Vulva
and Introitus
Biopsy
of the Vulva
Excision
of Urethral Caruncle
Bartholin's
Gland Cyst Marsupialization
Excision
of Vulvar Skin, with Split-Thickness Skin Graft
Bartholin's
Gland Excision
Vaginal
Outlet
Stenosis Repair
Closure
of Wide Local Excision of the Vulva
Wide
Local Excision
of the Vulva, With Primary Closure or Z-plasty Flap
Alcohol
Injection
of the Vulva
Cortisone
Injection
of the Vulva
Merring Operation
Simple
Vulvectomy
Excision
of the
Vulva by the Loop Electrical Excision Procedure (LEEP)
Excision
of
Vestibular Adenitis
Release
of Labial Fusion
Hymenectomy
Excision Of Hypertrophied Clitoris |
Wide Local Excision of the Vulva,
With Primary Closure Or Z-plasty Flap
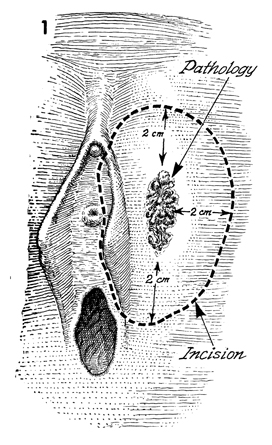
A wide local excision is indicated for women with in
situ or microinvasive carcinoma of the vulva. The goal of this operation
is to remove the carcinoma and a 2-cm margin of normal skin surrounding
the gross lesion. It is imperative that prior to making the incision
the surgeon measure the margin with a centimeter rule and outline it
with a marking pen to ensure that the specimen is adequate.
If the 2-cm
margin is not measured and the skin is not marked prior to the incision,
all too often the specimen sent to the pathologist will not have an
adequate margin.
In most cases, adjacent vulvar skin
can be mobilized and used to effect a primary closure of the vulva.
This is done in two layers after adequate hemostasis has been achieved.
In cases where extensive lesions are removed
and the defect is too large for primary closure, a Z-plasty flap may
be used to cover the wound without resorting to a split-thickness skin
graft.
Physiologic Changes. The in situ carcinoma
is removed without significant alteration of the physiology of the
vulva.
Points of Caution. Preoperative measurement
and marking of the diseased areas are mandatory. The Z-plasty flap
or primary closure should be completed, as large defects should not
be left in the vulvar area to simply granulate in and epithelialize.
If primary closure is to be performed, adjacent vulvar skin should
be adequately mobilized so that the suture line enclosing the vulva
is not under tension.
If the excised defect is too large for primary
closure, as demonstrated by tension on the suture line, the Z-plasty
flap procedure should be performed. In this case, care should be taken
to ensure that (1) the distance from point A to point B
on the Z-plasty flap is shorter than the distance from point B
to the margin of excised defect and (2) there is an adequate blood
supply entering the base of the flap. It is essential that all tissues
be adequately mobilized to avoid any tension on any suture line within
the flap area.
Patients
who have undergone a Z-plasty flap procedure recover best with complete
bed rest for 7 days. Intermittent pressure cuffs are applied to the
legs for thromboembolic prophylaxis. Defecation should be postponed
by a low-residue diet and the administration of Lomotil, 1 tablet q.i.d.
for 7 days.
Patients having primary closure for relatively small
vulvar defects do not require bed rest or bowel restriction.
