Vulva
and Introitus
Biopsy
of the Vulva
Excision
of Urethral Caruncle
Bartholin's
Gland Cyst Marsupialization
Excision
of Vulvar Skin, with Split-Thickness Skin Graft
Bartholin's
Gland Excision
Vaginal
Outlet
Stenosis Repair
Closure
of Wide Local Excision of the Vulva
Wide
Local Excision
of the Vulva, With Primary Closure or Z-plasty Flap
Alcohol
Injection
of the Vulva
Cortisone
Injection
of the Vulva
Merring Operation
Simple
Vulvectomy
Excision
of the
Vulva by the Loop Electrical Excision Procedure (LEEP)
Excision
of
Vestibular Adenitis
Release
of Labial Fusion
Hymenectomy
Excision Of Hypertrophied Clitoris |
Simple Vulvectomy
Simple vulvectomy is indicated for severe lesions of
the vulva that are not amenable to local excision or other forms of
conservative therapy. These conditions include extensive in situ or
microinvasion carcinoma of the vulva, Paget's disease, and severe leukoplakia.
Unlike
radical vulvectomy, this simpler procedure does not require an incision
all the way to the perineal fascia. With adequate preoperative counseling,
the patient usually experiences few psychologic problems with regard
to her sexual functioning.
Physiologic Changes. The skin and subcutaneous tissues
of the vulva are removed.
Points of Caution. To avoid complications, particular
attention must be paid to the control of hemorrhage around the urethra
and the lateral pudendal vessels.
Technique
The
patient is placed in the dorsal lithotomy position with her
buttocks at least 3 inches off the end of the table. |
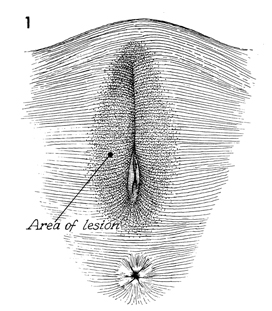
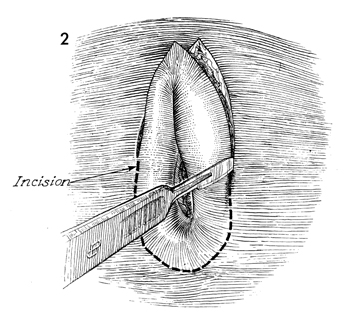
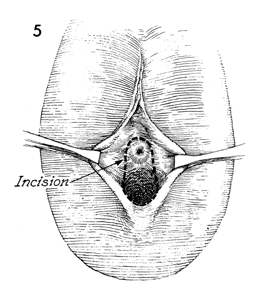
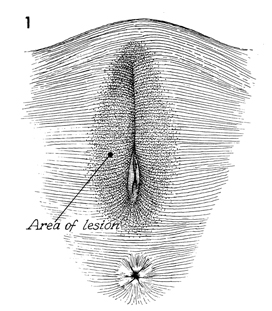
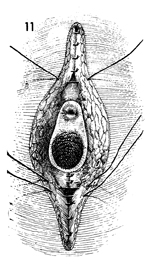
An outline of the lesion is made
with a brilliant green ink preparation. An elliptical incision
is made down to the subcutaneous fat. The incision starts from
above the labial folds on the mons pubis and is extended down the
lateral fold of the labia majora and across the posterior fourchette.
