Uterus
Dilatation
and Curettage
Suction
Curettage
for Abortion
Management
of Major
Uterine Perforations
From Suction Curet or
Radium Tandem
Cesarean
Section
Myomectomy
Jones
Operation
for Correction of
Double Uterus
Hysteroscopic
Septal
Resection by Loop
Electrical Excision
Procedure (LEEP) for
Correction of a Double
Uterus
Manchester
Operation
Richardson Composite Operation
Total
Vaginal Hysterectomy
Total
Abdominal
Hysterectomy With
and Without Bilateral
Salpingo-oophorectomy
Laparoscopy-Assisted
Vaginal Hysterectomy |
Manchester Operation
The Manchester operation was designed for women with
second-and third-degree uterine descensus with cystourethrocele. If
stress incontinence of urine accompanies the condition, the Manchester
operation can be combined with a Kelly plication of the urethrovesical
sphincter. The advantages of the Manchester operation are that the
surgeon does not enter the peritoneal cavity, the operating time is
reduced, and the operation is not associated with a prolonged or morbid
recovery. For all of these reasons, it is ideal for the elderly patient
with no other uterine disease.
The purpose is to reduce the cystourethrocele
and to reposition the fundus within the pelvis.
Physiological Changes. The principle behind use of
this procedure is to alter the angle of the uterus in the pelvis. This
is accompanied by bringing the cardinal and uterosacral ligaments anterior
to the lower uterine segment, which is displaced posteriorly. This
rotates the axis of the uterus to bring the fundus to an anterior position.
Points of Caution. Injury to the bladder can be avoided
by careful mobilization of the bladder off the lower uterine segment
and elevation of the bladder and ureter with a right-angle retractor.
Technique
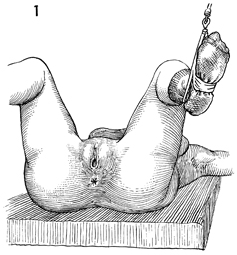
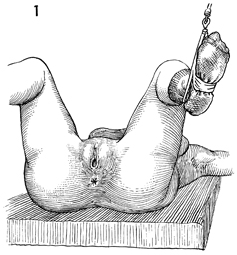
The patient is placed in the dorsal lithotomy
position. Thorough examination of the pelvis is performed. The
bladder is not catheterized because it can be identified and
dissected with greater safety when partially filled than when
empty. |
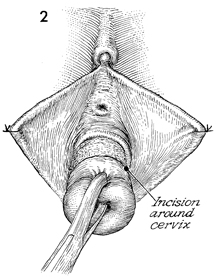
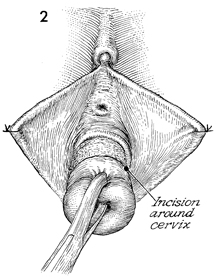
The labia may be tacked to the
perineum for retraction if they are redundant. A Jacobs tenaculum
is placed on the anterior lip of the cervix. Downward traction
on the cervix exposes the junction of the vagina and cervix where
a 360° circumcision incision is made. The bladder is sharply
and bluntly dissected off the lower uterine segment up to the
vesicouterine fold. |
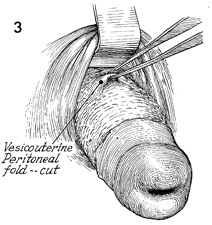
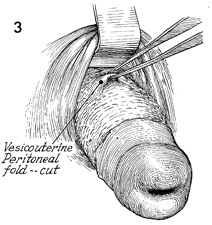
A right-angle retractor is placed under the
bladder to expose the vesicouterine peritoneal fold. This is
picked up and opened. |
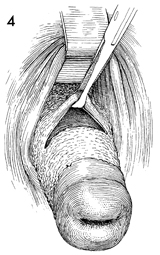
