Vulva
and Introitus
Biopsy
of the Vulva
Excision
of Urethral Caruncle
Bartholin's
Gland Cyst Marsupialization
Excision
of Vulvar Skin, with Split-Thickness Skin Graft
Bartholin's
Gland Excision
Vaginal
Outlet
Stenosis Repair
Closure
of Wide Local Excision of the Vulva
Wide
Local Excision
of the Vulva, With Primary Closure or Z-plasty Flap
Alcohol
Injection
of the Vulva
Cortisone
Injection
of the Vulva
Merring Operation
Simple
Vulvectomy
Excision
of the
Vulva by the Loop Electrical Excision Procedure (LEEP)
Excision
of
Vestibular Adenitis
Release
of Labial Fusion
Hymenectomy
Excision Of Hypertrophied Clitoris |
Vaginal Outlet Stenosis Repair
Vaginal outlet stenosis is sometimes seen in virgins,
but it appears most often in a woman who has undergone repair of an
episiotomy or posterior repair. In relieving this condition, which
is obviously associated with extreme dyspareunia, the surgeon opens
the posterior outlet and pulls the mobilized vaginal mucosa onto the
posterior fourchette and the perineal body. Postoperatively, the vaginal
mucosa is treated with estrogen so that it becomes well cornified.
Physiologic Changes. The vaginal outlet is opened
sufficiently to allow pain-free sexual intercourse.
Points of Caution. Adequate mobilization of the
posterior vaginal wall is extremely important in order that it may
be pulled over the perineal body.
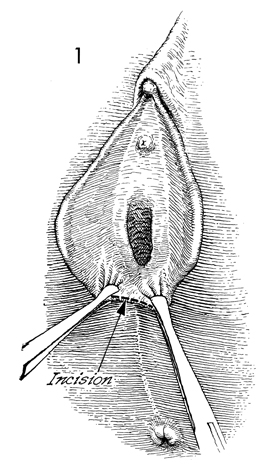
Technique
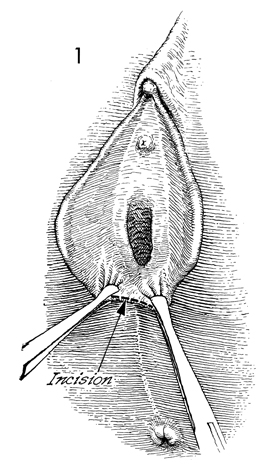
In a standard case of vaginal
outlet stenosis, Allis clamps are applied at the 7 and 5 o'clock
positions, respectively, and an incision is made at the posterior
fourchette. |
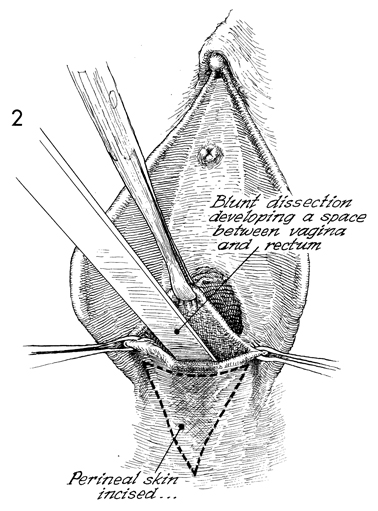
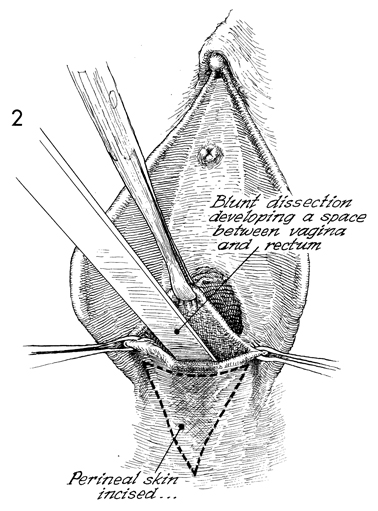
Dissection is carried up under the
posterior vaginal wall for a distance of approximately 7-8 cm.
