Vagina
and Urethra
Anterior Repair and Kelly
Plication
Site Specific Posterior Repair
Sacrospinous
Ligament Suspension of the Vagina
Vaginal Repair of Enterocele
Vaginal Evisceration
Excision of
Transverse Vaginal Septum
Correction of
Double-Barreled Vagina
Incision
and Drainage of Pelvic Abscess via the Vaginal Route
Sacral Colpoplexy
Le Fort Operation
Vesicovaginal Fistula
Repair
Transposition
of Island Skin Flap for Repair of Vesicovaginal Fistula
McIndoe Vaginoplasty
for Neovagina
Rectovaginal Fistula
Repair
Reconstruction of
the Urethra
Marsupialization
of a Suburethral Diverticulum by the Spence Operation
Suburethral
Diverticulum via the Double-Breasted Closure Technique
Urethrovaginal
Fistula Repair via the Double-Breasted Closure Technique
Goebell-Stoeckel
Fascia Lata Sling Operation for Urinary Incontinence
Transection
of Goebell-Stoeckel Fascia Strap
Rectovaginal
Fistula Repair via Musset-Poitout-Noble Perineotomy
Sigmoid
Neovagina
Watkins Interposition Operation |
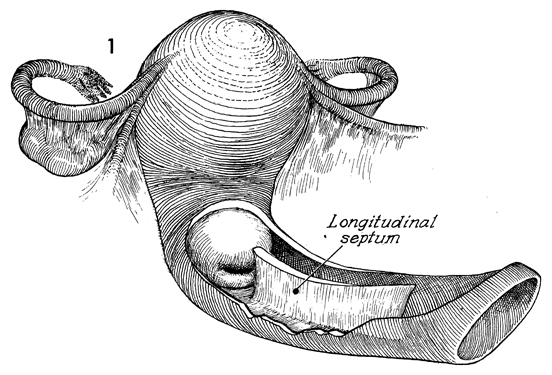
Correction of Double-Barreled Vagina
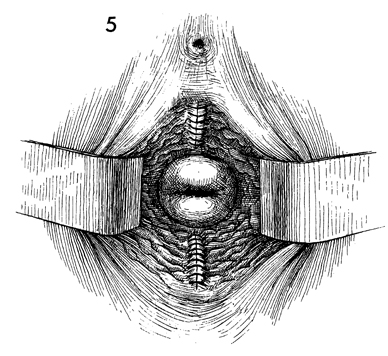
The Mullerian ducts are said to account for the upper
one-third of the vagina. Their failure to fuse can leave the vaginal
canal with a longitudinal horizontal septum that may extend from the
upper vagina as far as the vaginal outlet. This condition, known as
a "double-barreled vagina," is frequently unnoticed by the patient
until an initial gynecologic examination or delivery of the first baby.
It requires the surgeon to perform an appropriate workup for failure
of the other structures derived from the Mullerian ducts, such as the
cervix and the uterus. In addition, some patients with Mullerian duct
abnormalities have concomitant urinary tract abnormalities and, therefore,
an intravenous pyelogram (IVP) may be indicated. The best procedure
for correcting the longitudinal septum is excision.
The purpose of
the operation is to create a single-barreled vagina and, at the same
time, avoid dyspareunia.
Physiological Changes. A normal vagina is created.
Points of Caution. In creating a single-barreled vagina,
the surgeon must be careful not to remove excessive vaginal mucosa.
Technique
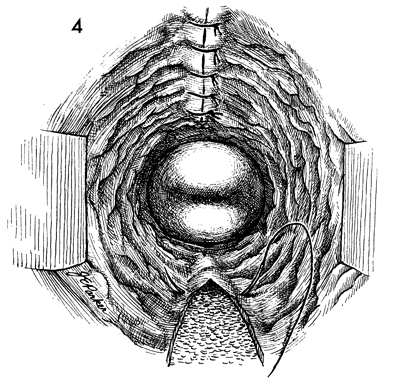
The longitudinal septum is demonstrated in this
cutaway section. |
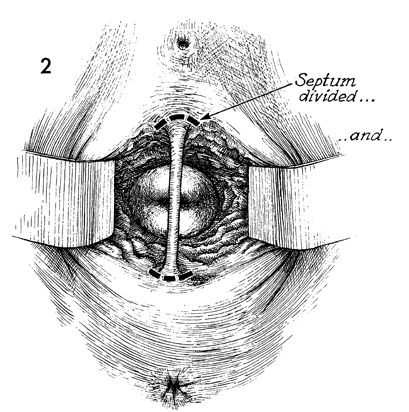
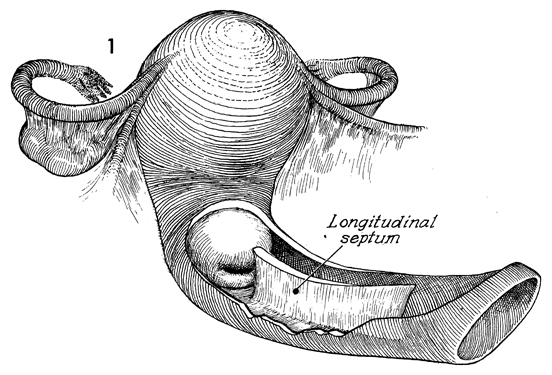
With the patient in the dorsal lithotomy position, the vulva and
vagina are prepped, the patient is draped, and the bladder is emptied
by catheterization. Adequate exposure to each vaginal canal is
made by lateral retractors. The longitudinal septum is grasped
with a clamp or tissue forceps and slight traction is applied.
