrhage.
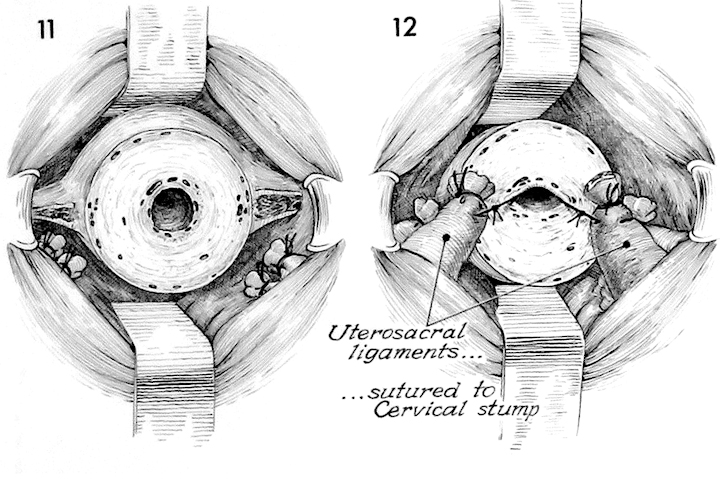
The lower uterine segment is again exposed with the left and right cardinal ligaments in place. The right angle Haney retractors are deflecting the bladder anteriorly and rectum posteriorly.
The uterosacral and cardinal ligaments are sutured into the angles of the lower uterine segment interrupted 1 synthetic absorbable suture. This suture is taken into the lower uterine segment canal, thereby drawing the uterosacral and cardinal ligaments firmly against the amputated lower uterine segment.
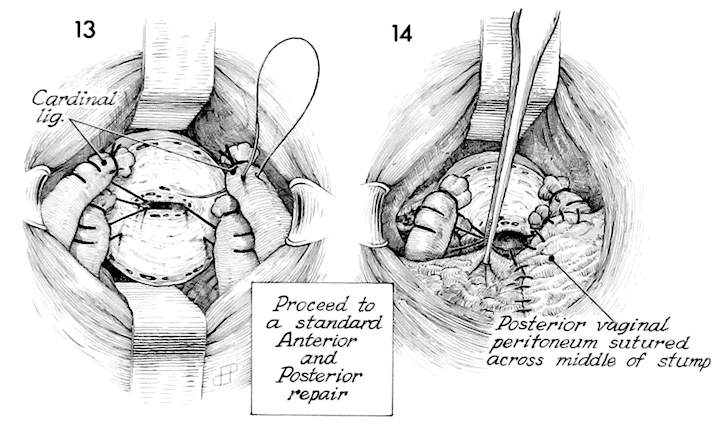
The cardinal ligaments are similarly sutured into this position. At this point many patients need an anterior and, frequently, a posterior repair. These may now be performed as previously describe in the section on Vagina. If there is stress incontinence of urine present, an anti-incontinence procedure may be performed.
The vaginal mucosa anteriorly and posteriorly is used to cover the lower uterine segment. Care is taken, as in the Manchester operation, not to totally obliterate the canal of the lower uterine segment. Although this is of less importance here, because coning these segments out has left little in the way of glandular tissue to secrete mucus, however, if mucus secreting glands are left the potential for mucocele is present, and a small opening therefore is desirable for drainage.
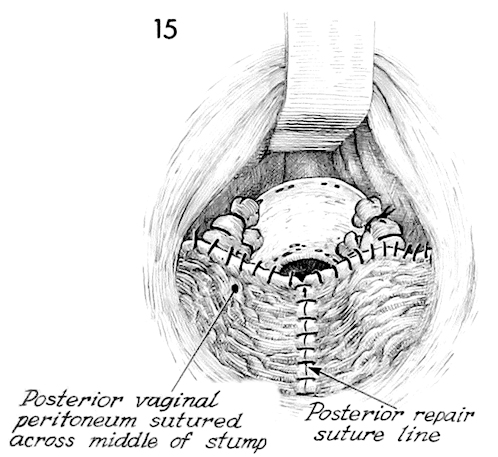
This drawing shows the completed posterior vaginal mucosa sutured into place.
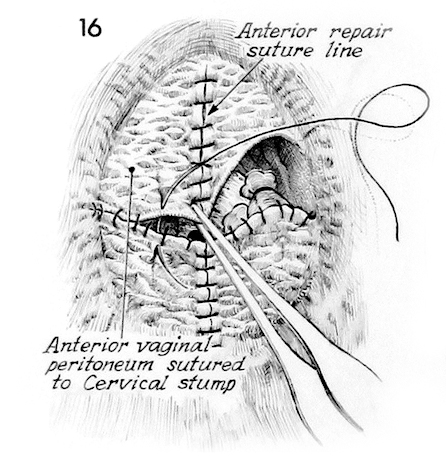
The anterior vaginal mucosa is then sutured to the posterior vaginal mucosa and the anterior lip of the lower uterine segment.
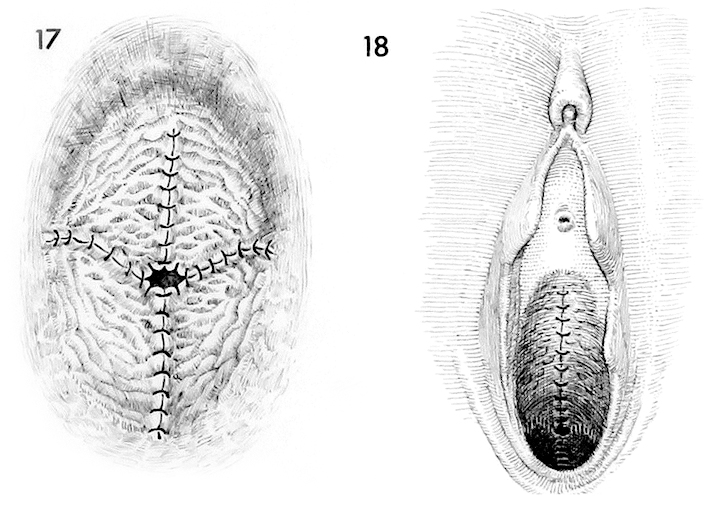
The operation is complete.
A view of the complete Richardson composite operation is illustrated. A Foley catheter is left in the bladder. Although no packing of the vaginal canal is recommended, it may be used at the discretion of the individual surgeon.