Vagina
and Urethra
Anterior Repair and Kelly
Plication
Site Specific Posterior Repair
Sacrospinous
Ligament Suspension of the Vagina
Vaginal Repair of Enterocele
Vaginal Evisceration
Excision of
Transverse Vaginal Septum
Correction of
Double-Barreled Vagina
Incision
and Drainage of Pelvic Abscess via the Vaginal Route
Sacral Colpoplexy
Le Fort Operation
Vesicovaginal Fistula
Repair
Transposition
of Island Skin Flap for Repair of Vesicovaginal Fistula
McIndoe Vaginoplasty
for Neovagina
Rectovaginal Fistula
Repair
Reconstruction of
the Urethra
Marsupialization
of a Suburethral Diverticulum by the Spence Operation
Suburethral
Diverticulum via the Double-Breasted Closure Technique
Urethrovaginal
Fistula Repair via the Double-Breasted Closure Technique
Goebell-Stoeckel
Fascia Lata Sling Operation for Urinary Incontinence
Transection
of Goebell-Stoeckel Fascia Strap
Rectovaginal
Fistula Repair via Musset-Poitout-Noble Perineotomy
Sigmoid
Neovagina
Watkins Interposition Operation |
Goebell-Stoeckel
Fascia Lata Sling Operation for Urinary Incontinence
Surgery for stress incontinence of urine has a long history of numerous
procedures designed to relieve patients of this disabling problem.
There are procedures that reinforce the pubovesical fascia beneath
the urethra, procedures that tack the urethra up to the rectopubic
space, and procedures that elevate the urethrovesical angle by a suspension
from the rectus fascia.
Long-term results reveal an interesting statistic.
Most surgical procedures to correct all forms of urinary incontinence
have a success rate of approximately 40-90%.
There are two ways to alter
the anatomy and thus change the physiology to correct stress incontinence
of urine. First, there are operations designed to increase the intraurethral
pressure so that it exceeds the intravesical pressure in the resting
and stress state. These include the Goebell-Stoeckel fascia lata sling,
anterior repair with Kelly plication, Sexton perivaginal suspension,
and the modified Marshall-Marchetti procedure in which the periurethral
vaginal tissue is suspended from the conjoined tendon. Other procedures,
such as the Marshall-Marchetti-Krantz operation, attempt to relieve
urinary stress incontinence by making the vesical neck of the bladder
an intra-abdominal organ.
The procedure
demonstrating the best long-term result in our clinic is the Goebell-Stoeckel
fascia lata sling.
We have used the Goebell-Stoeckel fascia lata sling
in cases of primary stress incontinence of urine in elderly nulliparous
patients, obese patients, and patients with congenital absence or traumatic
loss of the urethra in conjunction with a primary reconstructive procedure
to rebuild a urethra. In addition, we have used the Goebell-Stoeckel
fascia lata sling for those cases of secondary stress incontinence
of urine after an attempt to relieve the problem with one of the other
surgical procedures has failed.
The operation is intended to relieve
stress incontinence of urine.
Physiologic Changes. In this operation, the intraurethral
pressure is elevated above the intravesical pressure by reducing the
diameter of the urethral lumen. The increase in intraurethral pressure,
however, should not be greater than the intravesical pressure at the
moment of maximum detrusor contraction with normal voiding.
Points of Caution. There are several points of caution
to observe in performing this operation. (1) The vaginal dissection
at the urethrovesical angle should extend up behind the pubic bone
to the level of the urogenital diaphragm so that the abdominal dissection
down behind the symphysis pubis may be performed with blunt finger
dissection only. In this way, the chance of inadvertently entering
the bladder will be reduced. (2) The fascia strap should not be pulled
too tightly. The strap should be loose enough to allow easy insertion
of a Kelly clamp between the strap and the urethral vesical angle.
When the strap is pulled too tightly, the patient will have postoperative
urinary retention.
