Malignant
Disease:
Special Procedures
Staging
of Gynecologic
Oncology Patients With
Exploratory Laparotomy
Subclavian Port-A-Cath
Peritoneal Port-A-Cath
Application
of Vaginal
Cylinders for Intracavitary
Radiation Therapy
Application
of Uterine Afterloading Applicators
for Intracavitary Radiation Therapy
Pelvic High-Dose
Afterloader
Abdominal
Injection of Chromic Phosphate
( ) )
Supracolic
Total Omentectomy
Omental Pedicle "J"
Flap
Tube Gastrostomy
Total Vaginectomy
Radical
Vulvectomy
With Bilateral Inguinal
Lymph Node Dissection
Reconstruction
of the
Vulva With Gracilis Myocutaneous Flaps
Transverse
Rectus
Abdominis Myocutaneous
Flap and Vertical Rectus
Abdominis Myocutaneous
Flap
Radical
Wertheim
Hysterectomy With
Bilateral Pelvic Lymph
Node Dissection and With Extension of the Vagina
Anterior Exenteration
Posterior Exenteration
Total Pelvic
Exenteration
Colonic
"J" Pouch Rectal
Reservoir
Kock Pouch
Continent Urostomy
Omental "J" Flap
Neovagina
Ileocolic
Continent Urostomy (Miami Pouch)
Construction
of Neoanus
Gracilis Dynamic Anal
Myoplasty
Skin-Stretching
System Versus Skin Grafting
Gastric
Pelvic Flap for
Augmentation of Continent Urostomy or Neovagina
Control
of Hemorrhage in Gynecologic Surgery
Repair
of the Punctured
Vena Cava
Ligation
of a Lacerated
Internal Iliac Vein and
Suturing of a Lacerated Common Iliac Artery
Hemorrhage
Control in
Sacrospinous Ligament
Suspension of the Vagina
Presacral
Space
Hemorrhage Control
What
Not to Do in Case of Pelvic Hemorrhage
Packing
for Hemorrhage
Control
Control
of Hemorrhage
Associated With Abdominal Pregnancy |
Radical Vulvectomy With Bilateral
Inguinal Lymph Node Dissection
Radical vulvectomy with bilateral inguinal lymph node dissection is
indicated in invasive carcinoma of the vulva. The operation is best
performed in a single-stage procedure. Emphasis is placed on removal
of the entire lesion with an adequate tumor-free margin.
The purpose
of this operation is to remove the vulva, its adjacent structures,
a margin of normal tissue, and the inguinal lymph nodes from the anterior
superior iliac spine to the abductor canal in the leg.
Physiologic Changes. A large surgical wound is created
by this operation. If it cannot be closed per primam without tension,
it must be sealed with grafting or use of the new Sure-Closure skin
stretcher. If it is allowed to granulate slowly, marked physiologic
changes similar to those accompanying a burning, i.e., the loss of
electrolytes, fluids, and protein and contracture, will occur from
contracture.
Trauma to the femoral artery and vein increases the risk of thrombophlebitis
and pulmonary embolism.
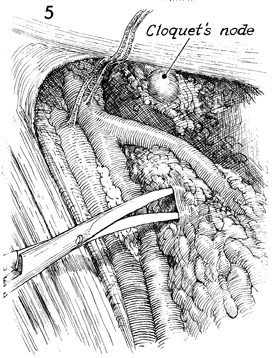
Points of Caution. Care must be taken that all lymph
nodes are excised. The Cloquet node should be removed and sent for
frozen section analysis. Pathologic analysis of this node determines
if a deep pelvic lymph node dissection is indicated.
The surgeon must clearly identify the saphenous vein to avoid its accidental
transection.
Before proceeding with dissection below the mons pubis,
the surgeon must make an incision around the urethral meatus and vaginal
introitus.
Mature surgical judgment is needed to ascertain
whether the margins of the wound can be sufficiently undermined and
mobilized to be brought together without tension. Radical vulvectomy
incisions closed under tension will necrose and open in approximately
1 week. The Sure-Closure skin stretchers are an alternative to undermining
skin flaps. Closed suction drainage of the wound has reduced seroma
formation and its associated sequelae.
