Reconstruction
of the Urethra
Reconstruction of the urethra is indicated if a part
of the urethra has been surgically removed or if there is a failure
of fetal urogenital sinus development. Loss of a portion of the urethra
may not be associated with total incontinence of urine. In cases of
epispadias, however, there is total incontinence. In those patients
who have lost the distal portion of the urethra and remain continent,
considerable disability remains because the voided stream may by uncontrollable
and, therefore, result in a significant esthetic problem.
When reconstruction
of the urethra is required because of total epispadias, the patient
may get a satisfactory anatomic result but remain incontinent unless
the procedure is combined with a Goebell-Stoeckel fascia lata strap
operation (see Vagina and Urethra).
Physiologic Changes. An epithelial channel is constructed
from the base of the bladder to the urethral meatus. Although this
neourethra has no muscle, it acts as a conduit for the proximal urethra
or bladder.
Points of Caution. The vaginal flap
must be designed to ensure that the vascular supply to the base of
the flap is sufficient to support the length of the flap needed.
If
the tube flap technique (Figs. 7-11) is employed, adequate flaps of
epithelium must be mobilized to meet in the midline without tension.
In
both techniques, mobilization of the lateral labial epithelium is essential
to cover and support the neourethra without tension.
Technique
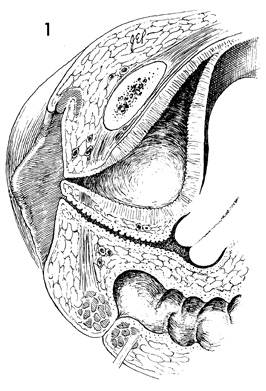
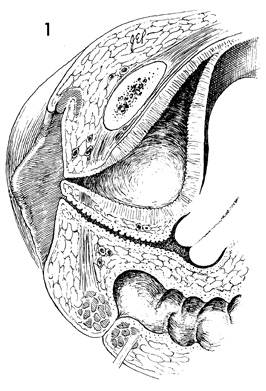
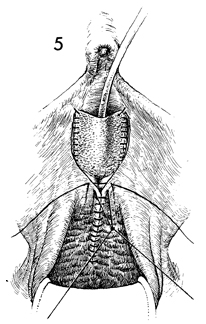
A sagittal section of the pelvis
without a urethra is shown. The patient is placed in the dorsal
lithotomy position. The perineum is surgically prepared. Careful
measurements should be made to design an adequate flap with 2
cm of width at the base for every 1 cm of length to ensure an
adequate blood supply to the flap. |
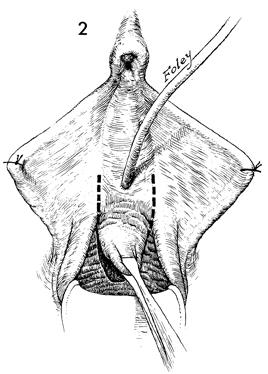
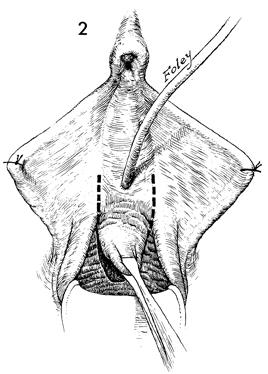
The proposed flap should be marked
off on the anterior vaginal wall. The mucosa is incised down
to the pubovesical cervical fascia with a scalpel. A Foley catheter
is inserted as indicated. |
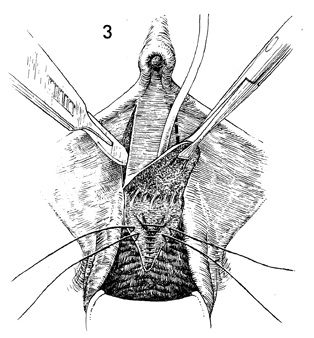
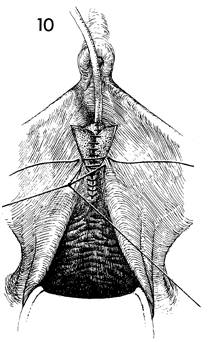
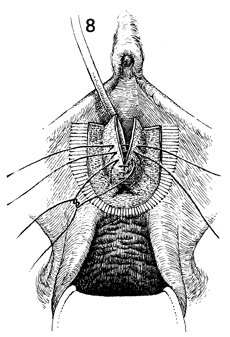
The flap has been mobilized. Two
parallel incisions are made approximately 2 cm apart to prepare
the receptor bed for the edges of the flap. Plication sutures
are placed in the pubovesical fascia from the apex of the vaginal
incision to the neourethral vesical angle. |
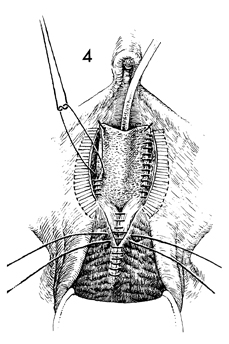
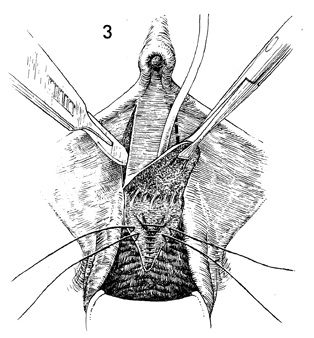
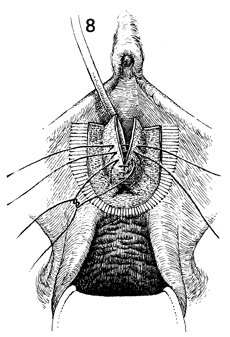
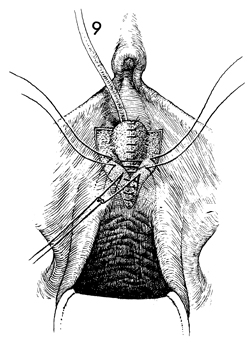
The flap is sutured into position
along the lateral grooves incised in the vestibule. This is performed
with interrupted 4-0 synthetic absorbable suture. Lateral to
the grooves, the labial tissue is mobilized by undermining it
for a sufficient distance, usually 4 cm, to allow it to be brought
to the midline without tension.
