Enterocele is a hernia of the lining of the peritoneal cavity with
or without abdominal viscera. The enterocele can occur posteriorly
with or without inversion of the vagina. The enterocele should be distinguished
from a rectocele, for the procedure for surgical correction is different.
The proximity of the ureter to the uterosacral ligaments
must be noted, and care must be taken not to include it when approximating
the uterosacral ligaments. Finally, care must be taken to depress the
rectum so that it is not incorporated into the plication of the levator
muscles.
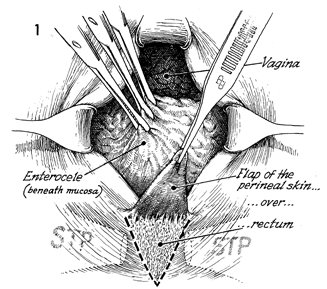
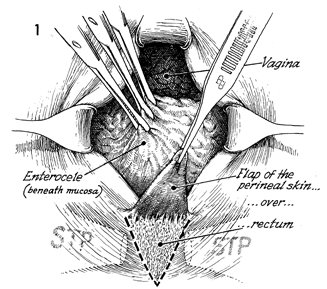
The patient should be placed in the
dorsal lithotomy position and prepped and draped in the usual manner
for pelvic surgery. At this point, an accurate diagnosis should
be made as to whether the patient has an enterocele alone or an
enterocele associated with a rectocele. STP identifies the superficial
transverse perineal muscle. |
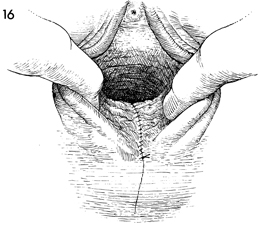
By excising an edge of perineal
body skin at the fourchette, the surgeon carries the triangle
up over the posterior fourchette into the posterior vaginal mucosa
and converts the triangle to a diamond-shaped defect. The Allis
clamps on the vaginal mucosa over the rectocele are elevated
by an assistant. |
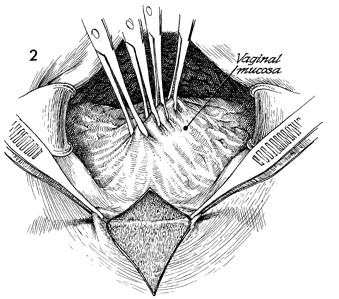
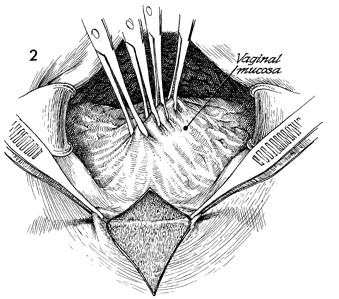
The posterior vaginal mucosa is
undermined by curved Mayo scissors and opened in the midline.
The edges of the vaginal mucosa are grasped with T-clamps and
held on traction. It is essential that the assistant create a
triangle for the surgeon by elevating the Allis clamps on the
posterior vaginal mucosa upward and the T-clamps on the edge
of the vaginal mucosa downward. The incision in the posterior
vaginal mucosa should be carried up to the vaginal apex and should
expose the sac of the enterocele. |
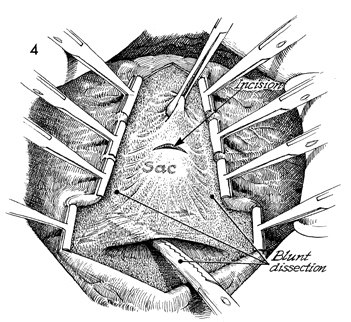
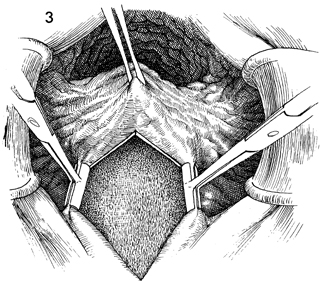
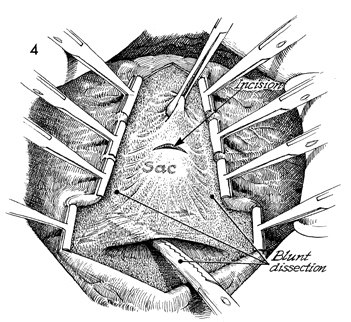
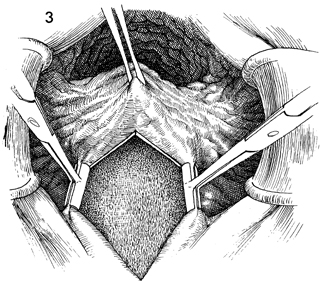
When the entire
posterior vaginal mucosa has been opened, the sac of the enterocele
is identified and grasped with an Allis clamp. Blunt dissection
is carried out to remove the perirectal fascia from the posterior
vaginal mucosa so that the sac of the enterocele can be clearly
identified. A small incision is made into the sac. |
