Vagina
and Urethra
Anterior Repair and Kelly
Plication
Site Specific Posterior Repair
Sacrospinous
Ligament Suspension of the Vagina
Vaginal Repair of Enterocele
Vaginal Evisceration
Excision of
Transverse Vaginal Septum
Correction of
Double-Barreled Vagina
Incision
and Drainage of Pelvic Abscess via the Vaginal Route
Sacral Colpoplexy
Le Fort Operation
Vesicovaginal Fistula
Repair
Transposition
of Island Skin Flap for Repair of Vesicovaginal Fistula
McIndoe Vaginoplasty
for Neovagina
Rectovaginal Fistula
Repair
Reconstruction of
the Urethra
Marsupialization
of a Suburethral Diverticulum by the Spence Operation
Suburethral
Diverticulum via the Double-Breasted Closure Technique
Urethrovaginal
Fistula Repair via the Double-Breasted Closure Technique
Goebell-Stoeckel
Fascia Lata Sling Operation for Urinary Incontinence
Transection
of Goebell-Stoeckel Fascia Strap
Rectovaginal
Fistula Repair via Musset-Poitout-Noble Perineotomy
Sigmoid
Neovagina
Watkins Interposition Operation |
Rectovaginal Fistula Repair
Rectovaginal fistulae must be divided into two groups.
The first group consists of those that occur secondary to obstetric
or gynecologic surgery for benign disease. The second group consists
of those that are associated with radiation therapy for pelvic malignancy.
Rarely is a diverting colostomy needed for fistulae from benign disease.
A transverse colostomy is always needed, however, for pelvic cancer
patients who have rectovaginal fistulae secondary to irradiation. An
outside blood supply, such as a muscular flap, is not required for
the repair of small rectovaginal fistulae secondary to obstetric or
gynecologic surgery, unless there is excessive scarring or repeated
attempts at closure have been unsuccessful. Patients with rectovaginal
fistulae associated with pelvic irradiation, however, require a vascular
flap to improve blood supply to the irradiated tissues.
The bulbocavernosus
muscle is the most convenient source of blood supply, but other sources
include the omentum, gracilis muscle, and myocutaneous flaps.
The cardinal
principles of repair of rectovaginal fistulae are (1) delay of repair
until all inflammation has cleared at the fistulae site, even if a
preoperative perineotomy is required; (2) excision of all fibrotic
and scar tissue surrounding the fistulous tract; (3) complete mobility
of the rectum and colon to eliminate any tension on the rectal mucosa
after excision of the scarred tissue; (4) use of delicate surgical
technique to preserve as much vascularity as possible; (5) broad surface-to-surface
closure; (6) improved vascularity using an outside blood supply; and
(7) diverting colostomy, in cases of irradiation, until 3-4 months
after the fistula has been confirmed closed by repeated examination.
Physiologic Changes. The rectovaginal
fistula is closed, and normal defecation per anus is resumed.
The bulbocavernosus
flap used to cover the rectovaginal fistula suture line improves vascularity
and gives an additional layer to the closure, thus improving the chances
of permanent fistula repair.
Points of Caution. The margins of
the rectal mucosa must lie adjacent to each other without tension.
Tension on the rectal mucosa suture line will invariable result in
separation of the wound. Hemostasis is a vital factor. The hemorrhoidal
plexus of veins can be difficult to control, but meticulous technique
in clamping, tying, and/or electrocoagulating each of these vessels
is imperative to fistula closure.
Dilatation of the anus at operation
produces temporary rectal paralysis of the sphincter muscle and, thereby,
temporary rectal incontinence, preventing the buildup of flatus and
stool in the terminal rectum and avoiding tension on the suture line.
Technique
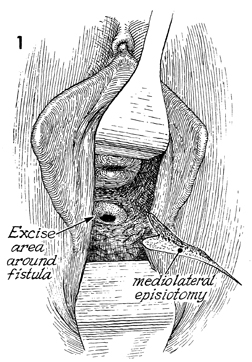
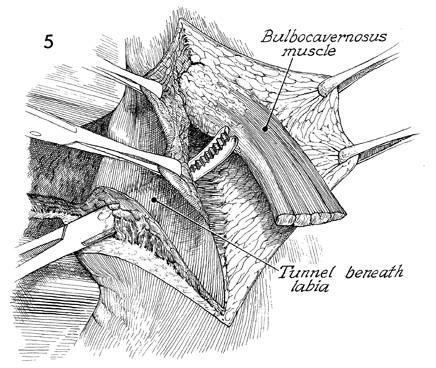
Occasionally, a fistula high inside
a narrow vagina is difficult to expose. Therefore, a mediolateral
episiotomy should be performed without hesitation to allow maximum
exposure to the operating site. The mediolateral episiotomy should
be extended up the vaginal mucosa to the margin of the fistula.