A dry pack is used to occlude the small bleeding vessels in the
skin until this incision is completed. |
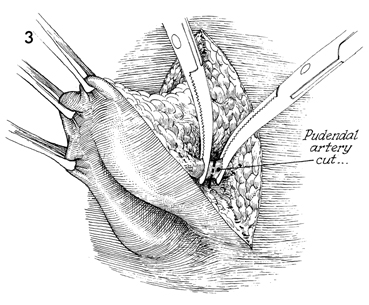
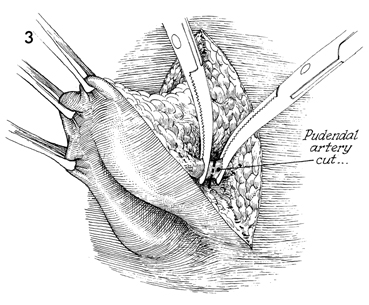
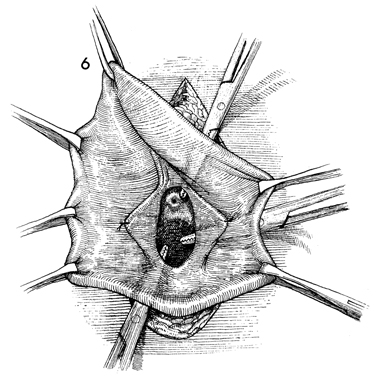
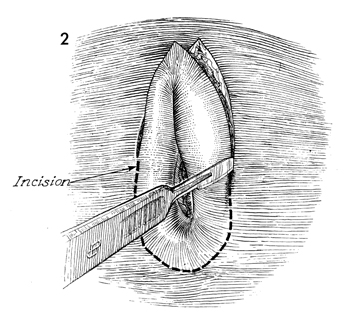
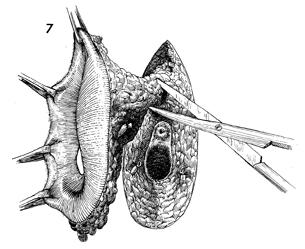
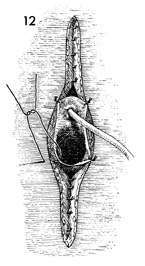
As the 3 and 9 o'clock positions
on the vulva are approached, the pudendal artery and vein are
encountered. These vessels, before being incised, should be
clamped to avoid major blood loss. For maximum exposure, the
specimen should be kept on tension by placing multiple Allis
clamps around the edges of the skin.
|
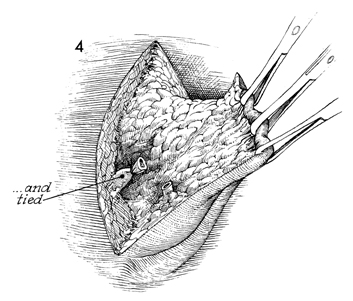
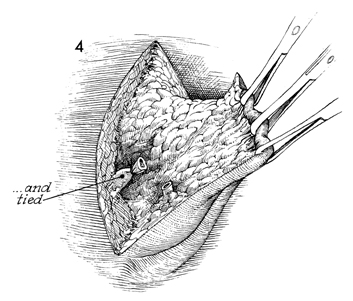
The pudendal vessels are securely tied, and the
incision is continued around the entire circumference of the lesion,
as shown in Figure 2. |
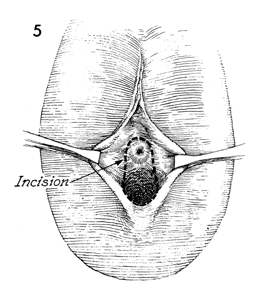
Exposure to the vaginal orifice
and urethra is made by retracting the labia laterally. The line
of incision around the urethra and vaginal orifice has been marked
with brilliant green surgical ink. The incision is started above
the urethral meatus and carried around the vaginal introitus
with an adequate margin around the lesion.
|
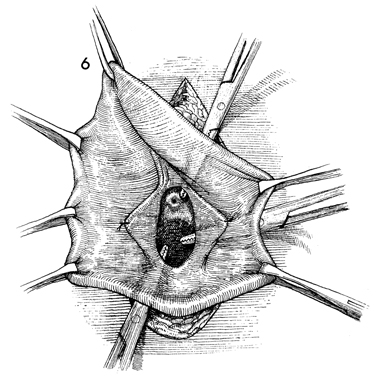
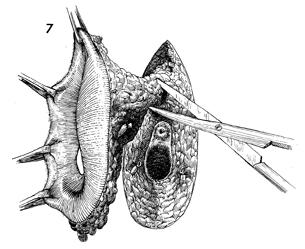
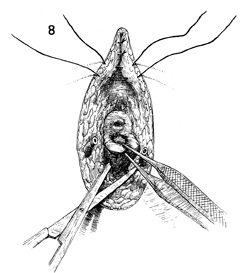
By palpating the incision above the urethral meatus
with the finger and placing a small hemostat behind the suspensory
ligaments of the clitoris, the surgeon makes an opening above the
urethra to ensure that damage to the urethral meatus is avoided.
A similar technique is used laterally to perforate the cutaneous
tissue from the lateral incision to the vaginal incision.