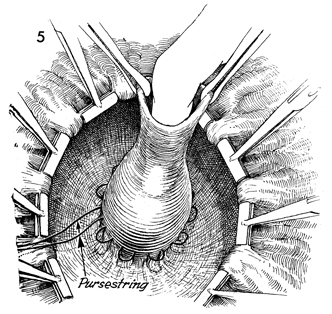
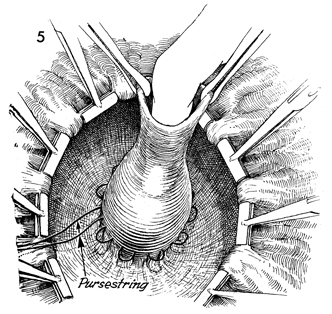
A finger is immediately inserted
into the opening of the sac, and the intestinal contents are
identified and displaced back into the abdomen. A pursestring
suture of 0 synthetic absorbable suture is placed around the
neck of the enterocele sac. |
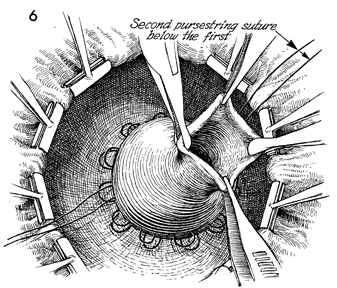
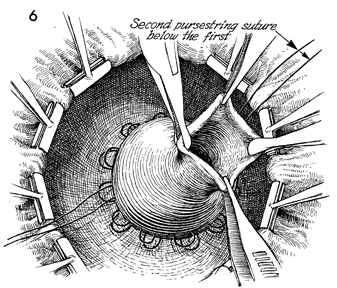
A second pursestring
suture of 0 synthetic absorbable suture is placed around the
neck of the enterocele sac. |
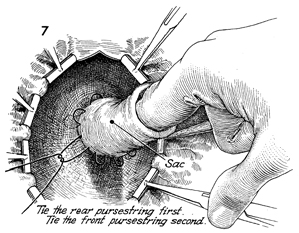
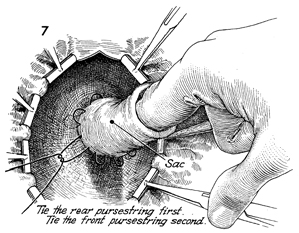
Before either of these sutures is
tied, a finger should again be inserted into the sac to displace
any intestinal contents back into the abdomen. The rear pursestring
suture should be tied first; then the front pursestring suture
should be tied. |
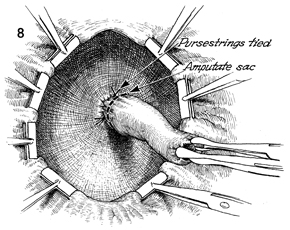
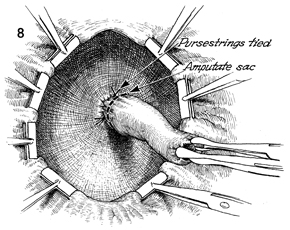
High ligation of the sac has been
completed, and the sac can now be removed. |
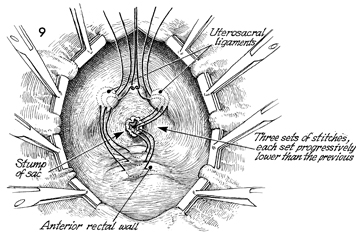
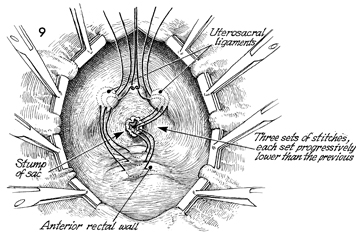
The stump of the sac is seen. The uetrosacral
ligaments and the anterior rectal wall are identified. Three
sets of 0 synthetic absorbable sutures should be placed between
the anterior rectal wall, the stump of the enterocele sac, and
the uretrosacral ligaments. Each suture is placed progressively
lower in the genital canal than the previous one. Each suture
is held on hemostats until all are placed; then each is progressively
tied. |
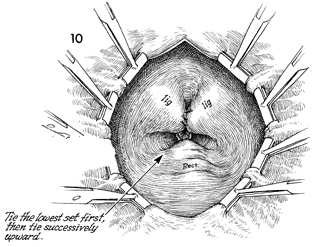
Uterosacral ligaments,
the stump of the amputated sac of the enterocele, and the anterior
rectal wall have all been plicated. The development of any future
enterocele is unlikely. |
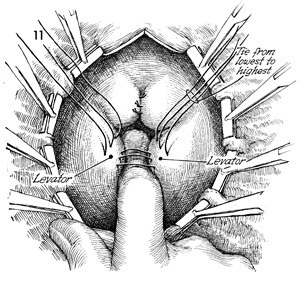
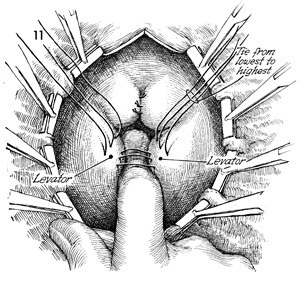
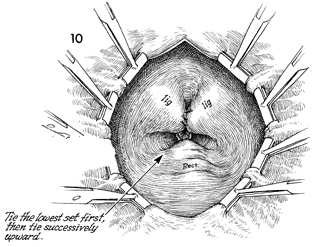
Attention can now be directed toward repair
of the rectocele if present. A finger is inserted in the midline,
depressing the rectum and exposing the levator muscles. Zero
synthetic absorbable sutures should be placed in the levators
and held prior to tying. After all sutures have been progressively
placed in the levators, they should be tied from the lowest suture
in the genital canal, placed first, to the uppermost suture,
placed last. |
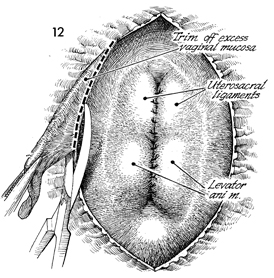
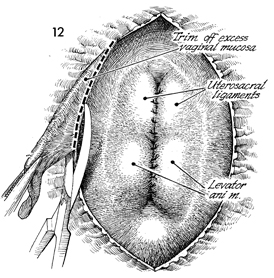