The anterior cul-de-sac is
opened, a finger is inserted, and the fundus and adnexa are explored. |
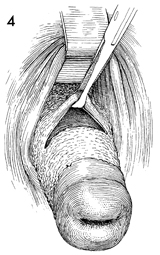
A right-angle Heaney retractor is placed
in the anterior cul-de-sac, allowing elevation of the bladder
and ureter. The cervix is rotated anteriorly, and the posterior
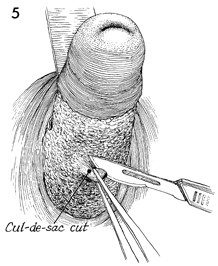
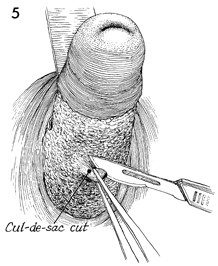
cul-de-sac is exposed. The peritoneum of the posterior cul-de-sac
is picked up and opened. |

The posterior cul-de-sac
is opened. A finger may be inserted into the cul-de-sac, and
the uterus and adnexa explored. |
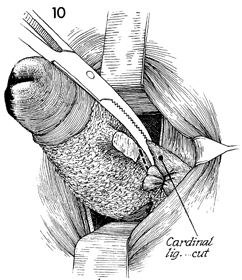
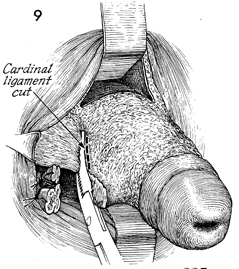
For demonstration purposes, two right-angle
retractors are shown, with the upper elevating the vagina and
bladder and the lower exposing the anterior cul-de-sac. The upper
retractor is removed, and the lower retractor is utilized to
elevate the bladder and ureter out of the surgical field. A right-angle
retractor is used to expose the lateral vaginal fornix. The cervix
is retracted to the contralateral side, exposing the uetrosacral
and cardinal ligaments. A finger is used to explore the posterior
cul-de-sac to ensure that bowel has not moved into this area
prior to placing the Heaney clamp on the uterosacral and cardinal
ligaments. The Heaney clamp should be placed immediately adjacent
to the body of the lower uterine segment. The tips of the clamp
should actually grasp a small portion of the lower uterine segment.
The uterosacral ligament and a small section of the cardinal
ligament are clamped and incised (dotted line). The
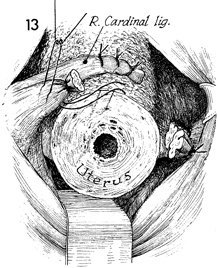
pedicle is tied with No. 1 synthetic absorbable suture. |
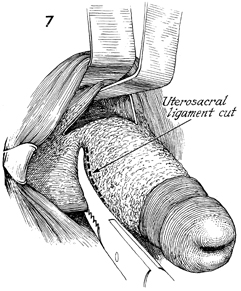
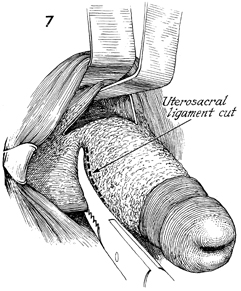
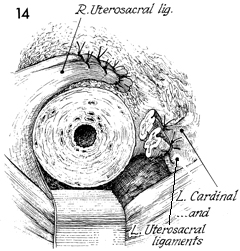
The right-angle Heaney retractors
are seen in the anterior and posterior cul-de-sac, and right-angle
lateral retractors have been moved to the left side of the vagina.
The cervix is deviated to the patient's right and slightly anterior,
exposing the uterosacral ligament on the left. The uterosacral
ligament is clamped, incised, and tied with 2-0 synthetic absorbable
suture. |
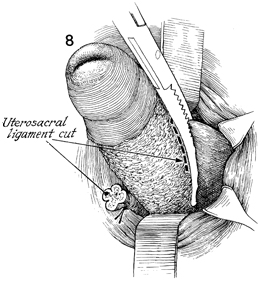
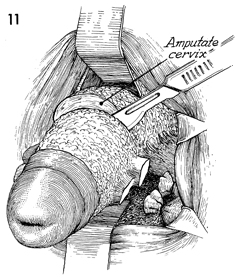
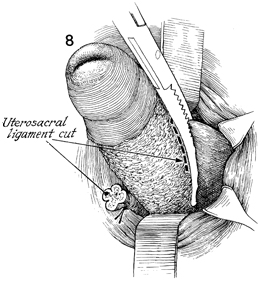
Depending on the length of the cervix, several
bites may be required to remove a long cervix while the right-angle
Heaney retractor is elevating the bladder and ureter. A small
portion of the cardinal ligament is clamped, incised, and tied
with 2-0 synthetic absorbable suture. |
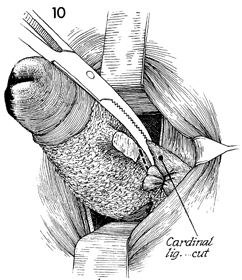
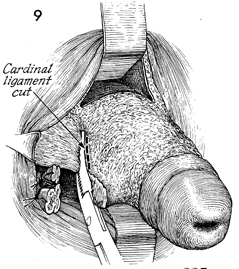
The cardinal ligament on the opposite side
is clamped, incised, and tied. |