Technique
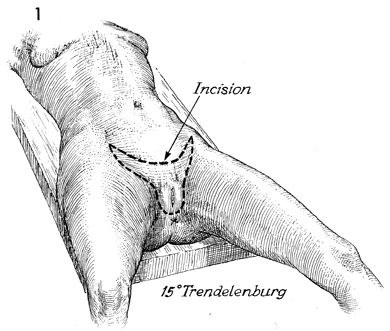
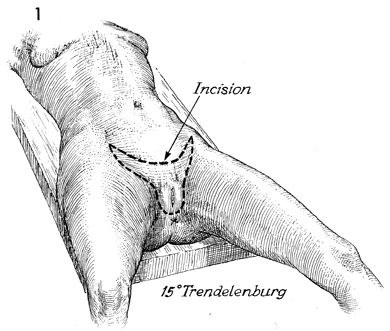
The patient undergoing radical vulvectomy
should be positioned on the operating table in the modified dorsal
lithotomy position with the legs extended, giving adequate exposure
to the lower abdomen and perineum. The hips should be abducted
30° and extended 5-10° with the knees flexed 90°.
The abdomen and perineum are
surgically prepped. A Foley catheter is inserted in the bladder.
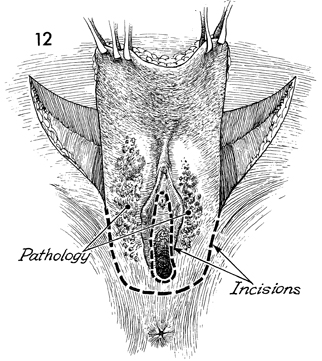
Although a variety of incisions
can be used for this operation, one shaped roughly like the head
of a rabbit is preferred. The proposed incision is marked with
brilliant green solution, starting from the anterior superior
iliac spine, sloping downward toward the mons pubis, lateral
to the inguinal ligament, to a point adjacent to the pubic tubercle.
At this point, it proceeds lateral to the labia majora and horizontal
with a "W" incision across the perineal body, joining the incision
lateral to the labia majora on the opposite side. A second incision,
superior and medial to the first, slopes down toward the mons
pubis and meets a similar incision from the outside.
This procedure
is best carried out with two surgeons, each with an assistant,
operating on both sides. |
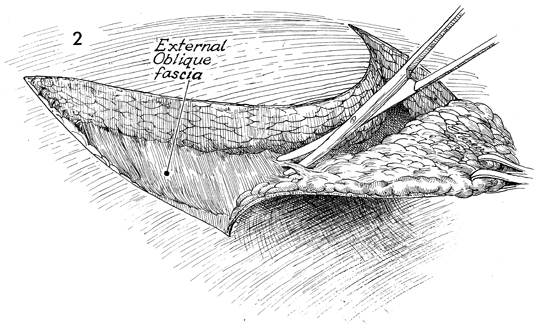
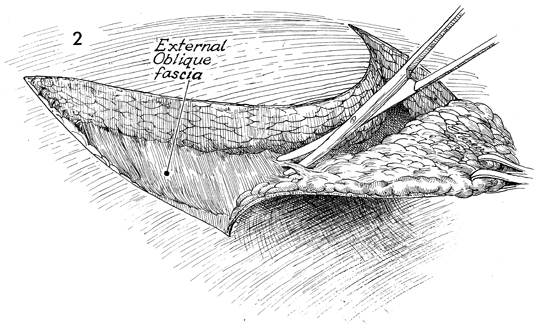
The upper portion of the entire
incision is made at one time. The incision is carried from the
anterior superior iliac spine down across the mons pubis, up
to the opposite anterior superior iliac spine, down lateral to
the inguinal ligament to the pubic tubercle. The incision is
