The Le Fort operation is an excellent procedure
for complete prolapse in elderly women who have had adequate sexual
counseling and who under no circumstances expect to have intercourse
in the future. Failure or recurrent prolapse after the procedure
is extremely rare. If
the procedure removes excessive anterior vaginal wall, however, the
urethrovesical angle may be brought down to the posterior fourchette,
and some patients will have either stress or overflow incontinence
of urine. To avoid this problem, we have modified the operation to
include the upper two-thirds of the vagina but not the lower third
of the anterior vaginal wall. Although a slight urethrocele may remain,
this generally causes no discomfort to the patient and at the same
time reduces the incidence of postoperative urinary incontinence.
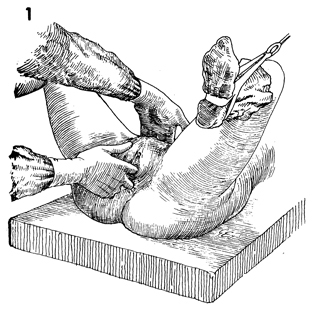
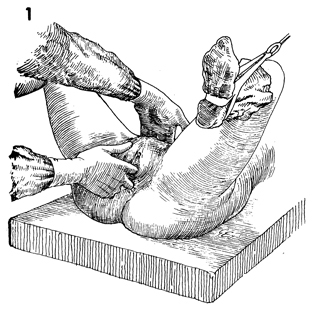
The patient is placed in the dorsal
lithotomy position and carefully examined under anesthesia. The
vulva and perineum are prepped and draped. |
The labia are anchored laterally
with interrupted 2-0 synthetic absorbable suture. |
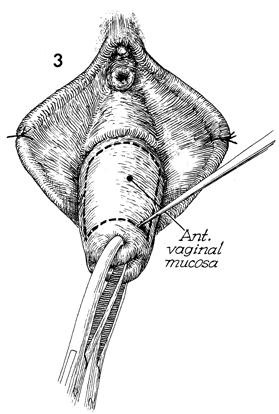
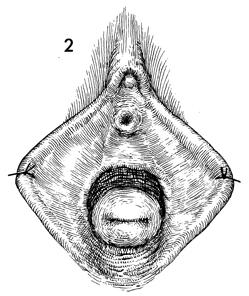
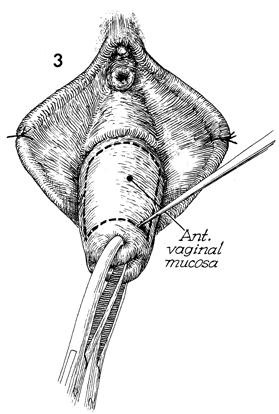
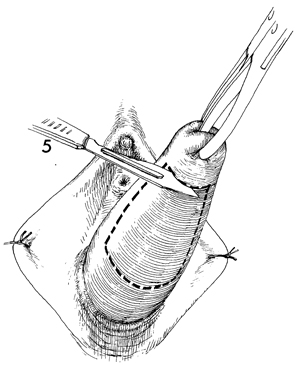
The cervix is grasped with a Jacobs
tenaculum and prolapsed from the vagina. A brilliant green marking
pen is used to outline the area of the anterior vaginal mucosa
that is to be undermined and removed. |