Technique
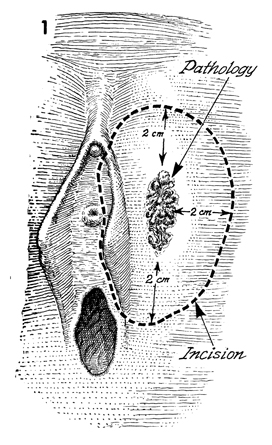
Wide Local Excision
The patient is placed in the dorsal lithotomy
position. The perineum is prepped and draped. With a centimeter
ruler, a 2 cm margin is measured around the lesion and marked
with brilliant green solution. Frequently, the labia minora have
to be sacrificed. |
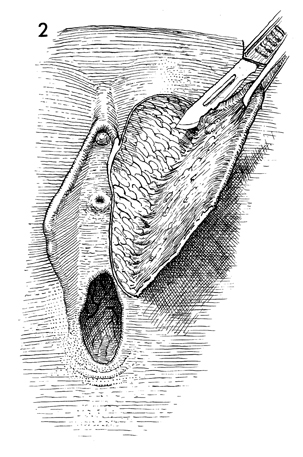
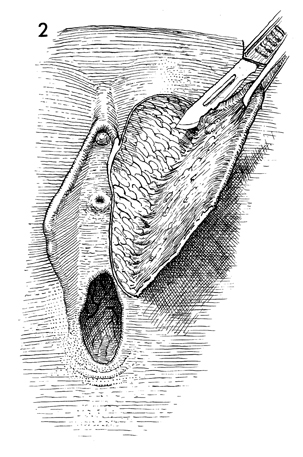
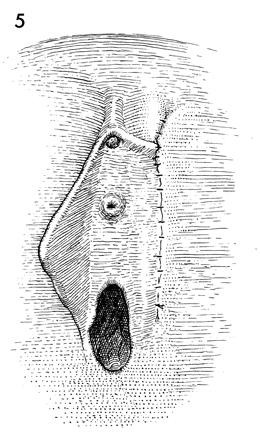
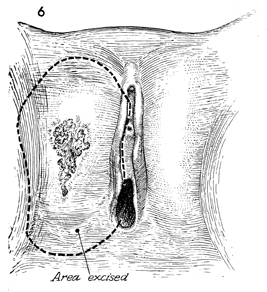
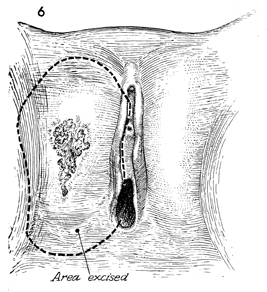
The margin of the lesion is excised
down to the subcutaneous tissue, and the tissue is elevated with
forceps. The entire lesion with its 2-cm margin and its subcutaneous
tissue is excised.
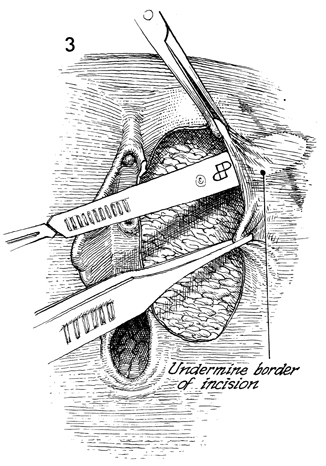
Meticulous hemostasis is achieved
at this point with fine pickups and electrocautery. Larger vessels
are delicately tied with 4-0 or 5-0 delayed synthetic absorbable
suture. At this point the defect is measured, and the surgeon decides
whether to proceed with primary closure of the wound or with a
Z-plasty flap. |
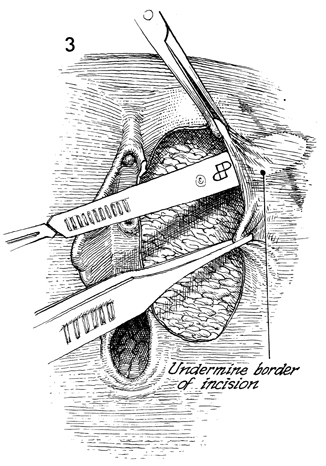
Primary Closure
Adequate mobilization of adjacent vulvar
skin is made by sharp and blunt dissection. It is essential that
the wound be closed without tension. Sutures should merely hold
the tissue that has been adequately mobilized and approximated. |
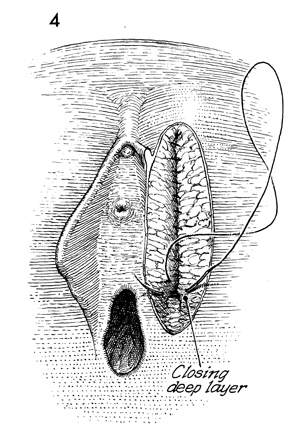
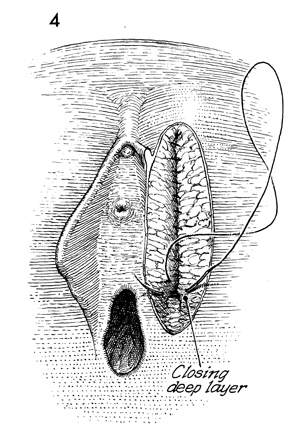
A continuous layer of 4-0 synthetic absorbable
sutures stitched with an intestinal needle is used to close the
subcutaneous space.
|
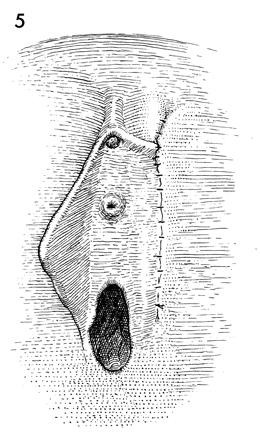
A subcuticular technique can
be used to approximate the skin, using 4-0 synthetic absorbable
suture. Small stainless steel skin clips can also be used and
can be removed on the seventh or eighth postoperative day. Fine
nylon sutures can be used in either a mattress technique or the
so-called flap stitch technique. These are removed on the seventh
or eighth postoperative day. |
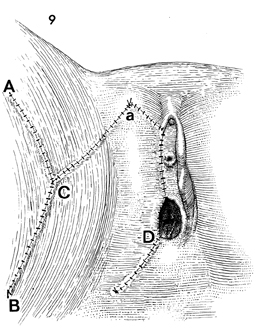
Z-Plasty Flap
If the lesion to be removed
leaves an excessively large defect, primary closure may be impossible.
