Uterus
Dilatation
and Curettage
Suction
Curettage
for Abortion
Management
of Major
Uterine Perforations
From Suction Curet or
Radium Tandem
Cesarean
Section
Myomectomy
Jones
Operation
for Correction of
Double Uterus
Hysteroscopic
Septal
Resection by Loop
Electrical Excision
Procedure (LEEP) for
Correction of a Double
Uterus
Manchester
Operation
Richardson Composite Operation
Total
Vaginal Hysterectomy
Total
Abdominal
Hysterectomy With
and Without Bilateral
Salpingo-oophorectomy
Laparoscopy-Assisted
Vaginal Hysterectomy |
Laparoscopy-Assisted
Vaginal Hysterectomy
There are two reasons for performing a laparoscopy-assisted
vaginal hysterectomy. The first is to attempt to make vaginal hysterectomy
with its advantages available to those women whose surgeons feel uncomfortable
with a regular vaginal hysterectomy and who have a tendency toward
performing the hysterectomy through the abdominal route with its disadvantages
of postoperative pain, need for hospitalization, and reduced time for
return to full activities and/or employment. The second is a significant
reduction in length of stay in the hospital with this procedure than
with an abdominal hysterectomy. It was originally thought that routine
vaginal hysterectomy required 5-6 days of hospitalization. Recently,
this has been shown to be untrue. It was originally thought that there
would be a cost savings from laparoscopy-assisted vaginal hysterectomy
compared with a regular vaginal hysterectomy. Several evaluations have
shown that because of the high cost of the instruments needed and the
length of operating time needed for laparoscopy-assisted vaginal hysterectomy,
this procedure is more expensive than a regular vaginal hysterectomy.
If the patient's surgeon feels uncomfortable with a regular vaginal
hysterectomy and would convert these operations to abdominal hysterectomy,
however, there is a definite advantage for the laparoscopy-assisted
vaginal hysterectomy in the length of stay, cost, and recovery.
The
typical patient on whom a surgeon would be tempted to perform a laparoscopy-assisted
vaginal hysterectomy would be one with myomata uteri, a history of
pelvic inflammatory disease, a history of previous pelvic surgeries
such as cesarean section, or significant endometriosis with adhesions
to bowel. The hypothesis is that with laparoscopy these variables can
be managed in a safer manner than with the traditional vaginal hysterectomy.
Physiologic Changes. The
predominant physiology is the loss of the uterus and the offending
signs and symptoms that require the uterus to be removed. If it is
a bleeding disorder, the bleeding will stop. If it is chronic pain
caused by the uterus, the pain should be eliminated. If it is an
ovarian-masking problem, the ovaries would now be free and could
be felt on routine examination. If there is carcinoma in situ or
significant cervical intraepithelial neoplasia, then that would be
removed.
Points of Caution. Laparoscopy is
not a completely complication-free operation. Bowel injuries, urinary
tract injuries, and hemorrhage are reported sequelae of laparoscopy.
Clinical experience in intra-abdominal laparoscopy as well as vaginal
hysterectomy must be obtained prior to initiating this procedure.
Technique
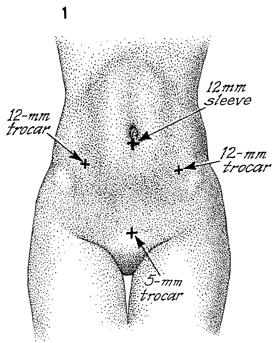
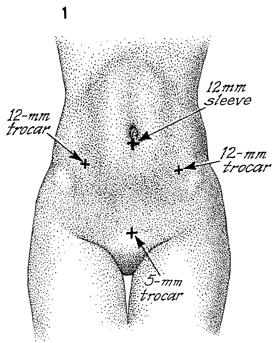
Usually, there are five sites of puncture
required for the insertion of the laparoscopic trocar and sleeves.