Excessive vaginal mucosa is trimmed away. |
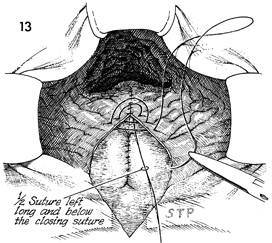
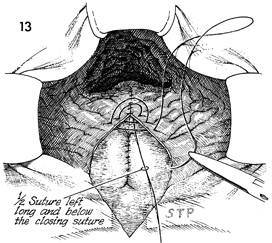
A 0 synthetic absorbable suture is used in
a running fashion to close the posterior vaginal mucosa. Note
how the long end of the suture is left in place from the apex
of the closure. Each suture is carefully placed above this suture;
care is taken not to entrap the suture with another bite of the
running stitch. STP identifies the superficial transverse perineal
muscle. |
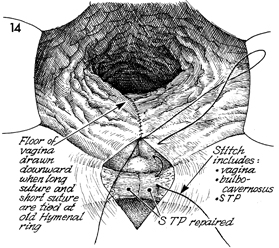
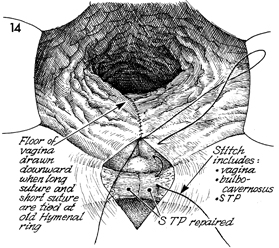
The entire posterior vaginal vault wall down
to the hymenal ring has been closed. At this point, the suture
is tied. Note that the free end of the original suture placed
at the apex remains. By tying the free end of the suture left
after the vaginal mucosa has been closed down to the hymenal
ring, the surgeon draws the apex of the posterior vaginal mucosa
against the levator muscles and eliminates dead space. After
tying the running suture in the posterior vaginal mucosa at the
hymenal ring, the surgeon inserts the needle behind the hymen
into the vagina and brings it out through the insertion of the
bulbocavernosus muscle.
At this point, plication of
the superficial transverse perineal muscle (STP) is made by several
interrupted 0 synthetic absorbable sutures. The insertion of
the bulbocavernosus muscle is plicated in the midline, incorporating
a suture into the superficial transverse perineal muscle to completely
reconstruct the perineal body. |
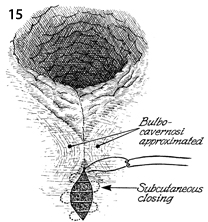
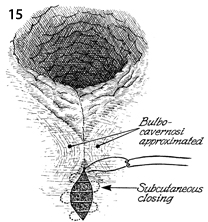
The bulbocavernosi muscles are approximated
in the midline by the running suture. The skin of the perineal
body is approximated by a subcuticular suture. |
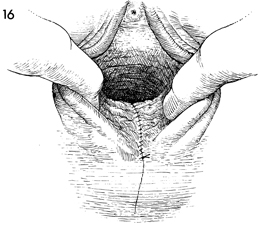
The reconstructed vaginal vault and perineal
body are shown. |
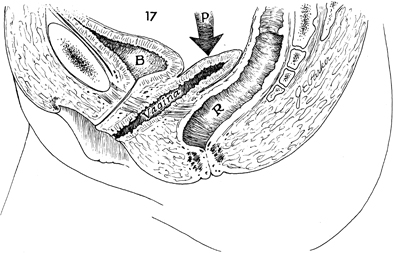
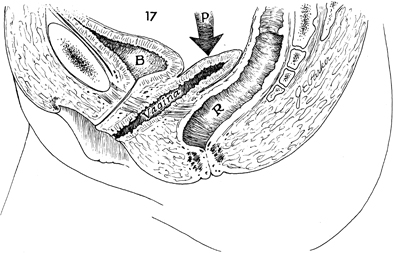
A sagittal view shows how the direction of
intra-abdominal pressure is now applied to the anterior vaginal
wall. Note how the cul-de-sac has been obliterated by the suturing
together of the posterior vaginal wall, pelvic peritoneum (P), anterior
rectal wall, and uterosacral ligaments. This line of pressure
is directed away from the genital hiatus in the levator plate,
reducing the possibility of recurrent prolapse. B, bladder;
and R, rectum. |