Technique

The patient is placed in the dorsal
lithotomy position and examined under anesthesia. The degree
of cystourethrocele is assessed. |
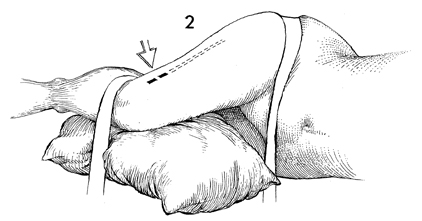
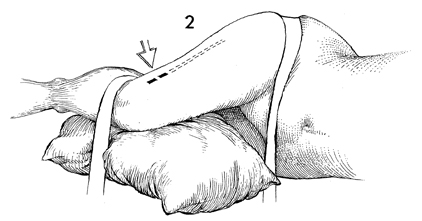
The patient is changed to the right
or left lateral decubitus position with flexion of both the hip
and the knee at approximately 60°. A pillow should be
placed between the knees in order to elevate the thigh to a level
position. Two large pieces of tape are used to stabilize the
patient and prevent her from moving to either side. The lateral
thigh is prepped and draped. The solid line marks the
site of the initial incision, and the dotted line marks
the direction of the incision in the fascia lata. |

The Masson fascia stripper consists
of two hollow metal tubes-one inside the other. The inner tube
has a narrow opening near one end; the edge of the outer tube
is sharpened to allow cutting of the fascia strip at the desired
level. |
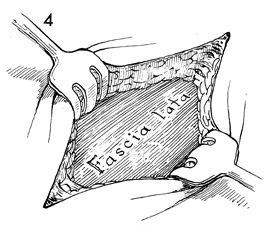
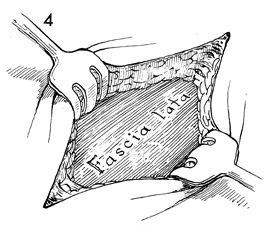
A longitudinal incision of 5 cm
is made approximately 4 cm above the knee. This incision is carried
down to the fascia lata. Small rake retractors are used to expose
the fascia lata. |
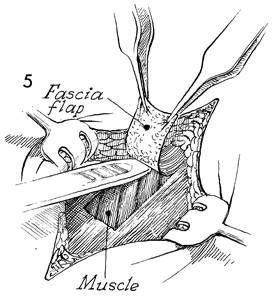
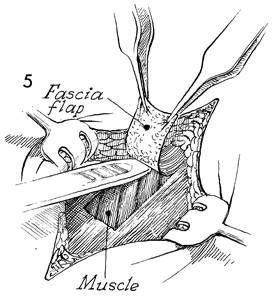
The strap is started with the scalpel
blade and should be approximately 3 cm wide. It is dissected
off the muscle and the subcutaneous fat for a distance of at
least 10-12 cm with the handle of the knife and index finger. |
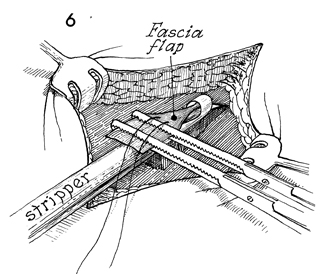
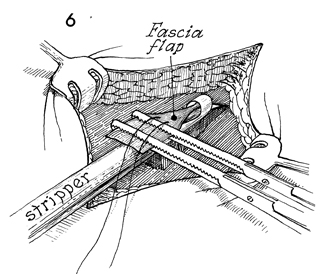
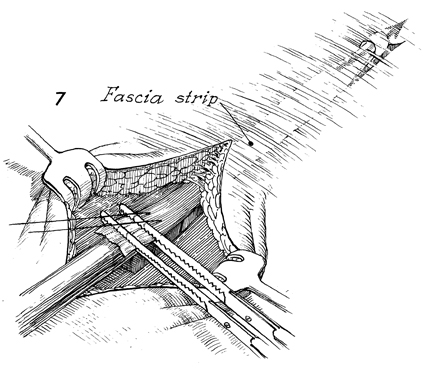
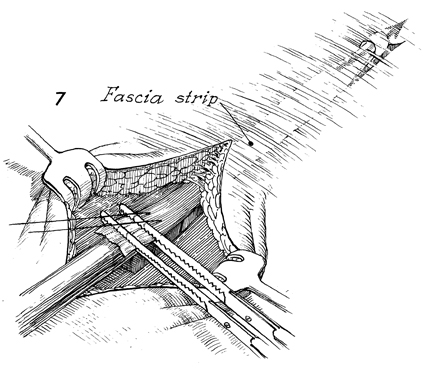
The hand-carved portion of the strap
is fed through the eye of the inner tube of the Masson fascia stripper.