If adequate exposure cannot be obtained completely from the vaginal
approach, the abdominal route should be considered, particularly
in those cases where the fistula is high in a deep vagina. |
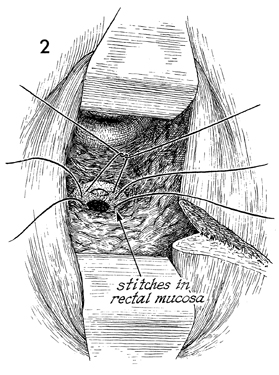
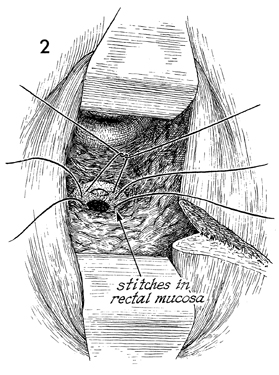
Extreme care should be taken that
the bowel mucosa is adequately mobilized and that devitalized,
scarred, or avascular portions of the mucosa have been excised.
If the intestinal mucosa cannot be mobilized and it is apparent
that the closure of the intestinal mucosa will be under tension,
the surgeon should perform a laparotomy and totally mobilize
the rectosigmoid colon from above. Many fistula repairs fail
because this in not done. After adequate mobilization of the
intestinal mucosa, the edges of the intestinal mucosa are closed
in an inverting fashion with interrupted 3-0 Dexon suture with
a Lembert stitch. |
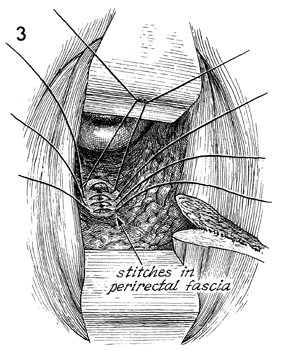
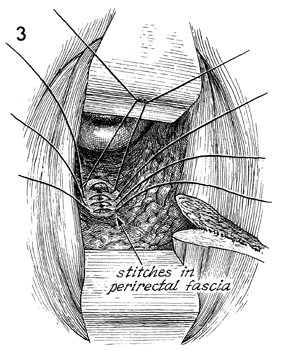
The perirectal fascia and even some
levator ani muscle may be drawn into a second layer of closure
using 0 Dexon. |
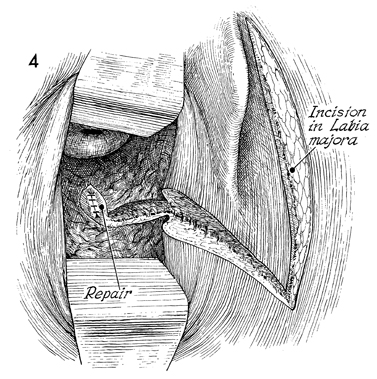
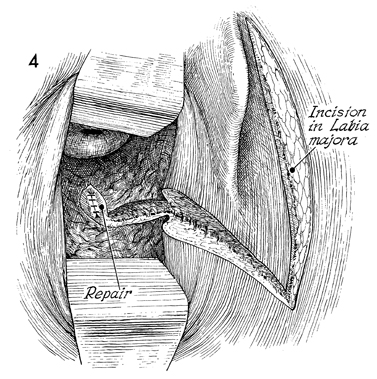
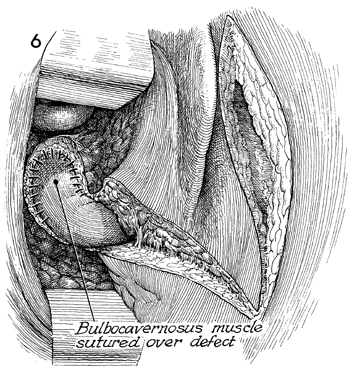
If an outside blood supply is desirable,
the margin of the excised fistula tract is connected with the
incision of the episiotomy. The bulbocavernosus muscle is palpated
under the labia majora, and a longitudinal incision is made down
the labia majora through the fat pad until the bulbocavernosus
muscle is located. |
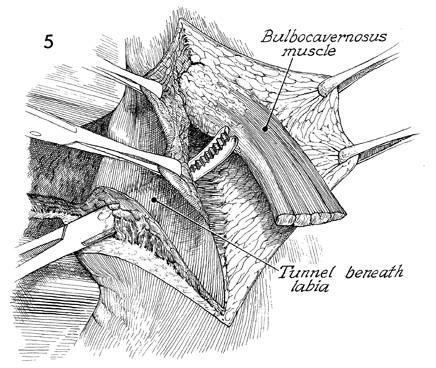
The bulbocavernosus muscle is dissected
out and transected above its insertion into the perineal body,
leaving its blood supply from the branches of the pudendal artery