First, a 12-mm incision is made in the inferior rim of the umbilicus
for insertion of the observation laparoscope. Second, two 12-mm
incisions, one in the left lower quadrant and one in the right
lower quadrant, are needed. These incisions should be lateral
to the rectus abdominis muscle to avoid injury to the epigastric
vessels. Third, an incision is required for grasping forceps,
dissection scissors, and irrigation and suction instruments.
Fourth, a 5-mm suprapubic incision is needed for additional surgical
instrument. |
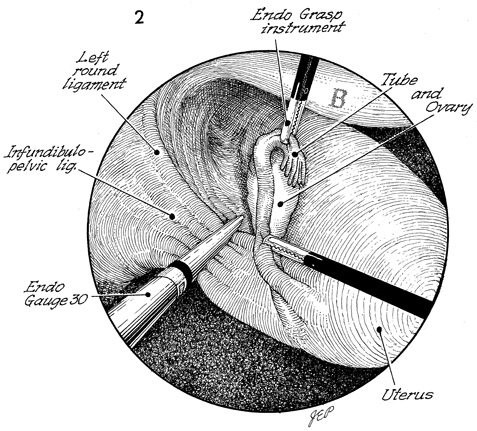
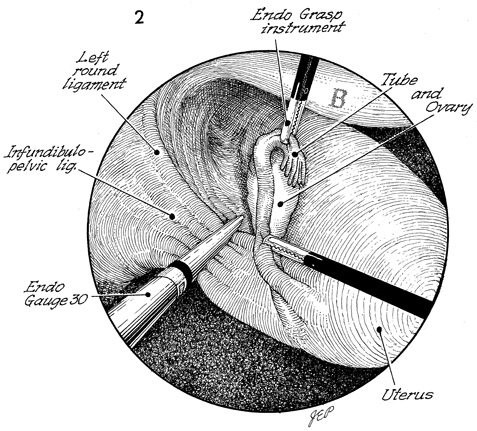
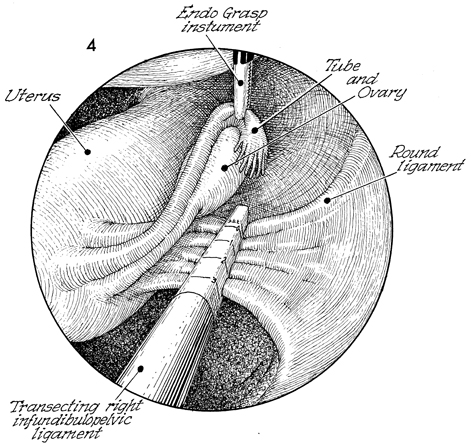
This laparoscopic view of the
pelvis shows the bladder (B) at the 12-1 o'clock position
and the fundus at the 4-5 o'clock position with the intra-vaginal
and cervical instrument manipulating the uterus so the infundibulopelvic
ligament can be exposed. A grasping forceps has been used to
remove the ovary and Fallopian tube medially, further exposing
the infundibulopelvic ligament. The ureter must be clearly identified
prior to placing the Endo-GIA (gastrointestinal anastomosis)
stapler on the infundibulopelvic ligament. First, the size and
thickness of the infundibulopelvic ligament must be known. This
can be best done by placing an Endo Gauge 30-mm instrument across
the infundibulopelvic ligament, measuring the thickness. This
allows for the appropriate Endo-GIA stapler to be placed. The
Endo-GIA stapler is placed across the infundibulopelvic ligament
as well as the round ligament. Care must be taken to ensure that