The vaginal wall defect should
be closed with interrupted 2-0 synthetic absorbable sutures. |
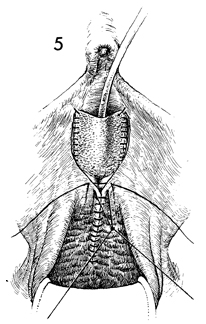
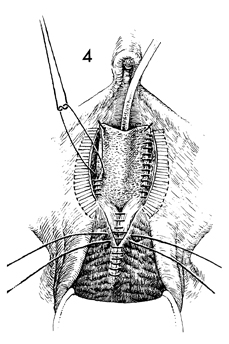
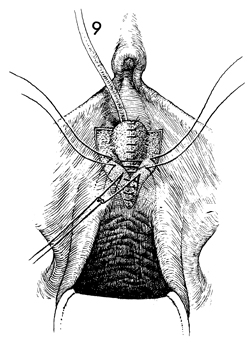
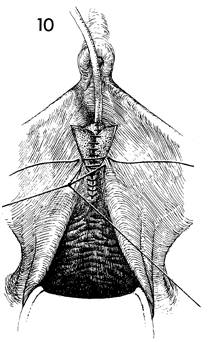
The previously mobilized labial
epithelium is sutured in the midline with 2-0 synthetic absorbable
sutures to cover the flap and provide nutrition and support. |

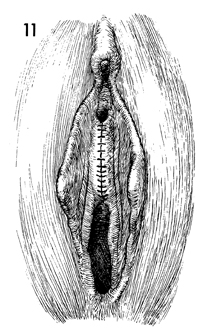
The completed operation is shown. |
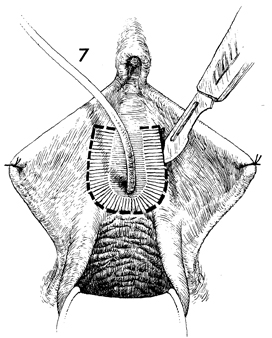
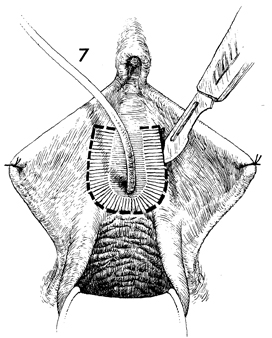
A second technique for reconstruction
of the urethra involves rolling a tube flap, then covering it
with a second layer of periurethral tissue. The flap is marked
with brilliant green solution along the proposed new urethra.
Care should be taken to ensure that sufficient tissue is mobilized
to allow it to meet in the midline without tension. The margins
of the flap are incised with a scalpel, and the tissue is mobilized
medially. |
Tissue is then rolled toward the midline
and sutured into place with interrupted 4-0 synthetic absorbable
suture. The tissue lateral to the mobilized flap is undermined
for a distance of about 4 cm. |
The lateral tissue is closed over the flap
in two layers with interrupted 3-0 synthetic absorbable suture.
A Foley catheter remains in the bladder. |
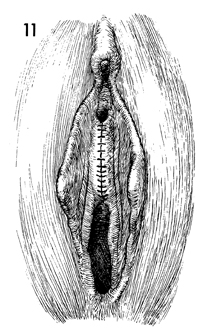
The epithelium is closed with interrupted
3-0 absorbable sutures. |
The completed operation is shown with neourethra. |
|
|