A 2-0 suture is placed through the fascia at the level of the eye
to be used as a retriever in case the strap is inadvertently cut
up inside the thigh. Two straight Kocher clamps are applied to
the end of the strap for countertraction. The outer tube of the
Masson fascia stripper is inserted over the inner tube, and they
are locked together with a bolt action. |
With countertraction on the
two Kocher clamps placed across the end of the strap, the Masson
fascial stripper is advanced up the fascia lata until the desired
length of fascia is obtained. At that point, the outer tube of
the Masson fascia stripper is disengaged from the inner tube,
and with a sudden shearing motion the inner tube is withdrawn
from the outer tube, cutting the proximal end of the fascia strap. |
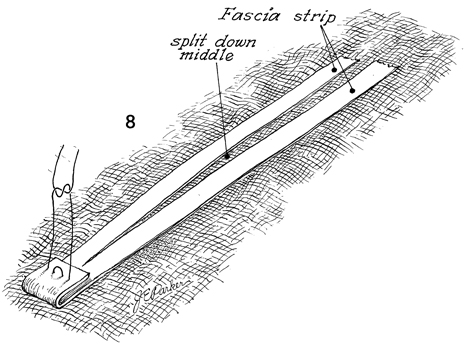
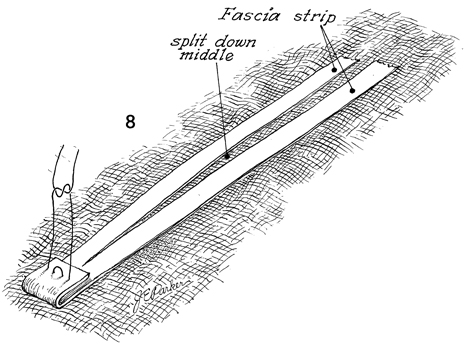
On occasion, the fascia strap
will be too short, particularly in obese patients. Therefore,
one end of the strap may be folded on itself, and several interrupted
2-0 Prolene sutures will need to be placed to anchor it. From
the opposite end, and incision can be made down the length of
the strap, thereby doubling the overall length. |
The incision in the thigh is closed with
two layers-the inner layer with 3-0 synthetic absorbable suture
and the outer layer with fine monofilament suture such as nylon
or Prolene. |
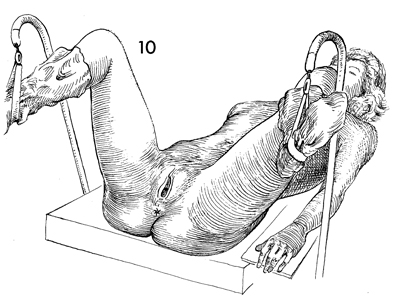