the ureter is not included in this grasp and is out of danger
from being transected and stapled. |
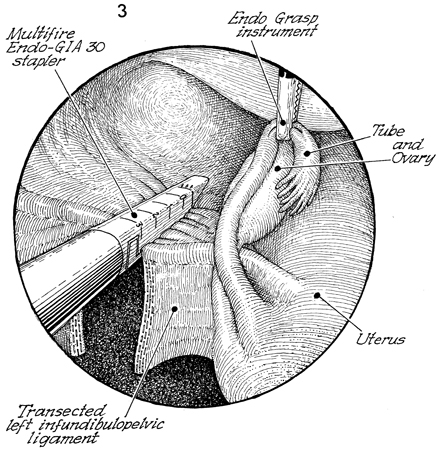
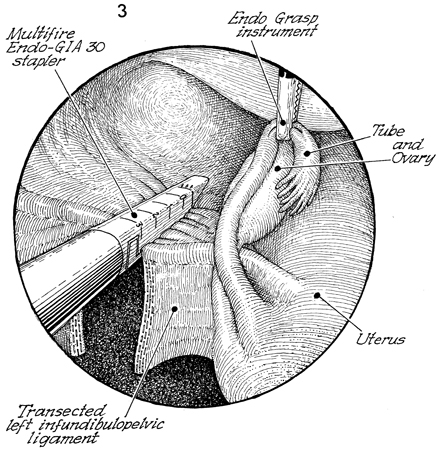
The fundus of the uterus is
at the 5 o'clock position, the tube and ovary have been removed
medially by the Endo Grasp instrument, the bladder is at the
2 o'clock position, and a second application of the multiple-fire
Endo-GIA 30 stapler is applied to the upper broad ligament. At
the 7 o'clock position, the previously stapled and incised left
infundibulopelvic ligament can be seen. The round ligament and
the upper portion of the broad ligaments are included in this
second bite of the Endo-GIA 30 stapler. |
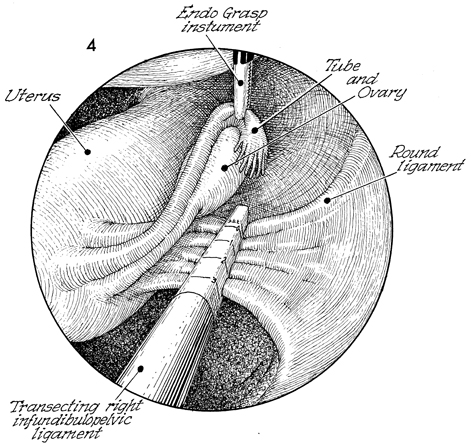
This endoscopic view shows
the fundus of the uterus at the 9 o'clock position, the bladder
at the 12 o'clock position, and the right infundibulopelvic ligament
exposed by manipulating the intra-vaginal cervical manipulator
as well as the grasping forceps, moving the tube and ovary medially.
The round and infundibulopelvic ligaments can also be seen. The
right ureter must be clearly identified before the Endo-GIA stapler
is placed on the infundibulopelvic ligament. |
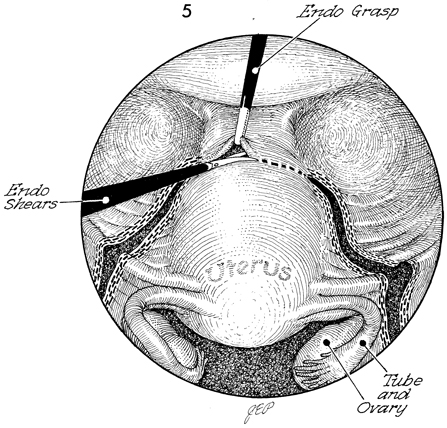
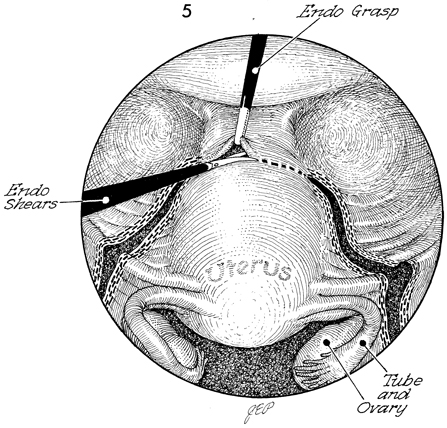
This laparoscopic view shows
the bladder at the 12 o'clock position and the right and left
infundibulopelvic ligaments stapled and transected. The round
and broad ligaments have been stapled and transected down to
a point approximately 0.5 cm above the ureter and uterine artery.