Extreme traction should be avoided in order not to tent the underlying
urethra and bladder tissue into the area to be excised. The junction
of the longitudinal septum and vaginal mucosa should be excised
with scissors. The same procedure is carried out at the junction
of the longitudinal septum on the posterior vaginal wall. A defect
is made in the anterior and posterior vaginal walls that should
extend no deeper than the pubovesical cervical fascia anteriorly
and the perirectal fascia posteriorly. |
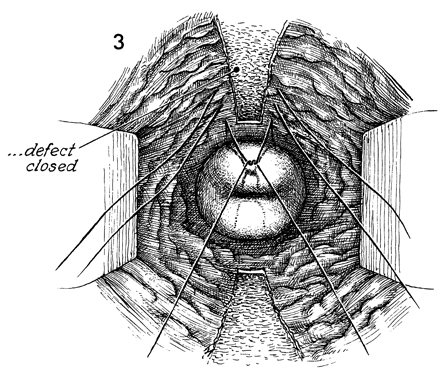
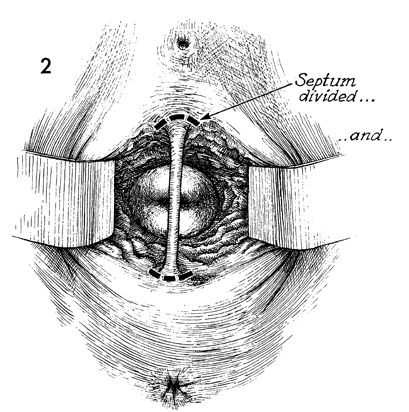
Primary repair can be carried out by closing the defect with interrupted
2-0 synthetic absorbable suture. |
The same technique is used to repair the
posterior vaginal wall. |
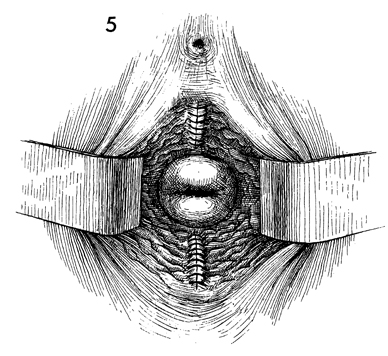
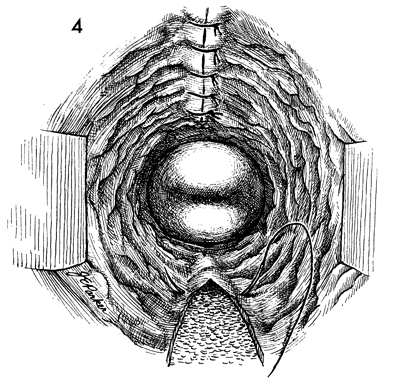
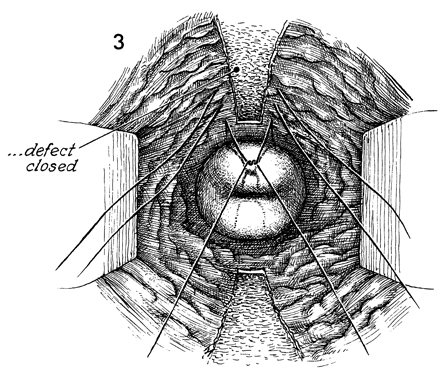
The repair is completed. No vaginal pack is left in the vagina,
and no catheter is needed for drainage of the bladder. The patient
can usually be discharged within 1-2 days after the operation and
can resume sexual intercourse 1 month after closure of the vaginal
incision. |
|