|
||||||||
Bartholin's Gland Cyst Marsupialization Excision of Vulvar Skin, with Split-Thickness Skin Graft Vaginal
Outlet Closure of Wide Local Excision of the Vulva Wide
Local Excision Alcohol
Injection Cortisone
Injection Excision
of the |
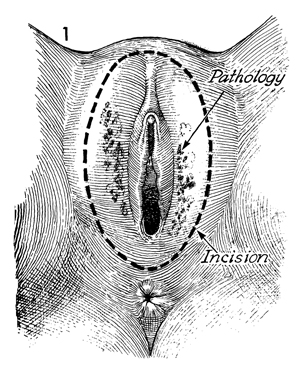
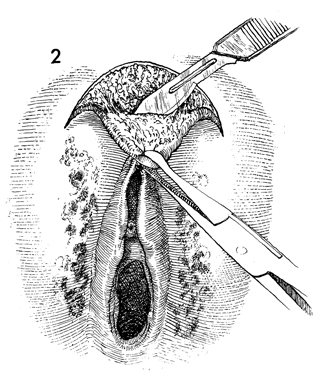
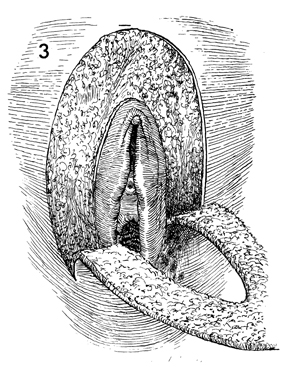
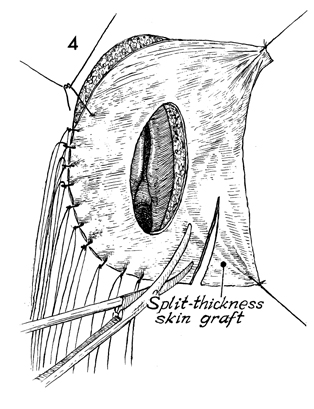
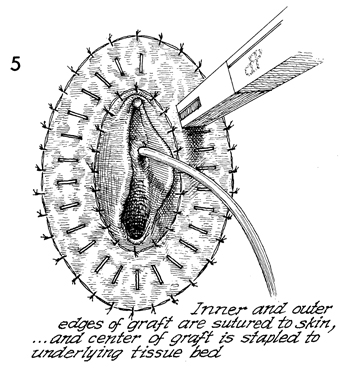
Excision of Vulvar Skin, A cutaneous vulvectomy is indicated for young women with extensive in situ carcinoma of the vulva. The goal in such an operation is to remove the in situ carcinoma but to leave a functional vulva that is psychologically as well as physically satisfactory to the patient. To accomplish this, the surgeon removes the cancerous vulvar epithelium and replaces it with a split-thickness skin graft of normal epithelium from a selected donor site. Physiologic Changes. The in situ cancer is removed. Points of Caution. Meticulous hemostasis should be complete in the wound prior to applying the split-thickness skin graft. This aids essential nutrition through transudation during the first 48-72 hours, until microcapillary neoangiogenesis connects the graft with the general circulation within the recipient site. Technique
|
|||||||
Copyright - all rights reserved / Clifford R. Wheeless,
Jr., M.D. and Marcella L. Roenneburg, M.D.
All contents of this web site are copywrite protected.