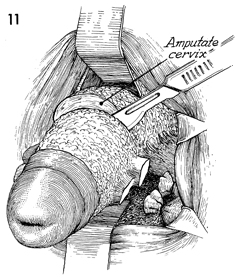
It is best to remove the cervix at the lower
uterine segment, and the surgeon must judge how much of the cervix
should be amputated. |
The anterior right-angle Heaney retractor
elevates the bladder and ureter, and the posterior right-angle
Heaney retractor depresses the rectum. Traction is made on the
cervix, and the amputation is made with a scalpel at the lower
uterine segment. |
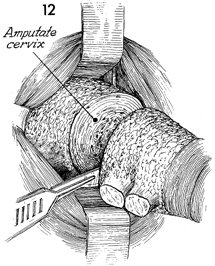
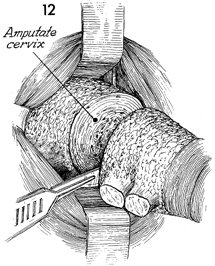
An attempt is made to angulate
the plane of the incision in the cervix so that it is "wedged
out' rather than incised perpendicular to its surface. This facilitates
coverage of the lower uterine segment with vaginal mucosa. The
lower uterine segment is moved posteriorly; the cardinal and
uterosacral ligaments are brought across the anterior surface
of the cervix and sutured to the lower uterine segment with interrupted
No. 1 synthetic absorbable sutures. The bladder and ureters are
elevated out of the surgical field with the right-angle Heaney
retractor. |
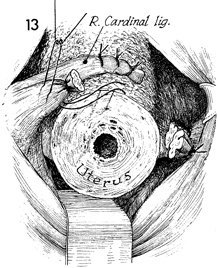
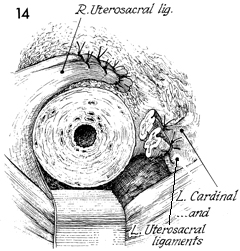
The right uterosacral and cardinal ligaments
have been sutured in place, and the left uterosacral and cardinal
ligaments are exposed. |
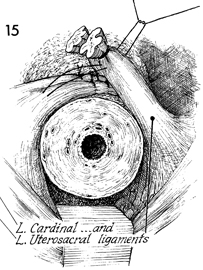
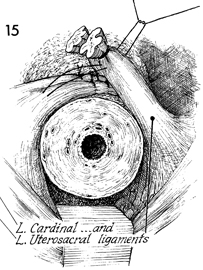
The left cardinal and uterosacral ligaments
are sutured in place, overlapping those from the right side and
creating a firm ligament band in front of the lower uterine segment.
The lower uterine segment is held posteriorly, bringing the fundus
anteriorly. The angle of the uterus is thus changed in the pelvic
canal. |
In most cases of second-and
third-degree uterine descensus, there will be significant cystourethrocele.
Therefore, the standard anterior repair as shown in Vagina and
Urethra, would be performed at this time.
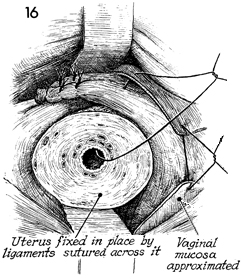
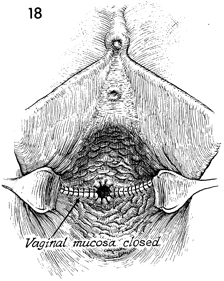
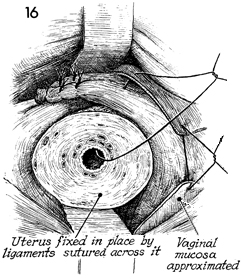
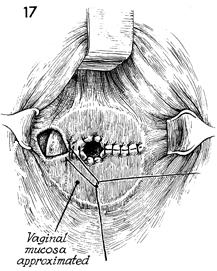
After the anterior repair has been performed,
the vaginal mucosa is closed with interrupted No. 1 synthetic
absorbable suture so that it covers the lower uterine segment
with vaginal mucosa. |
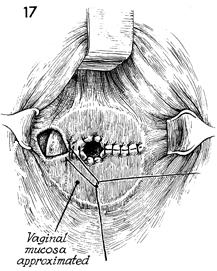
The row of interrupted synthetic absorbable
sutures closing the vaginal mucosa is extended to the opposite
side. |
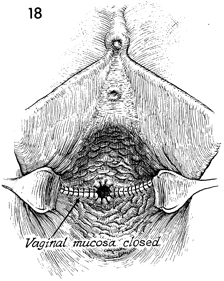
The finished procedure shows the uterine
canal opened for drainage of mucus.
A Foley catheter is placed in the bladder
and left in place for 4-5 days when an anterior repair and Kelly
plication have been performed. If no anterior repair or Kelly
plication was performed, a Foley catheter may not be necessary. |
|