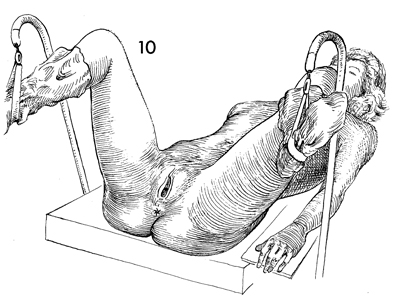
The patient is now changed from the lateral
decubitus position to the dorsal lithotomy position. The vulva,
vagina, and lower abdomen are prepped and draped. |
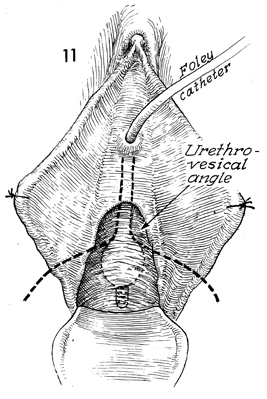
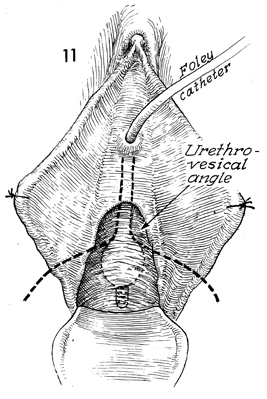
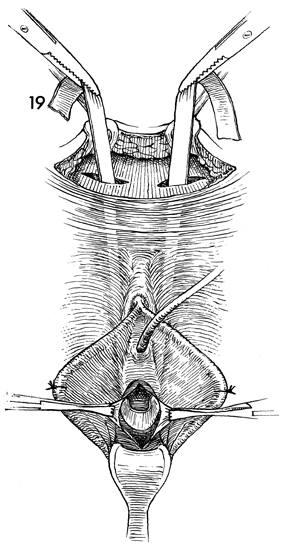
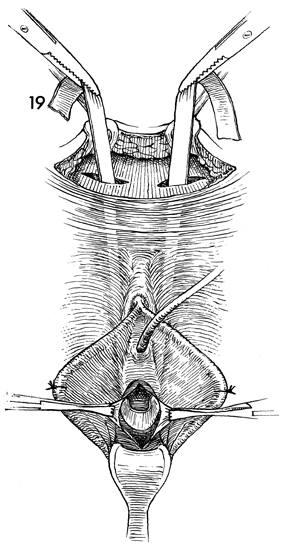
With the labia minora tacked to the perineum
with interrupted sutures, a Foley catheter is inserted into the
bladder, and tension is applied to define the urethrovesical
angle. |
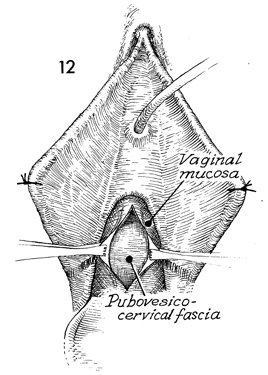
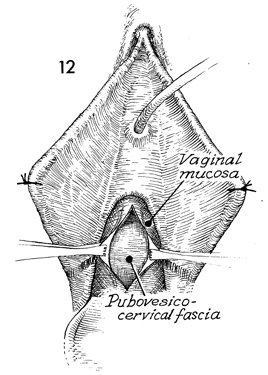
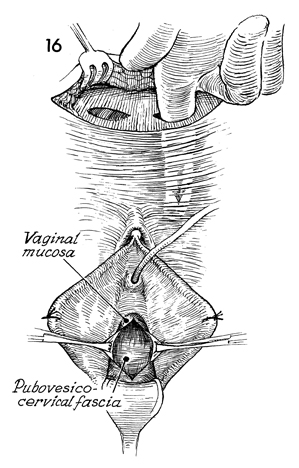
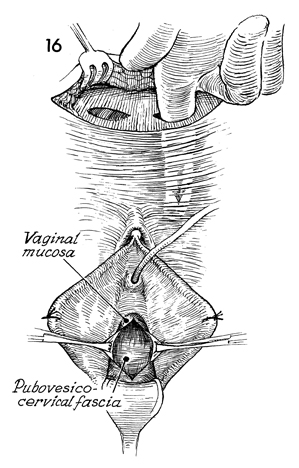
Two Allis clamps are applied at the urethrovesical
angle, and a linear incision is made in the vaginal mucosa. This
is carried down to the pubovesical cervical fascia. |
After sharp dissection has separated the
vaginal mucosa from the pubovesical cervical fascia, blunt dissection
with the finger can usually be carried out without difficulty
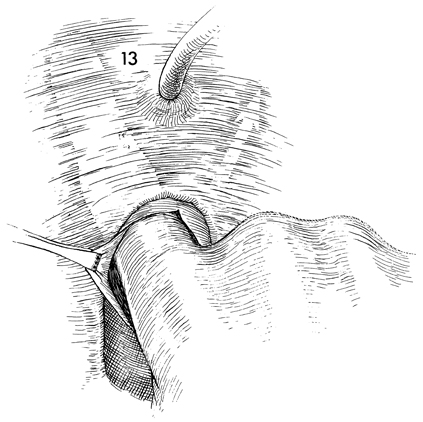
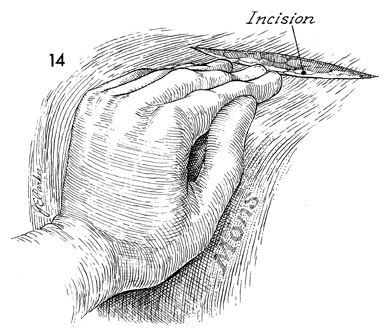
lateral to the urethra up to the urogenital diaphragm. The same
dissection should be carried out on the opposite side. |
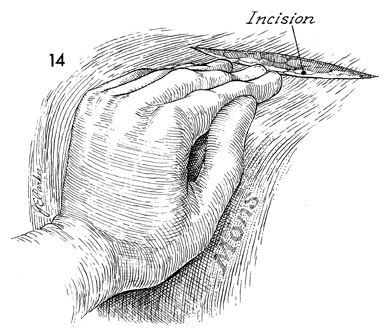
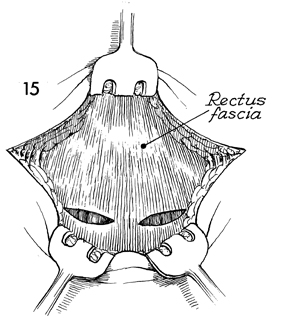
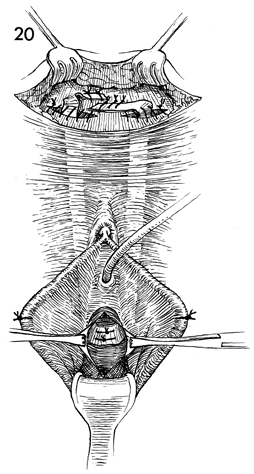
