Vagina
and Urethra
Anterior Repair and Kelly
Plication
Site Specific Posterior Repair
Sacrospinous
Ligament Suspension of the Vagina
Vaginal Repair of Enterocele
Vaginal Evisceration
Excision of
Transverse Vaginal Septum
Correction of
Double-Barreled Vagina
Incision
and Drainage of Pelvic Abscess via the Vaginal Route
Sacral Colpoplexy
Le Fort Operation
Vesicovaginal Fistula
Repair
Transposition
of Island Skin Flap for Repair of Vesicovaginal Fistula
McIndoe Vaginoplasty
for Neovagina
Rectovaginal Fistula
Repair
Reconstruction of
the Urethra
Marsupialization
of a Suburethral Diverticulum by the Spence Operation
Suburethral
Diverticulum via the Double-Breasted Closure Technique
Urethrovaginal
Fistula Repair via the Double-Breasted Closure Technique
Goebell-Stoeckel
Fascia Lata Sling Operation for Urinary Incontinence
Transection
of Goebell-Stoeckel Fascia Strap
Rectovaginal
Fistula Repair via Musset-Poitout-Noble Perineotomy
Sigmoid
Neovagina
Watkins Interposition Operation |
Sacrospinous
Ligament Suspension of the Vagina
Sacrospinous ligament suspension of a prolapsed vagina
is an ideal procedure for a sexually active woman who has a complete
prolapse of the vaginal canal. Prolapse of the vagina can occur following
a hysterectomy or can evolve with the uterus in place. If the uterus
is still in place, it is best to remove it by vaginal hysterectomy,
as shown in the section Uterus. The sacrospinous ligament suspension
operation has the advantage of retaining an adequate length and width
of the vaginal canal.
Physiologic Changes. Total prolapse of the vagina
may interfere with bladder function, defecation, and sexual intercourse.
Some women with total prolapse of the vagina have no evidence of urinary
incontinence. There are, however, some women who after correction of
the prolapse may experience urinary incontinence unless certain surgical
techniques are employed to ensure that the intravesical pressure does
not exceed the intraurethral pressure, other than in the act of micturition.
After suspension of the prolapsed vagina, rectal function should improve,
and the patient should be able to defecate without digital manipulation
of the rectum. Comfortable sexual intercourse can be achieved if the
vagina is of adequate length and diameter and if the vaginal outlet
has not been constricted.
Points of Caution. To achieve a safe
and permanent sacrospinous ligament suspension of the vagina, there
must be appropriate attention to detail. The rectovaginal space must
be entered and dissected prior to entering the pararectal space through
the vagina. If the lateral extent of the cardinal ligament is inadvertently
entered, copious hemorrhage can occur from the hypogastric venous plexus
that resides in the upper two-thirds of this area (the web).
The sacrospinous
ligament must be visualized and identified. Failure to place sutures
directly into the ligament is the most common cause of recurrent prolapse.
Care must be taken to avoid the pudendal artery and nerve, since these
are immediately posterior and inferior to the ischial spine. The sutures
must be placed at least 2 cm medial to the ischial spine to avoid injury
to the pudendal nerve, which could result in chronic pain. The type
of suture material used must be carefully chosen to avoid recurrence.
We prefer a synthetic nylon suture mounted on a small Mayo needle or
a Deschamps ligature carrier for placement.
Technique
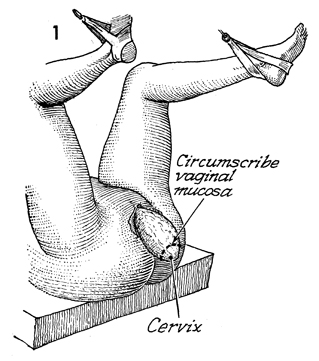
The patient is placed in the dorsal lithotomy
position and is prepped and draped in the usual manner.