This technique can also be used inferiorly
to avoid damaging the rectum. The surgeon may place a finger in
the rectum while retracting the specimen superiorly and perforating
the dermis tissue between the inferior skin margin and the vagina
along the lines of the incision made in both structures. After
the dermis has been permeated, one blade of curved Mayo scissors
may be inserted to cut between the perforations. |
The specimen has been transected
between the perforations made in the vaginal mucosa, leaving
the specimen attached only to the fat pad in the mons pubis and
to the vascular plexus surrounding the suspensory ligaments of
the clitoris. This area should be clamped and tied before it
is transected with scissors. |
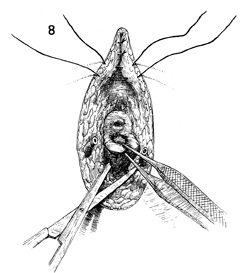
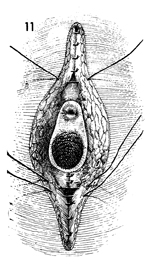
Primary closure of the wound
is begun. First, the posterior wall of the vaginal mucosa is
undermined and brought out to the posterior fourchette so that
contracture of the vaginal introitus is avoided. After hemostasis
is achieved, closure of the wound is continued superiorly in
the mons pubis by closing the subcutaneous tissue with interrupted
2-0 synthetic absorbable suture. |
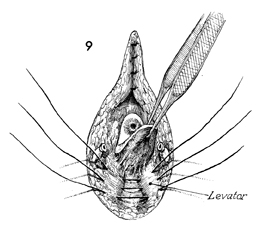
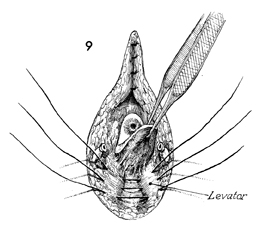
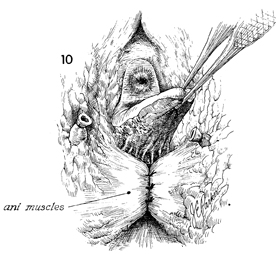
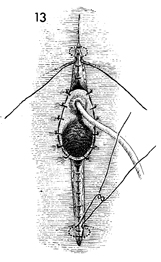
Three or four 2-0 synthetic
absorbable sutures are placed in the levator ani muscles, which
are plicated in the midline after the posterior vaginal mucosa
has been mobilized. Note that the subcutaneous tissue of the
mons pubis has been closed almost down to the urethral meatus. |
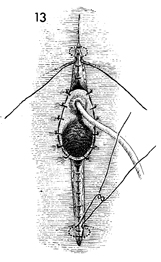
A close-up of the plicated levators,
the pudendal vessels, and the mobilized posterior wall of the
vagina is shown. |
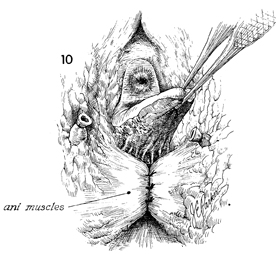
Closure of the subcutaneous
tissue of the perineal body is begun with interrupted 2-0 synthetic
absorbable sutures. The subcutaneous tissue remaining superiorly
is then closed. |
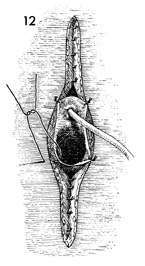
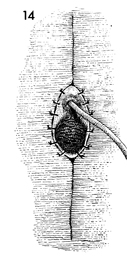
A catheter is inserted into
the urethral meatus, and the periurethral mucosa is sutured to
the skin with interrupted 3-0 synthetic absorbable sutures. The
vaginal mucosa is likewise sutured to the skin with interrupted
3-0 synthetic absorbable sutures. |
Skin closure is begun in a subcuticular
fashion over the mons and the perineal body, respectively, with
interrupted 3-0 synthetic absorbable sutures. The remaining vaginal
mucosa is sutured to the skin with interrupted 3-0 synthetic
absorbable sutures.
|
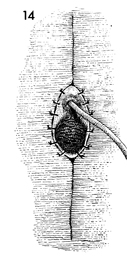
Final closure of the simple
vulvectomy is made by using synthetic absorbable sutures, making
permanent sutures unnecessary. During closure of this incision,
it is most important to eliminate tension on the suture line.
The surgeon should mobilize the perineal tissues until the margins
of the wound come together without tension. The Foley catheter
is left in place for 24 hours and then removed. The patient is
ambulated immediately. Laxatives and stool softeners are administered
on the third postoperative day. |
|