A triangle of skin is removed from the perineal body, from the
posterior fourchette down toward the anus. |
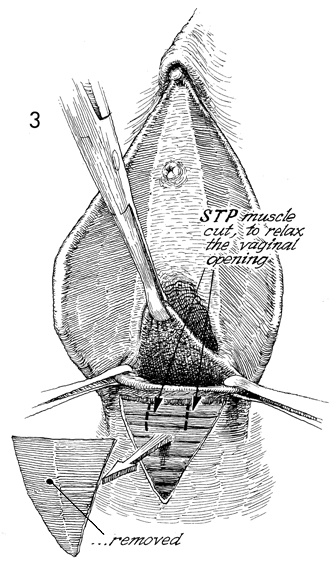
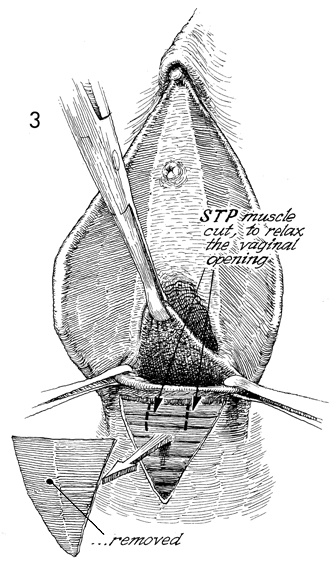
The superficial transverse
perineal (STP) muscle is exposed. Small incisions are made
into this muscle in order to relax the vaginal outlet. An Allis
clamp is used to keep the posterior vaginal wall on traction.
|
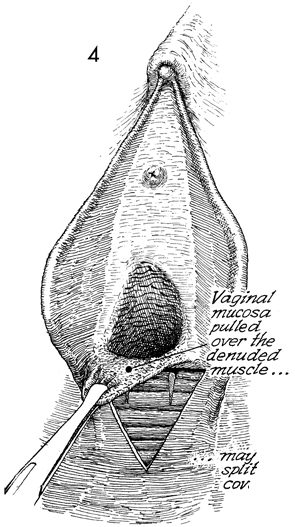
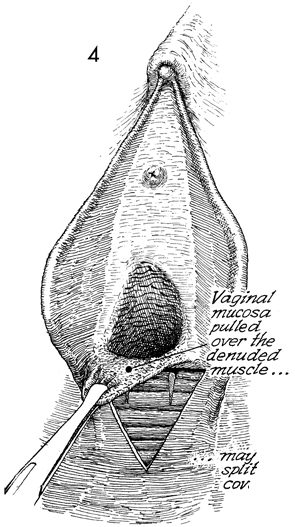
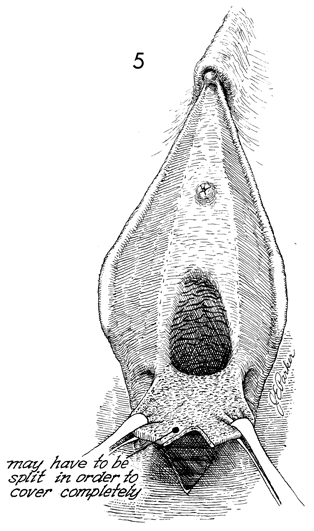
The posterior vaginal mucosa is pulled
over the denuded superficial transverse perineal muscle onto
the perineal body. |
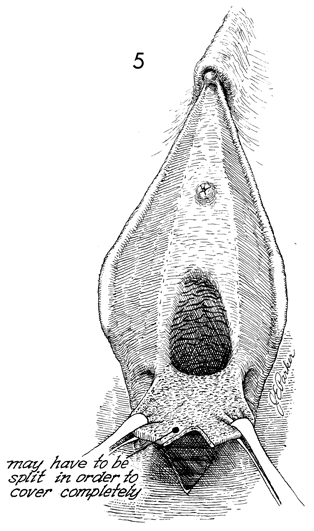
If sufficient posterior vaginal wall
mucosa is not available to cover the perineal defect, the vaginal
mucosa can be split in the midline, thereby enlarging the flap
to allow adequate coverage.
|
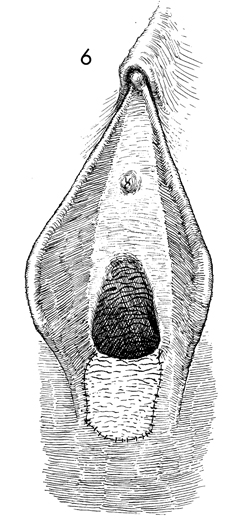
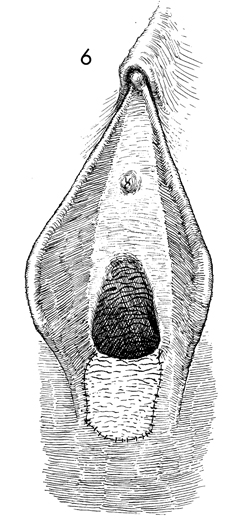
The posterior vaginal mucosa is sutured to the
skin of the perineal body with interrupted 4-0 synthetic absorbable
sutures. |
|