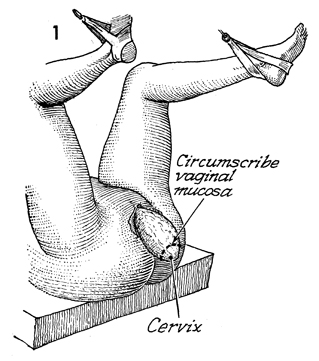
If the patient has not had a hysterectomy,
the procedure is started by circumscribing the vaginal mucosa
at the junction of the cervix and vagina in the routine manner
for starting a vaginal hysterectomy. |
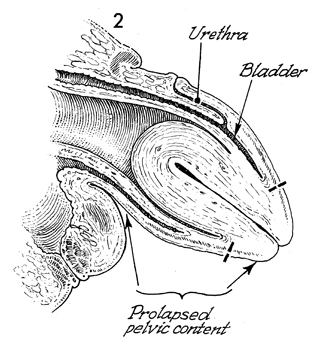
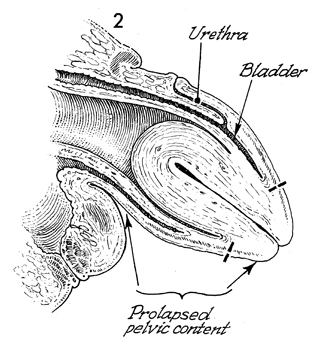
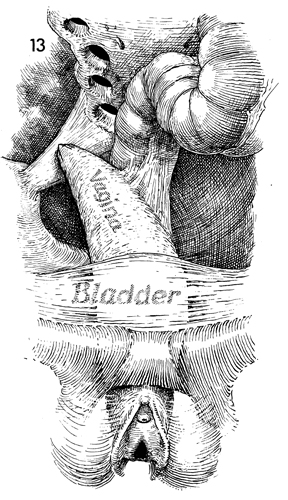
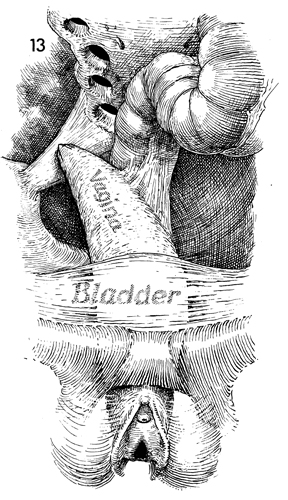
A sagittal view of total prolapse
of the urethra, bladder, uterus, and rectum is shown. The vaginal
hysterectomy is completed at this point according to the technique
shown in the section Uterus. |
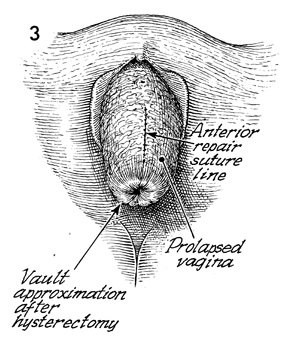
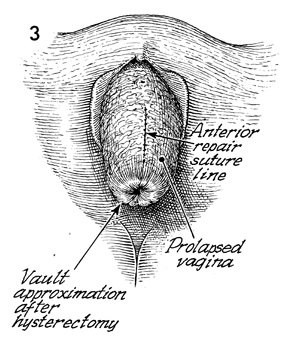
A perineal view of total prolapse of the
vagina following the vaginal hysterectomy and anterior repair
is shown. |
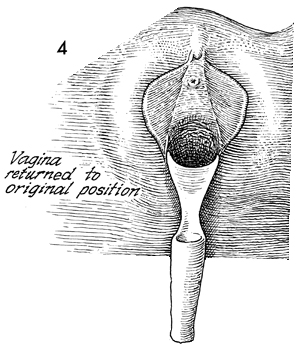
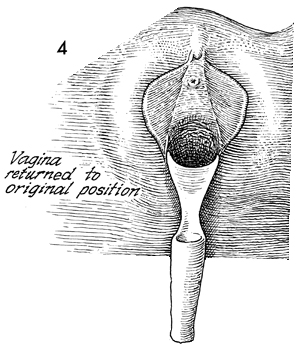
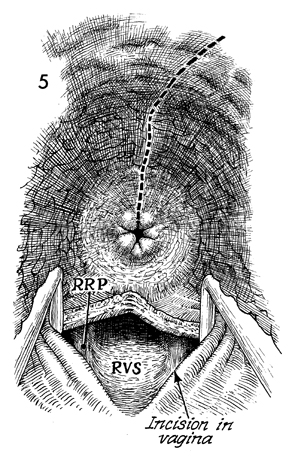
The prolapsed vagina is
returned to its original position. |
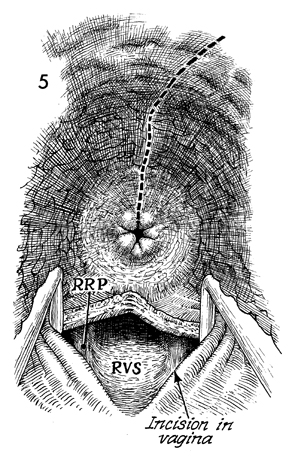
The suture line can be seen
in the anterior vaginal mucosa following the anterior repair.