carried through the skin down to the fascia. Metzenbaum scissors
are used to dissect along the fascial surface, removing en bloc
the skin and its subcutaneous lymph nodes. |
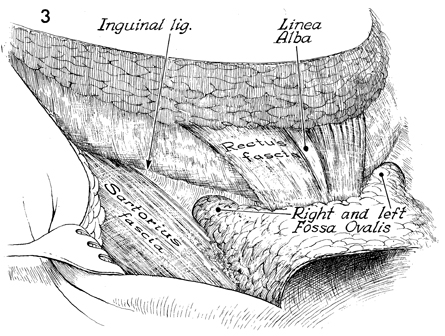
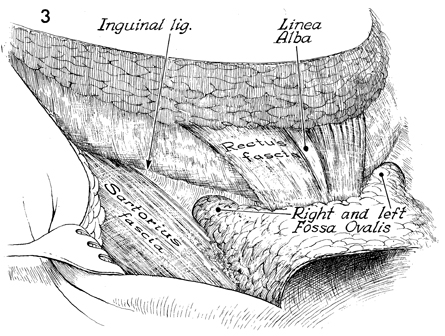
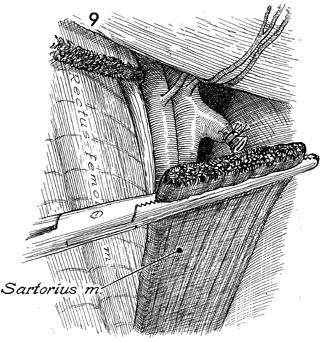
The inguinal ligament and rectus
fascia have been cleaned of all nodal tissue. A retractor is
used to deflect the skin overlying the sartorius muscle. The
right and left fossae ovalis are identified. If identification
of the fossae of ovalis proves difficult, the fascia covering
the sartorius muscle should be reflected medially to ensure total
removal of the lymph nodes without lacerating vascular structures
within the fossae ovalis. |
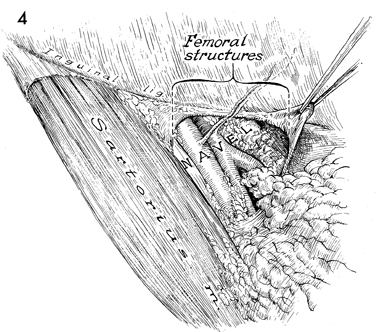
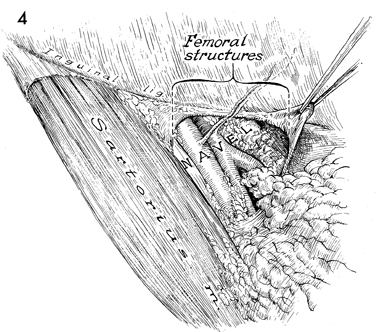
Structures within the femoral
canal generally follow the code word "navel", i.e., the most
lateral structure is the femoral nerve followed in order by the
femoral artery, vein, an empty space, and a lymphatic space.
The femoral artery should be identified, and dissection should
be carried along the artery until all lymphatic tissue is removed
down to the adductor canal. The femoral nerve should be preserved,
although occasionally a few of its terminal cutaneous branches
must be sacrificed. The femoral vein should be identified along
with the saphenous vein. This can be facilitated by noting the
anatomic relationship between the circumflex artery, generally
1-2 cm above the junction of the femoral artery, and the saphenous
veins. |
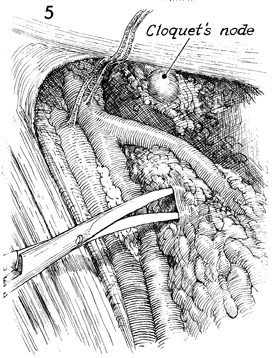
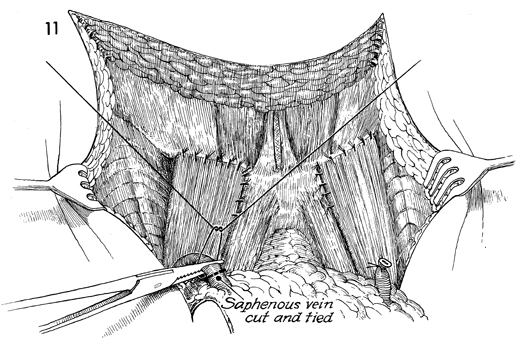
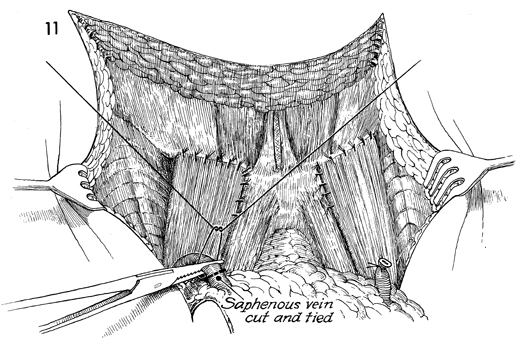
