Vagina
and Urethra
Anterior Repair and Kelly
Plication
Site Specific Posterior Repair
Sacrospinous
Ligament Suspension of the Vagina
Vaginal Repair of Enterocele
Vaginal Evisceration
Excision of
Transverse Vaginal Septum
Correction of
Double-Barreled Vagina
Incision
and Drainage of Pelvic Abscess via the Vaginal Route
Sacral Colpoplexy
Le Fort Operation
Vesicovaginal Fistula
Repair
Transposition
of Island Skin Flap for Repair of Vesicovaginal Fistula
McIndoe Vaginoplasty
for Neovagina
Rectovaginal Fistula
Repair
Reconstruction of
the Urethra
Marsupialization
of a Suburethral Diverticulum by the Spence Operation
Suburethral
Diverticulum via the Double-Breasted Closure Technique
Urethrovaginal
Fistula Repair via the Double-Breasted Closure Technique
Goebell-Stoeckel
Fascia Lata Sling Operation for Urinary Incontinence
Transection
of Goebell-Stoeckel Fascia Strap
Rectovaginal
Fistula Repair via Musset-Poitout-Noble Perineotomy
Sigmoid
Neovagina
Watkins Interposition Operation |
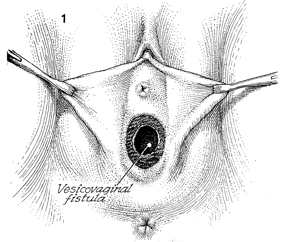
Transposition of Island Skin Flap for Repair
of Vesicovaginal Fistula
Vesicovaginal fistulae that have occurred secondary to irradiation
and/or have recurred after repeated attempts to close them must be
treated with procedures beyond the ordinary. In such cases, an island
skin flap based on the bulbocavernosus muscle can be transposed to
aid in the closure. This myocutaneous tissue, which in most patients
with gynecologic malignancy is usually spared from heavy radiation,
brings a nonirradiated blood supply to aid in wound healing.
Physiologic Changes. The vesicovaginal fistula is
closed. The vulva is spared excoriation from constant urine leakage.
Points of Caution. The
surgeon must ensure that the blood supply of the bulbocavernosus
muscle is intact. If the patient has received radiation that has
covered the vulva, the blood supply muscle and fat pad may be insufficient
for proper nutrition to the island skin flap. In addition, the margins
of the vesicovaginal fistula must be examined and found free of necrosis
and cellulitis before a closure is attempted.
Technique
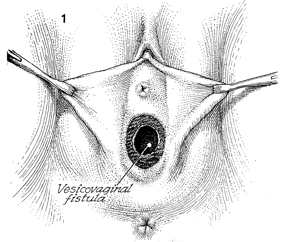
A vesicovaginal fistula is depicted
slightly behind the trigone of the bladder. The surgeon has debrided
the vesicovaginal fistula of all scarring and unhealthy tissue.
Previous cystoscopy has shown that the ureteral orifices and
ureters at the trigone are intact and not involved with the fistulae.
If this is in doubt, however, catheters should be placed up the
ureter to the kidney and left in for the entire operation. |
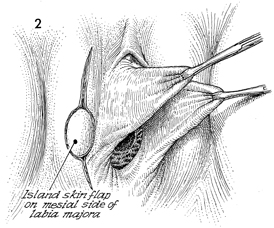
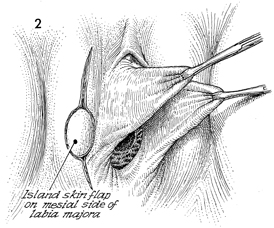
A longitudinal incision is made
from the top of the labia majora down to the point of the island
myocutaneous flap. After measuring the diameter of the vesicovaginal
fistula in the vagina, this island skin flap can be marked off
and cut to appropriate size. It is always wise to cut the island
skin flap a little larger than needed. |
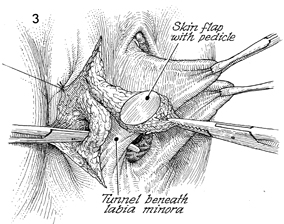
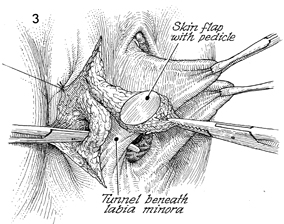
The island skin flap has been dissected
out with its bulbocavernosus muscle and associated fat pad that
ensures the blood supply to the skin flap through its small perforated
vessels. A Kelly clamp is used to open a tunnel underneath the
labia minora. The labia minora are retracted away from this area
with Allis clamps. |
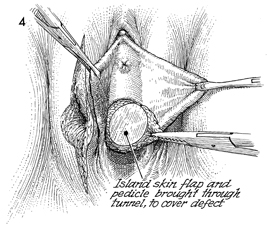
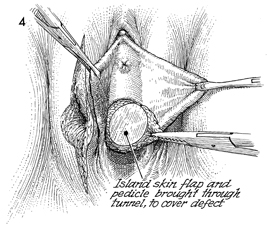
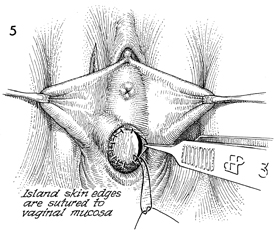
The bulbocavernosus myocutaneous
flap has been tunneled underneath the labia minora. It is placed
into the defect of the vesicovaginal fistula. |
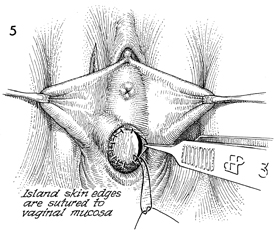
The bulbocavernosus myocutaneous
flap is sutured to the margins of the vaginal mucosa with interrupted
3-0 monofilament delayed synthetic absorbable suture. The bladder
can be tested at this point by placing a catheter in the bladder
and filling the bladder with a milk solution to note any leaks
around the fistula. A cystoscope can be placed to ensure that
the ureteral orifices are intact and not compromised by the surgical
procedure or the sutures used to place the flap.
|
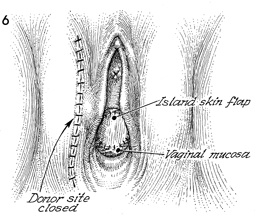
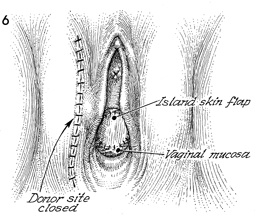
The vesicovaginal fistula repair has
been completed. The donor site incision is closed with interrupted
monofilament synthetic absorbable suture.
|
|