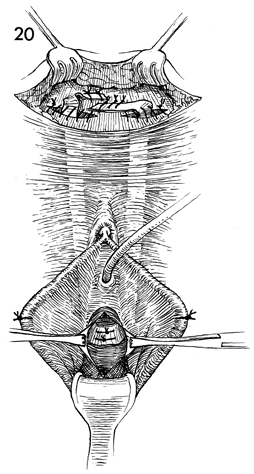
The surgeon should make an 8-cm transverse
incision approximately 8 cm above the pubic bone. |
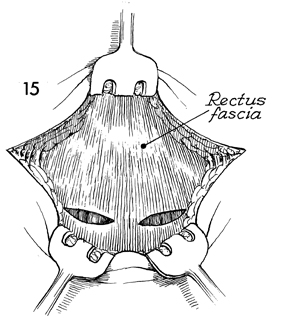
This incision should be carried down to the
rectus fascia, and two small oblique incisions large enough to
admit a finger should be made in the rectus fascia. |
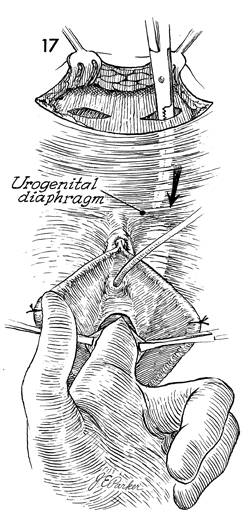
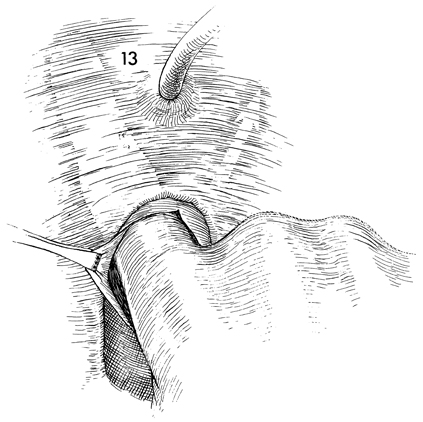
Blunt dissection with a finger is used to
create a space behind the pubic bone down to the urogenital diaphragm
lateral to the urethra. |
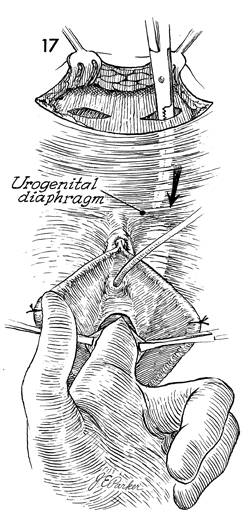
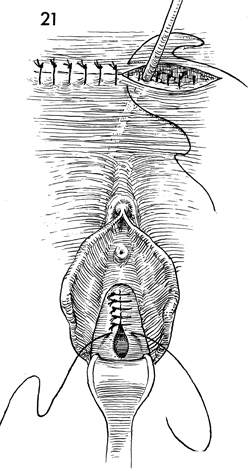
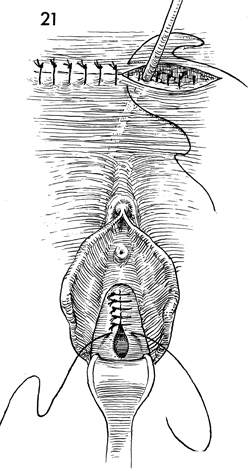
A finger is inserted through the vaginal
mucosa lateral to the urethra and up to the urogenital diaphragm.
At the same time, a large Kelly clamp can be inserted through
the rectus incision down to the point where it touches the finger. |
The Kelly clamp
is then pushed through the urogenital diaphragm and out into
the vagina. The clamp is used to grasp one end of the fascia
strap. |
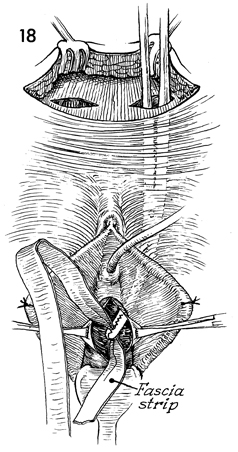
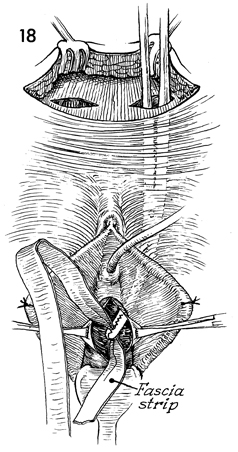
The strap is pulled up to the rectus abdominis
incision and held with a small hemostat. A similar technique
of dissection and strap pull-through is performed on the opposite
side. A strap now is through both incisions in the rectus fascia
and is around the urethrovesical angle.