In these cases, a Z-plasty flap may be the procedure of choice. |
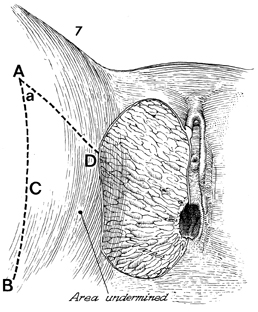
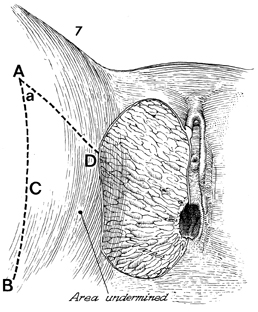
The defect is measured with
a ruler. The medial margin usually extends from the clitoral
area to the posterior fourchette of the vagina and is equal to
the distance on the proposed flap by the line marked A-D. It
is essential that the base of the flap from B to the
lateral edge of the defect be wider than the length of the flap.
The blood supply to the flap will enter through this area, and
if the length of the flap is longer than the width of the base,
the flap will have insufficient blood supply, and its tip may
necrose. A scalpel is used to incise the border of the flap through
a full thickness of skin and subcutaneous fat. Meticulous hemostasis
must be achieved at this point. |
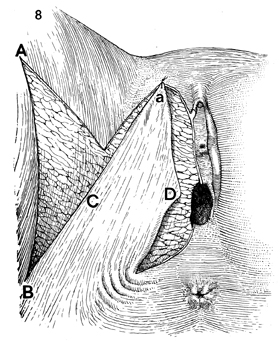
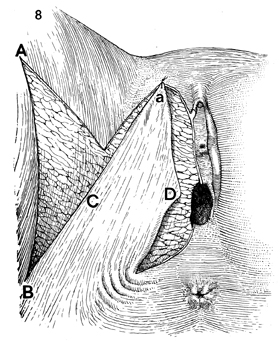
The portion of the flap marked a should
be stitched with fine synthetic absorbable suture to the ventral
margin of the defect. This suture should be in the form of a
flap stitch that enters the full thickness of the skin of the
margin of the defect and is brought through the flap with a subcuticular
technique. The needle reenters the subcuticular layer of the
flap skin adjacent to the first suture, then reenters the full
thickness of the margins of the defect from the subcutaneous
layer and exits the cutaneous layer adjacent to the first suture.
This flap stitch aids healing by less constricture of the blood
supply in the flap. The second suture should be placed in the
posterior fourchette of the vagina and be brought to the angle
of the flap marked D with
the same stitch described above. At this point, the part of the
flap marked C should be sutured with the flap stitch
to the angle (ABC) created by the entire Z-plasty. After the
margins of the flap have been sutured, the surgeon can make adjustments
if necessary. If undue tension is noted at any particular point,
it can be released by greater mobilization of adjacent skin. |
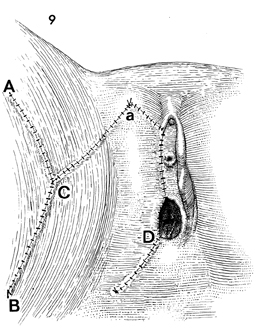
Several techniques are acceptable
for suturing the flap to the adjacent recipient skin and vaginal
wall. The new stainless steel skin clips have the advantage of
being inert and causing little tissue reaction. They can be left
in for long periods of time to allow for complete closure and
healing of the wound. Synthetic absorbable suture material can
be utilized and, in general, gives improved cosmetic result.
Sutures of fine nylon, in the flap stitch technique, can be used
throughout the closure. These require removal after the margins
of the wound have completely healed. Patients who have undergone
large perineal Z-plasty flaps should remain in bed for a minimum
of 6-7 days.
Thromboembolic prophylaxis utilizing
the contemporary technique of intermittent pressure cuffs is
essential. Defecation should be delayed for 6-8 days until the
margin of the flap has sealed. This is achieved by a low-residue
diet and the administration of Lomotil tablets q.i.d. |
|
|