Endo Shears are used to transect the peritoneum over the anterior
uterine segment. |
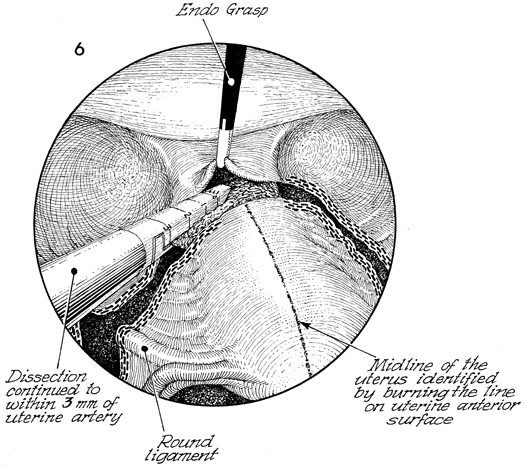
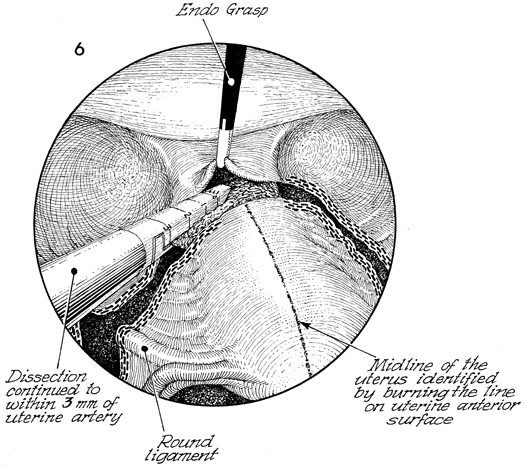
The vesicoperitoneum is grasped
with an endo-grasping forceps and elevated. The Endo-GIA stapler
is placed adjacent to the lower uterine segment on the lower
broad ligament but superior to the uterine artery.
To distinguish
the anterior from the posterior surface of the uterus, the midline
of the uterus from the fundus down to the lower uterine segment
is slightly coagulated with electrocoagulation forceps. |
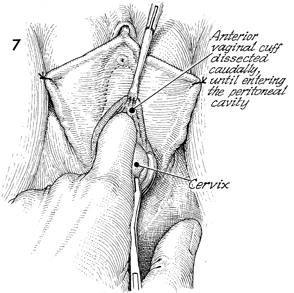
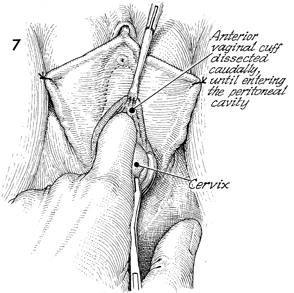
The surgeon goes below, leaving the laparoscope
in the hands of an assistant, and transects circumferentially
the vaginal mucosa immediately adjacent to the cervix. The cervix
is grasped with a Jacobs tenaculum, and the anterior vaginal
cuff is dissected caudally until the peritoneal cavity is entered
through the previous dissection of the vesicoperitoneal fold
seen in Figure 5. |
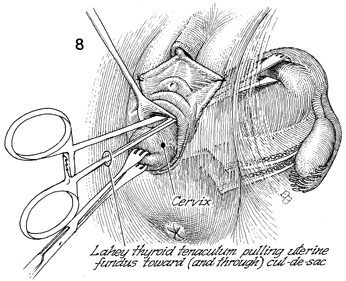
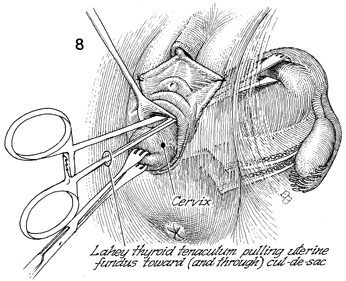
A Lahey thyroid tenaculum is placed into
the anterior cul-de-sac and pulls the uterine fundus through
the anterior cul-de-sac. Traction is maintained on the cervix
with the Jacobs tenaculum. |
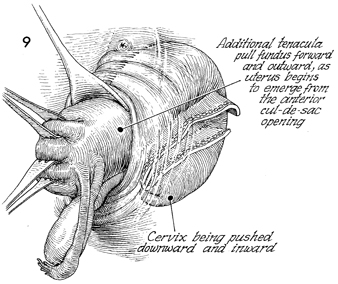
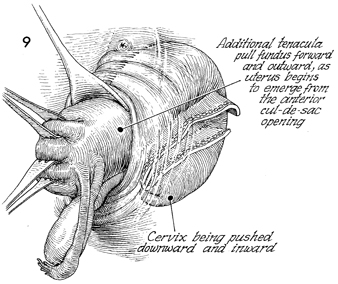
