Vagina
and Urethra
Anterior Repair and Kelly
Plication
Site Specific Posterior Repair
Sacrospinous
Ligament Suspension of the Vagina
Vaginal Repair of Enterocele
Vaginal Evisceration
Excision of
Transverse Vaginal Septum
Correction of
Double-Barreled Vagina
Incision
and Drainage of Pelvic Abscess via the Vaginal Route
Sacral Colpoplexy
Le Fort Operation
Vesicovaginal Fistula
Repair
Transposition
of Island Skin Flap for Repair of Vesicovaginal Fistula
McIndoe Vaginoplasty
for Neovagina
Rectovaginal Fistula
Repair
Reconstruction of
the Urethra
Marsupialization
of a Suburethral Diverticulum by the Spence Operation
Suburethral
Diverticulum via the Double-Breasted Closure Technique
Urethrovaginal
Fistula Repair via the Double-Breasted Closure Technique
Goebell-Stoeckel
Fascia Lata Sling Operation for Urinary Incontinence
Transection
of Goebell-Stoeckel Fascia Strap
Rectovaginal
Fistula Repair via Musset-Poitout-Noble Perineotomy
Sigmoid
Neovagina
Watkins Interposition Operation |
Incision and Drainage of Pelvic Abscess via
the Vaginal Route
A pelvic abscess can be drained through the vagina if three conditions
are present. The abscess must (1) be fluctuant, (2) dissect the rectovaginal
septum, and (3) be in the midline. If any of these three criteria is
absent, complications are increased significantly. If the abscess is
not fluctuant, adequate drainage cannot be achieved. If the abscess
has not dissected the rectovaginal septum, the vaginal incision may
enter the rectum. If the abscess is not in the midline, incision and
drainage will result in peritoneal spread of purulent material.
The purpose of the operation is to drain the abscess and thereby allow
reversal of the septic process.
Physiologic Changes. The
physiologic changes associated with incision and drainage of any
abscess are release of the purulent material to the outside and relief
of the septic condition associated with the abscess.
Points of Caution. In addition to the above-mentioned
criteria essential for drainage, the abscess must remain open 4-6 days
to allow complete drainage and granulation of the abscess cavity.
Technique
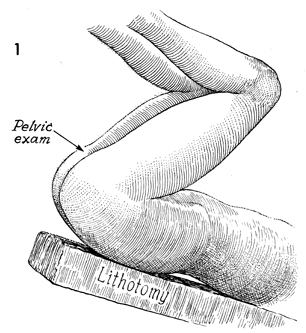
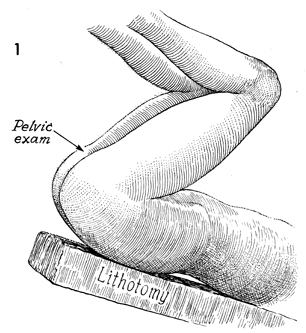
The patient is placed in the dorsal
lithotomy position and is prepped and draped.
|
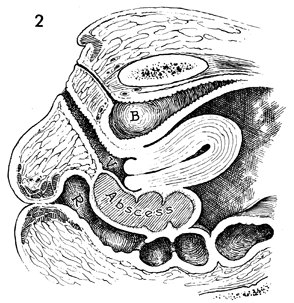
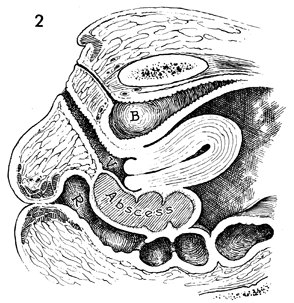
A sagittal view illustrates one
of the three criteria necessary for drainage, i.e., dissection
of the rectovaginal septum by the abscess. B,
bladder; R, rectum; and V,
vagina. |
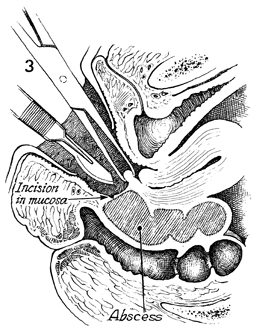
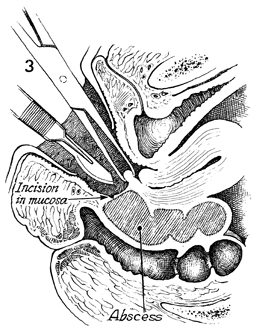
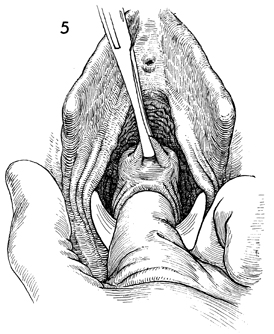
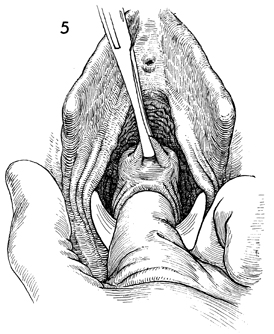
The posterior lip of the cervix
is grasped with a Jacobs tenaculum, and traction is applied.