At this time, the Cloquet node is located,
removed, and sent for pathologic analysis. The lymphatic dissection
continues along the saphenous vein until it can be sufficiently
freed for clamping and ligation. |
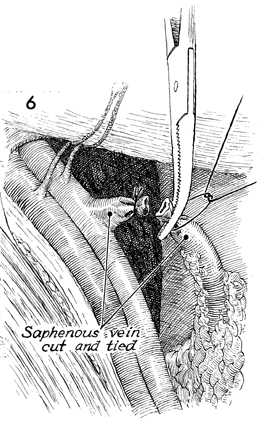
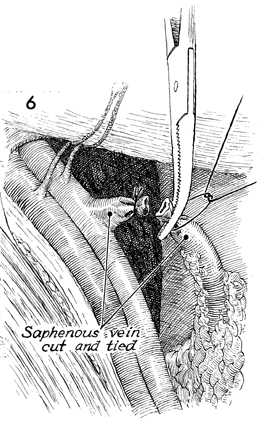
The saphenous vein is doubly clamped,
incised, and tied with a 2-0 suture. |
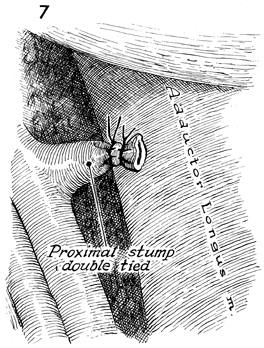
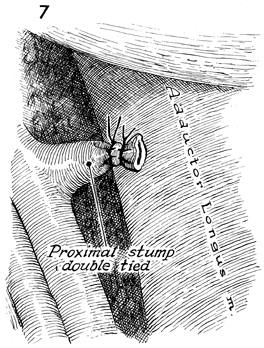
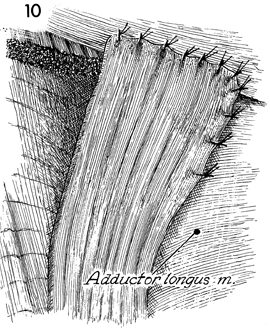
The adductor longus muscle can now be identified
and should be cleaned of all fatty nodal tissue by retracting
the saphenous vein en bloc with the lymph nodes until the adductor
canal is reached. |
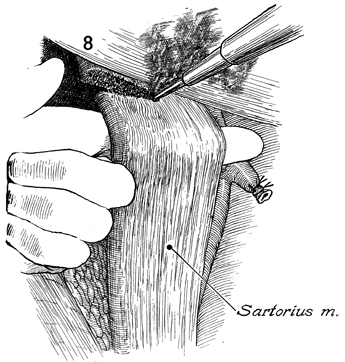
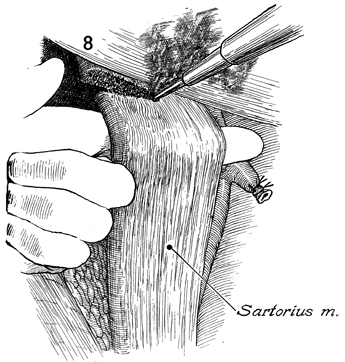
The sartorius muscle is identified,
mobilized and transected at its insertion with the electrocautery. |
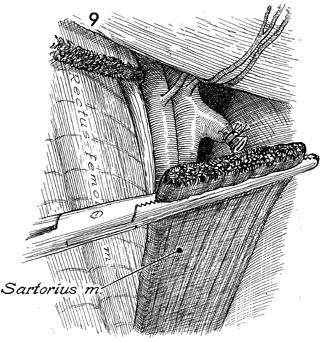
The sartorius muscle is transplanted over
the femoral artery and vein. |
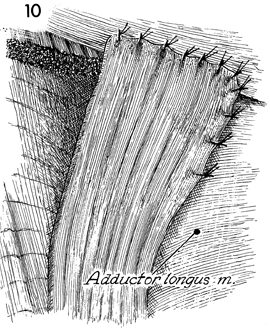
The sartorius muscle is sutured
to the inguinal ligament with interrupted 2-0 suture. To reduce
the possibility of hernia, a few 2-0 sutures are placed on the
medial border of the sartorius muscle, suturing it to the adductor
longus muscle. |
The lymph node dissection with
the sartorius transplant portion of the operation has now been
completed. The saphenous vein adjacent to the adductor canal
is identified for the second time. It is clamped and tied with
a 2-0 suture. |
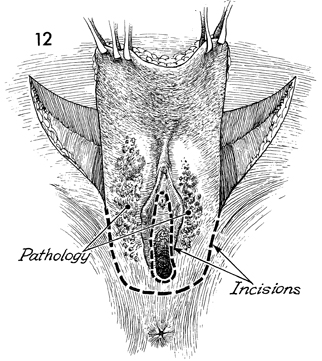
The surgeon moves from the lateral side of the patient
to the perineal area, and the entire surgical specimen is elevated
with Allis clamps.