The tenaculum on the cervix is released,
allowing the uterus to be flipped forward; additional tenacula
are placed on the anterior uterine wall, progressively pulling
the fundus forward and outward as the uterus begins to emerge
from the anterior cul-de-sac opening. |
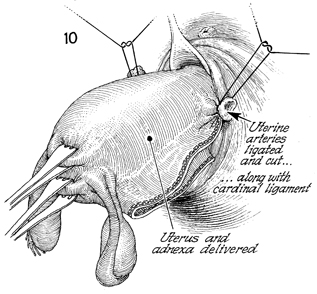
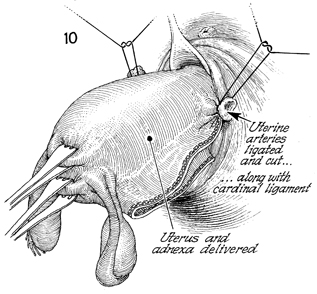
The uterine artery on both sides is clamped,
ligated, cut, and tied with synthetic absorbable suture. The
uterus and adnexa are delivered through the anterior cul-de-sac
wound. |
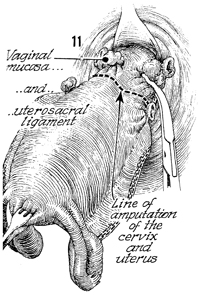
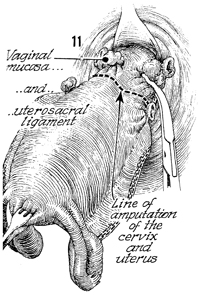
The posterior surface of the uterus from
the fundus to the lower uterine segment can be identified because
its lacks the burn stripe previously applied to the anterior
surface. The vaginal mucosa is identified on both sides; clamped
and incised. The clamp is placed slightly above the uterosacral
ligaments. The line of amputation of the cervix and uterus
is shown.
|
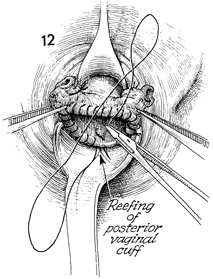
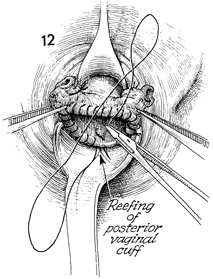
The vaginal cuff has been reefed with running
0 synthetic absorbable suture. |
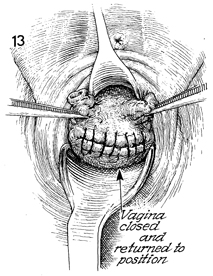
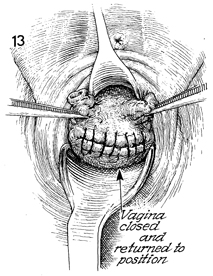
The vagina is closed and returned
to its proper position. The ties are seen on the uterosacral
ligaments. They are plicated in the midline for enterocele prophylaxis
and vaginal cuff suspension. |
|
|