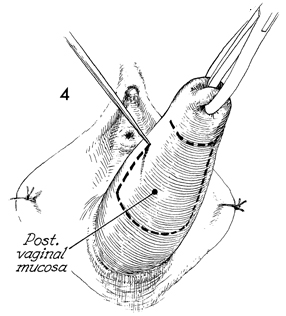
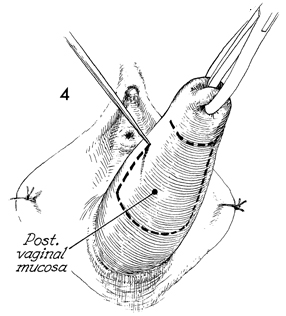
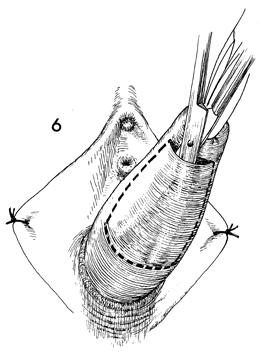
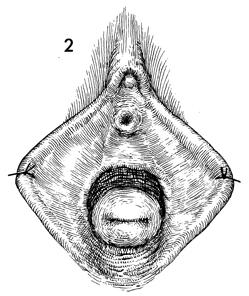
In a similar manner, a brilliant
green marking pen is used to outline the posterior vaginal mucosa. |
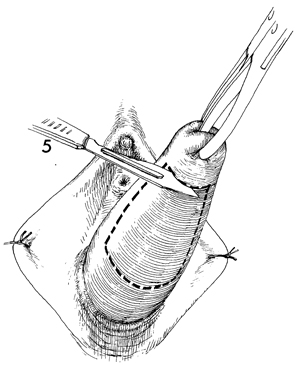
With a scalpel, the posterior vaginal
mucosa is incised transversely at its junction with the cervix. |
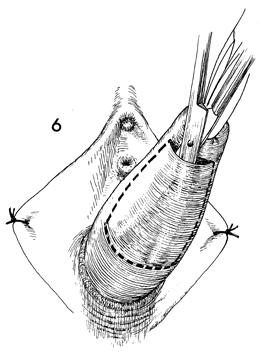
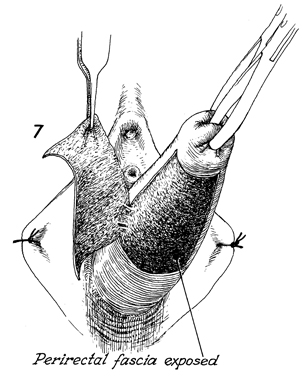
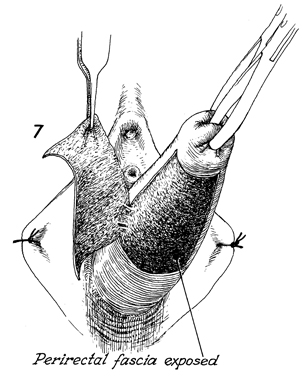
The blades of curved Mayo scissors
are inserted underneath the posterior vaginal mucosa and on top
of the perirectal fascia, and the vaginal mucosa is freed to the
lateral margins of the marked area. |
The posterior vaginal mucosa is then cut
along the prescribed marking lines with curved Mayo scissors
and removed.
|
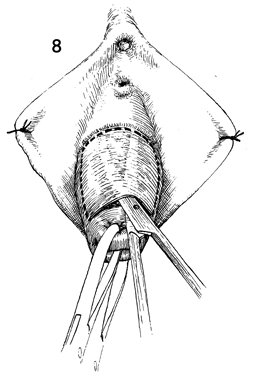
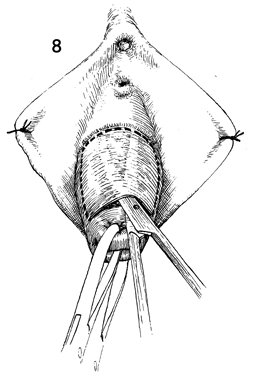
A similar transverse incision is made
in the anterior vaginal mucosa at its junction with the cervix.
The blades of curved Mayo scissors are inserted underneath the
anterior vaginal mucosa to dissect laterally and upward toward
the urethral meatus until the limits of the marked area are reached.
This procedure is facilitated if traction is held on the Jacobs
tenaculum. |
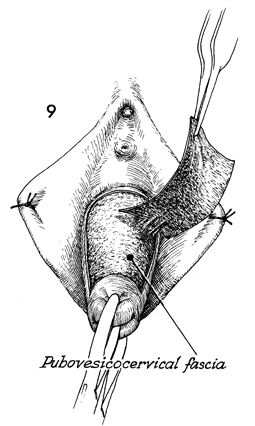
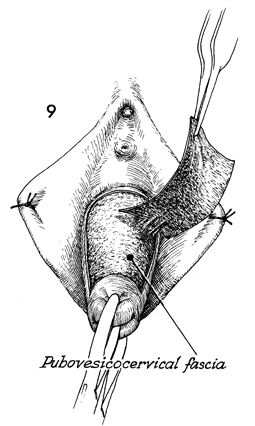
The anterior vaginal mucosa
is removed from the underlying pubovesical cervical fascia.