A scalpel is used to incise the vaginal mucosa. |
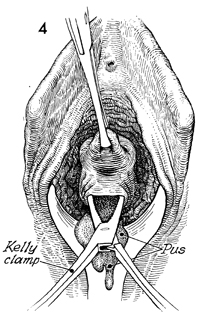
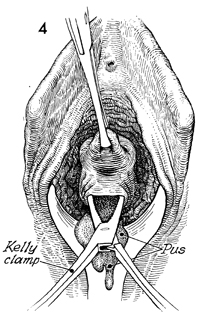
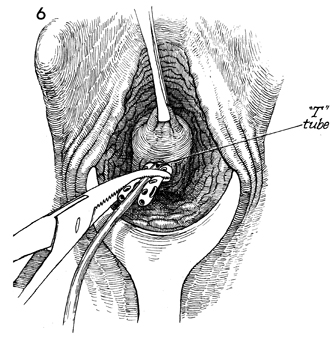
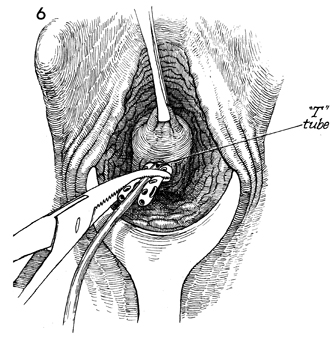
With the posterior lip of the cervix
under traction, a Kelly clamp is used to puncture the abscess,
allowing the egress of pus. |
A finger is inserted into the abscess
cavity to break up adhesions and drain any additional small loculated
abscesses. |
|
 |
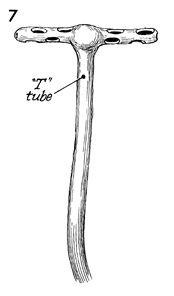 |
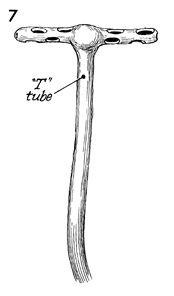
A
convenient drain for pelvic abscess is a T-tube. We prefer a
16-French size, with the arm of the T cut off approximately 3
cm from the shaft of the tube. In addition, small holes are made
along the arms of the T. The arms of the T are then folded back
on the shaft of the tube, which is grasped with a Kelly clamp
and inserted up into the pelvic abscess. When the Kelly clamp
is removed, the arms of the T return to their original position,
thereby holding the drain in place. |
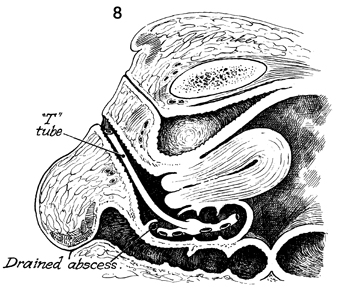
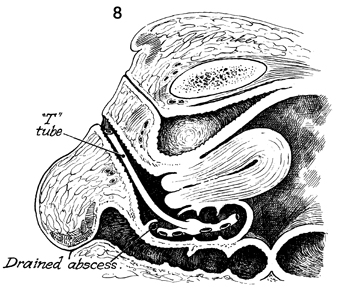
A sagittal section shows the drain in place
in the pelvic abscess. Suction on the T-tube is not necessary
and may inadvertently result in its removal. The shaft of the
T-tube should be trimmed behind the introitus so that it does
not protrude through the labia minora and hymenal ring. |
|
|