The posterior vaginal mucosa is opened in the routine fashion
as described previously in Posterior Repair. A finger is inserted
through the incision in the posterior vaginal mucosa, dissecting
out the rectovaginal space (RVS). The rectal pillars
on both sides can be immediately identified. The right rectal
pillar (RRP) is
identified. The rectal pillar can be bluntly perforated either
with the finger or with the tip of a long Kelly clamp. |
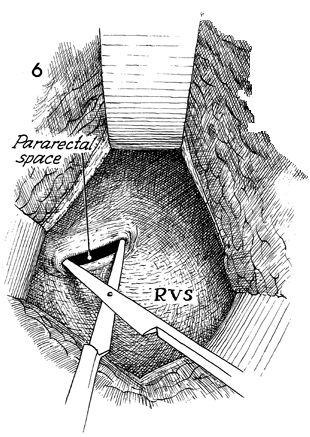
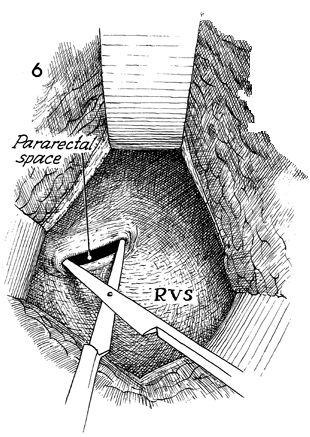
A Breisky-Navratil retractor
is ideal for exposing the rectovaginal space in order to enter
the pararectal space. The narrow Deaver retractor may also be
used, but the curve of the Deaver retractor is less effective
than that of the Breisky-Navratil retractors. Adequate retraction
of the cardinal ligament, vagina, and rectum is essential for
safe operative exposure. Visualization and illumination can be
achieved by a bright fiberoptic head lamp focused onto the pararectal
space. |
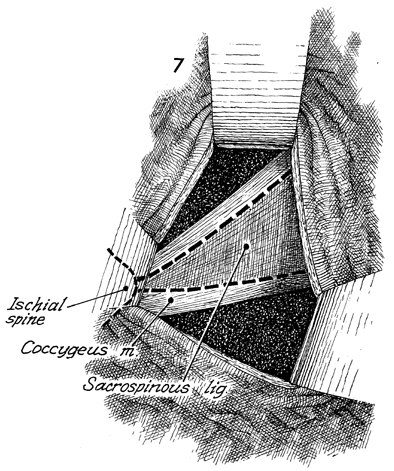
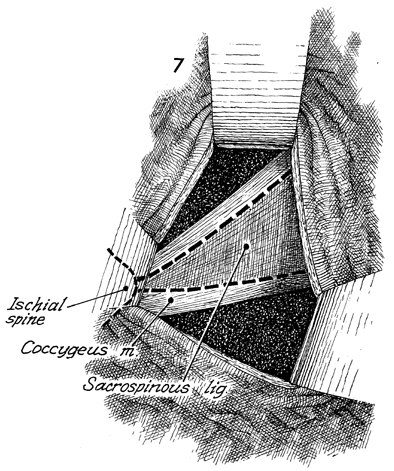
With
long thin retractors, the surgeon displaces the rectum to the
left and the cardinal ligament and ureter anteriorly. A narrow
right-angle retractor is used to displace the side walls of
the pelvis and perineum. The superior surface of the pelvic
diaphragm is exposed. A sponge dissector is used to bluntly
dissect the sacrospinous ligament. It is important for the
surgeon to remove the areolar tissue from the surface of the
right sacrospinous ligament in order to visualize it directly.
The ischial spine should be palpated directly,
and a zone approximately 2 cm medial to the spine should be selected
for insertion of the suture needle. |
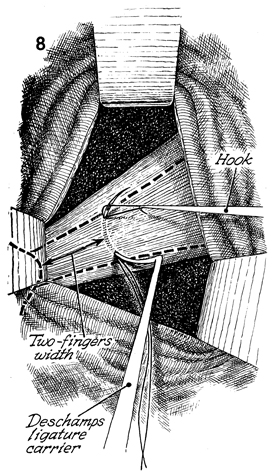
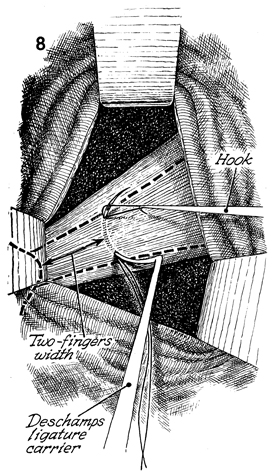
The Deschamps ligature carrier, loaded with
a 0 monofilament nylon suture, can be
inserted directly into the ligament. The suture is grasped with
a skin hook and held while the Deschamps carrier is removed.