intact. A tunnel approximately 3 cm wide is created from inside
the vaginal canal with a Kelly clamp, and the bulbocavernosus
muscle is drawn through this tunnel underneath the labia minora
and hymenal ring. |
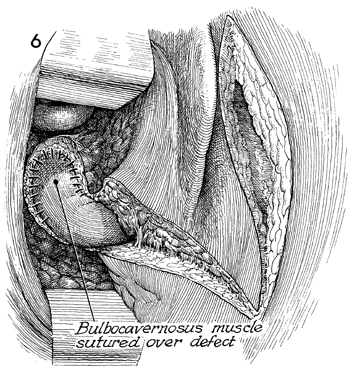
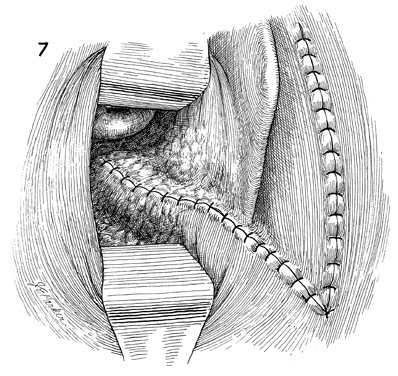
The bulbocavernosus muscle is sutured
over the perirectal fascia with interrupted 3-0 Dexon sutures. |
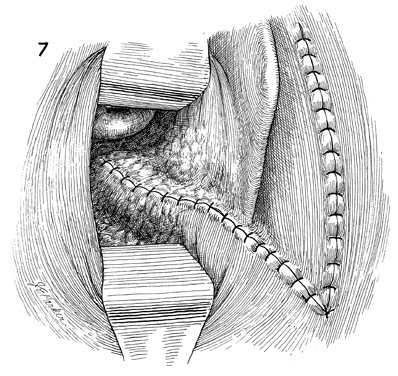
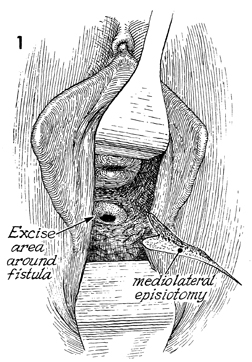
The edges of the vaginal mucosa
are then approximated with interrupted 2-0 Dexon sutures. The
wound over the labia minora may be sutured by subcuticular 3-0
Dexon or interrupted 4-0 nylon sutures. Occasionally, there will
be troublesome bleeding from the bed of the bulbocavernosus muscle.
If this cannot be brought under adequate control by delicate
clamping and suturing, it is often possible to pack this area
with Avitene collagen hemostat. In this event, a small 1/4-inch
closed suction drain can be brought out from the inferior edge
of the labial incision. To have the entire wound completely dry
and avoid hemostatic agents or drains is preferred, however.
Care must be taken to ensure
that the stool is completely soft and that there is no buildup
of flatus above the sphincter. The latter can be accomplished
by two techniques. One is to dilate the sphincter to 4-5 cm manually,
thus temporarily paralyzing the rectal sphincter and leaving
the patient fecally incontinent for approximately 1 week. The
other is to incise the rectal sphincter at the 7 or 9 o'clock
position in one plane only. Multiple radial incisions in the
rectal sphincter may produce permanent fecal incontinence. It
is highly recommended that the patient use a stool softener for
3-6 months following fistula repair.
|
|
|