Tension on the strap is adjusted
so that there is enough space between the urethrovesical angle
and the strap to easily insert a Kelly clamp. |
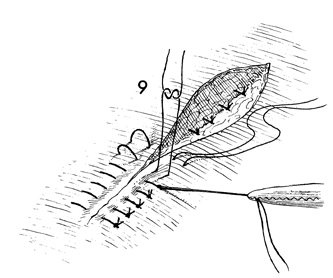
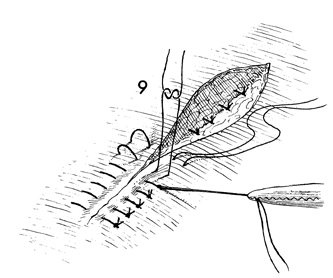
At this point, two 3-0 synthetic absorbable
sutures are placed between the strap and the pubovesical cervical
fascia at the urethrovesical angle. In addition, sutures are
placed in the strap and rectus fascia. |
A suprapubic Foley catheter
is inserted in the bladder as shown in Bladder and Ureter. The
abdominal incision is closed in layers; the vaginal mucosa is
closed with interrupted 0 synthetic absorbable suture. The Foley
catheter is left in place for at least 5 days, after which clamping
of the catheter is started and the patient is encouraged to void. |
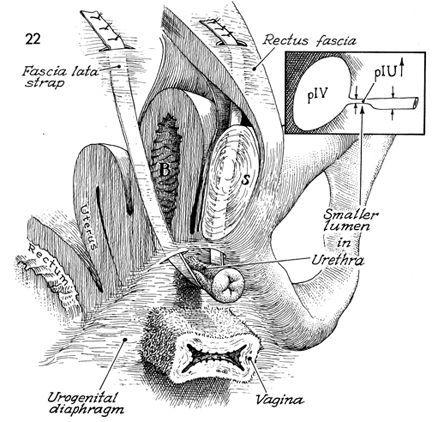
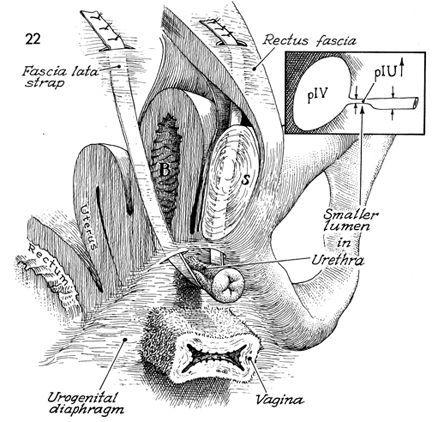
Figure 22 shows the physiologic
changes in the anatomy that allow the Goebell-Stoeckel fascia
lata sling procedure to correct urinary incontinence.
The central alteration in the anatomy
is a reduction in size in the proximal and middle third of the
urethral lumen, as noted in the insert to Figure 22 of
the bladder and urethra. Continence is achieved by elevating the
pressure inside this area above the pressure inside the bladder (B).
S identifies
the symphysis pubis.
It is important to note that unlike
the retropubic "pin-up operations" (Marshall-Marchetti-Krantz,
Burch, and Tenagho), the Goebell-Stoeckel fascia lata sling procedure
does not make the bladder into an intra-abdominal organ. Instead,
it increases the intra-urethral pressure (pIU) so
that it becomes higher than the intravesical pressure (pIV) except
when, on command, there is massive contraction of the detrusor.
Figure
22 illustrates a key point in this procedure. If the fascia strap
is pulled too tightly, the chance of postoperative urinary retention
will be greater than 30%. This is not a procedure to correct pelvic
prolapse. The strap should not be used to bring the bladder back
to an intra-abdominal organ like the Marshall-Marchetti-Krantz,
Burch, and Tenagho procedures. Failure to recognize this point
results in an unacceptable level of postoperative urinary retention. |
|