If the suture is placed too close to the ischial spine, it may
entrap the pudendal nerve. |
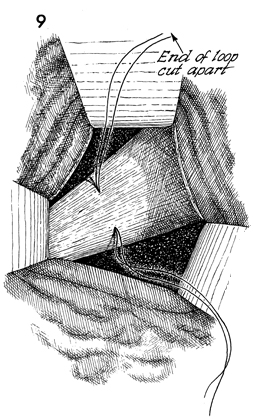
A second suture is loaded into the Deschamps
ligature carrier and passed through the sacrospinous ligament
in a similar manner. |
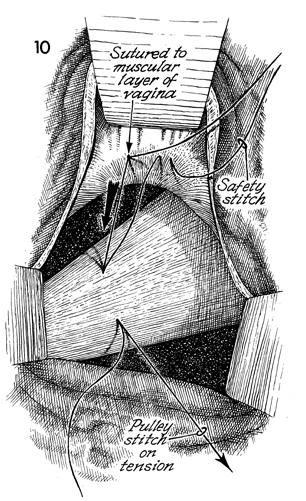
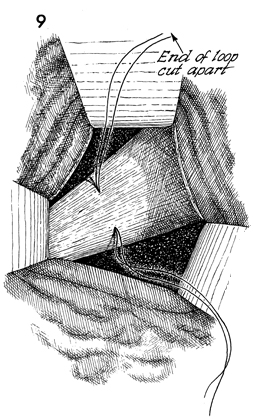
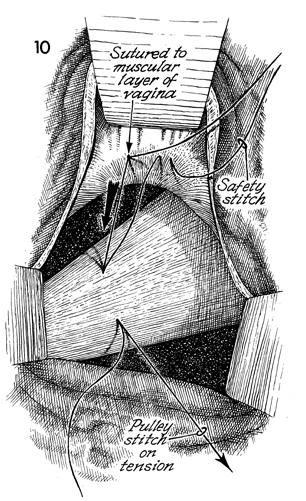
One end of the suture previously inserted
through the sacrospinous ligament is placed through the muscular
layer of the vagina. In a similar manner, the second suture is
placed. The opposite end of the suture in the sacrospinous ligament
is left free and held on a small hemostat. Traction on this suture
will draw the vaginal vault directly to the ligament, where a
square knot will promptly affix it to the sacrospinous ligament. |
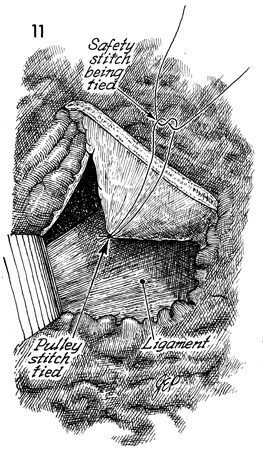
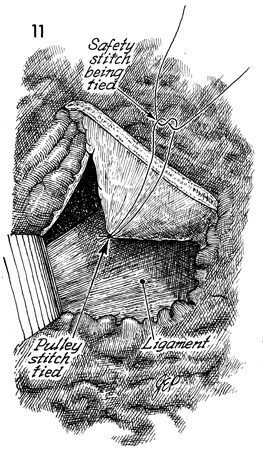
The pulley stitch has been tied, and the
ends of the suture have been cut. The safety stitch is then tied. |
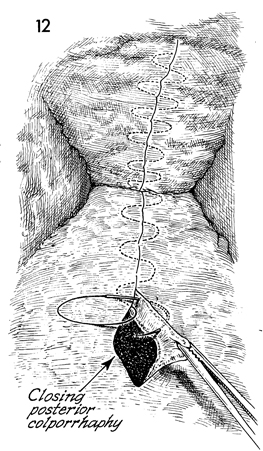
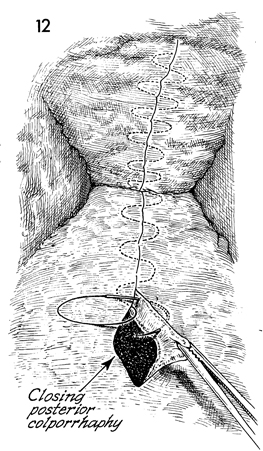
A posterior colporrhaphy is carried out in
the routine fashion, and the vaginal mucosa is closed. |
The completed sacrospinous ligament suspension
with the apex of the vagina suspended from the sacrospinous ligament
approximately 2 cm from the ischial spine is shown.
A Foley catheter is inserted into the bladder
and left for a minimum of 4 days. Thereafter, management of bladder
function is similar to that following surgery for urinary incontinence.
No vaginal packs or drains are used.
|
|
|