|
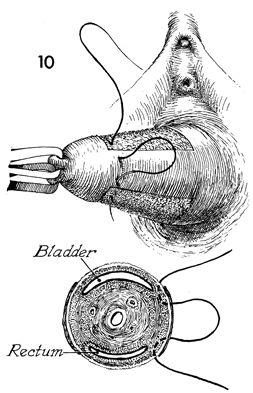
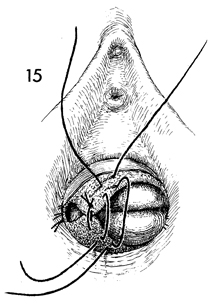
The surgeon progressively approximates
the pubovesical cervical fascia anteriorly and the perirectal fascia
posteriorly with Lembert inverting sutures. |
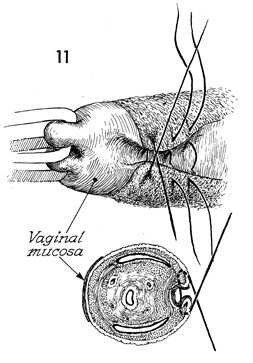
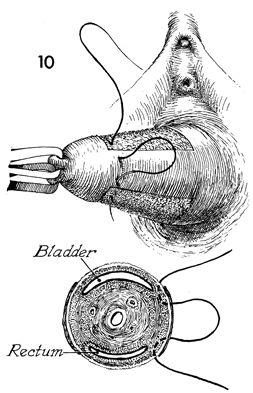
When this suture is tied, a tunnel
is created along each lateral margin for drainage of cervical mucus,
thereby preventing the formation of mucocele. The cross section
underneath Figure 11 demonstrates how this tunnel is formed. |
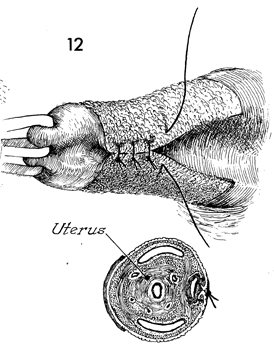
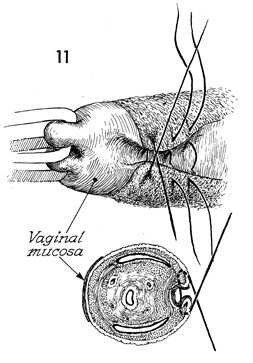
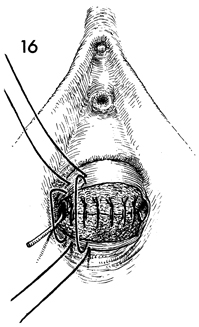
Several sutures are placed in a similar
manner to complete the tunnel. |
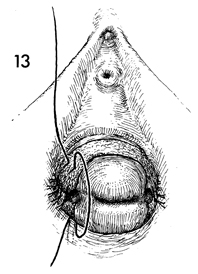
Lembert 0 absorbable sutures are placed from
the pubovesical cervical fascia anteriorly to the perirectal
fascia posteriorly over the portio of the cervix. |
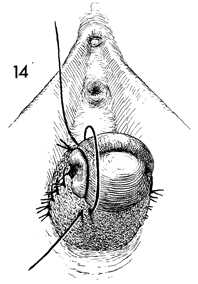
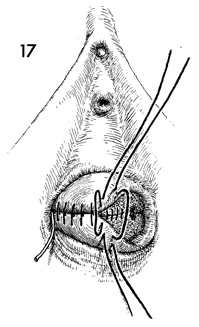
After several of these sutures have been
placed, the surgeon inverts the portio of the cervix. |
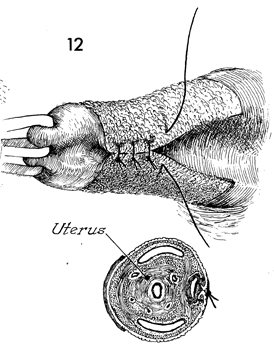
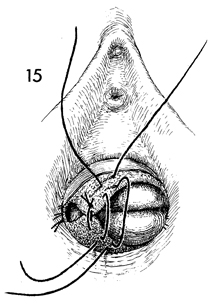
After several rows of sutures have been completed,
the cervix is totally inverted, and the pubovesical cervical
fascia anteriorly and the perirectal fascia posteriorly are plicated. |
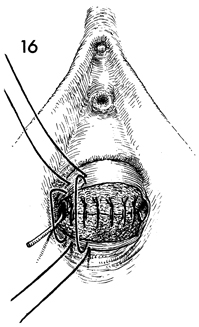
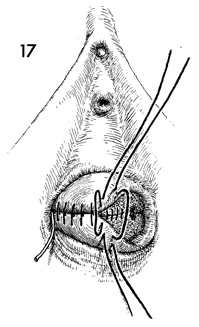
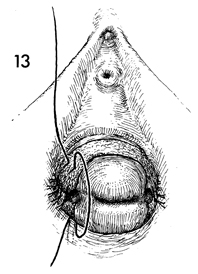
A final row of 0 synthetic absorbable sutures
is placed between the remaining vaginal mucosa anteriorly and
posteriorly. Note that a small wire probe can be inserted into
the tunnel laterally on each side. |
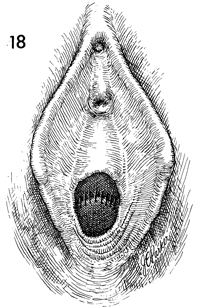
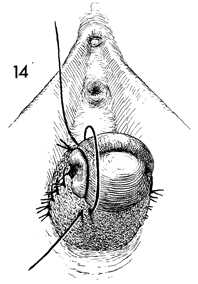
The vaginal mucosal sutures are completed.
Note that the urethra and the urethrovesical angle are not included
in the procedure and are not sutured to the posterior fourchette.
Such a procedure would distort the urethrovesical angle and in
many cases lead to postoperative urinary incontinence. |
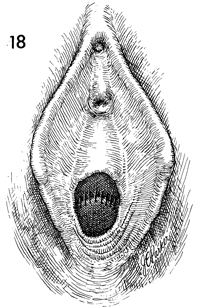
Although the finished operation leaves the
patient with a slight urethrocele or bulge, the surgeon should
make no attempt to close off the entire vagina. |