|
||||||||||
Anterior Repair and Kelly
Plication |
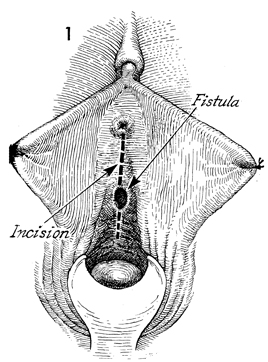
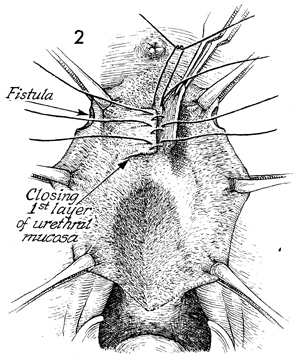
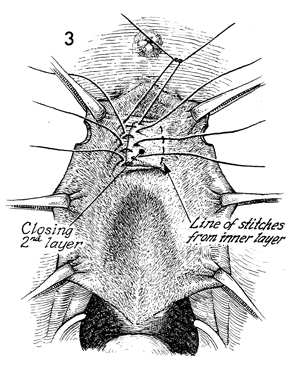
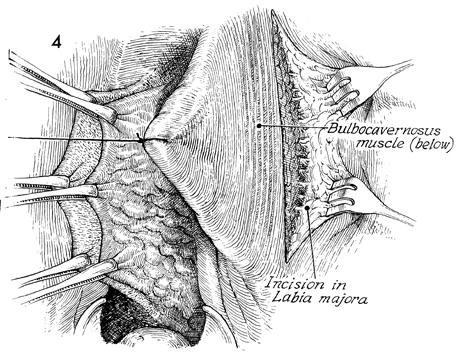
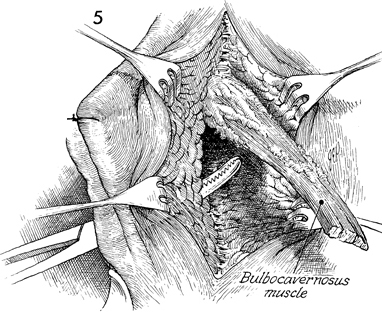
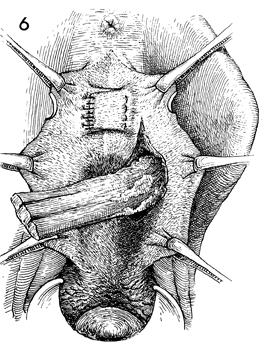
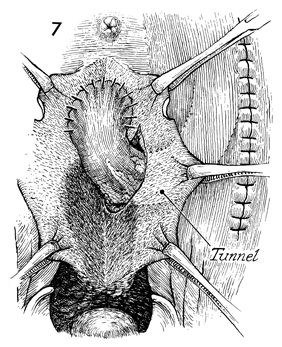
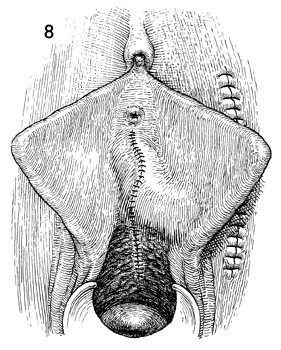
Urethrovaginal Fistula Repair via the Double-Breasted Closure Technique Urethrovaginal fistulae are generally secondary to one of two conditions: (1) surgical trauma following anterior colporrhaphy or (2) obstetrical trauma. In many instances, a urethrovaginal fistula exists, but the patient is still completely continent and has no problem voiding. Some patients with this condition, especially those with the fistula in the proximal one-third of the urethra, suffer a combination of incontinence and inability to control their urine stream when attempting to void. This technique is not applicable to fistulae in the distal one-third of the urethra. Those fistulae are adequately treated by the Spence operation. Physiologic Changes. In repairing a urethrovaginal fistula, the surgeon corrects the physiology of the urethra so that the patient may remain continent and the urinary stream may be emitted normally from the meatus. This procedure consists of three basic principles: (1) excise the scarred, devascularized tissue surrounding the fistula, (2) approximate healthy margins of tissue with multiple layers of closure, and (3) bring a source of blood supply and support to the base of the urethra to cover the fistula. This is particularly important in those cases where severe scarring and devasularization of tissue have occurred. Preoperative evaluation of the patient should consist of a complete bladder-urethra workup including urodynamics, cystoscopy, urethroscopy, and urine culture. Points of Caution. The margins of the fistula must be brought together without tension. The flaps of the pubovesical cervical fascia must be mobilized to allow the double-breasted closure technique. The size and caliber of the urethra must be adequate for voiding. The multiple-layer approach to fistula closure has stood the test of time and represents the best opportunity for permanent closure. A vascular pedicle flap such as the bulbocavernosus muscle has reduced the incidence of recurrent fistula in high-risk patients. Technique
|
|||||||||
Copyright - all rights reserved / Clifford R. Wheeless,
Jr., M.D. and Marcella L. Roenneburg, M.D.
All contents of this web site are copywrite protected.