A careful outline of the vaginal introital incision is made with
brilliant green solution. The incisions lateral to the labia majora
are made down to the fascia. |
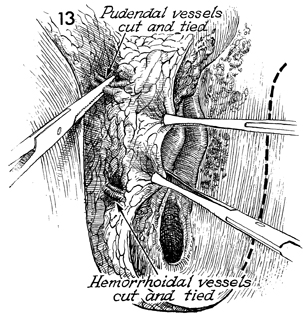
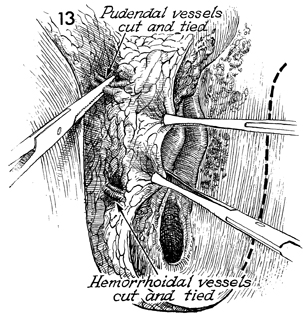
The pudendal artery and vein
are clamped and tied prior to transection. The specimen is retracted
medially with multiple Allis clamps. The incision is extended
down the lateral border of the labia majora and superficially
extended across the perineal body. |
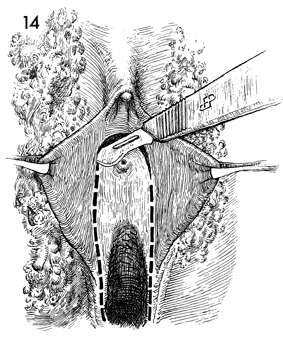
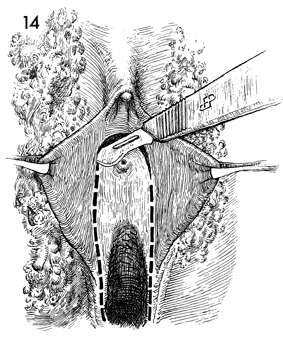
The labia minora are retracted
laterally with Allis clamps, and an incision is made in the vestibule
around the urethral meatus, down around the posterior fourchette,
and back up the other side. |
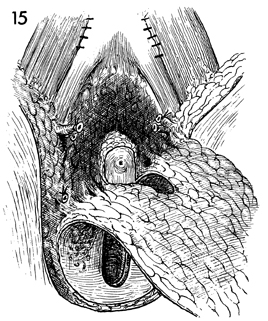
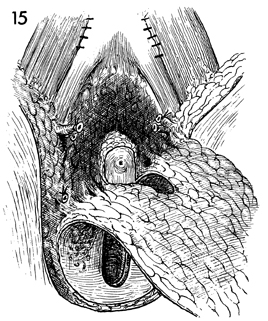
The en bloc specimen is retracted downward, and the
surgical dissection is made along the fascia until the perineal
body is reached.
|
The surgeon elevates the posterior
vaginal mucosa with Allis clamps and undermines it for approximately
6-7 cm with curved Mayo scissors, releasing the rectum from the
posterior vaginal wall.
|
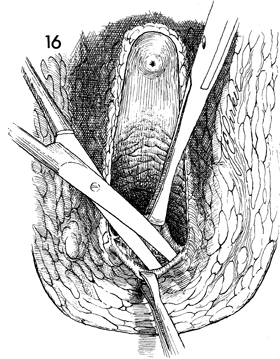
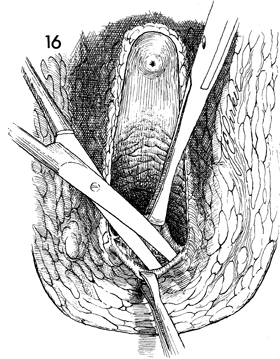
A
Foley catheter is reinserted into the bladder. The wound is
assessed to determine whether it can be closed primarily without
tension by mobilizing adjacent tissue, should the Sure-Closure
skin stretchers be used, or whether it requires a graft or
flap.
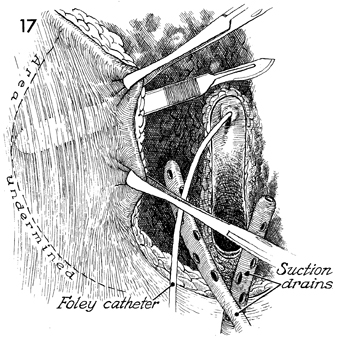
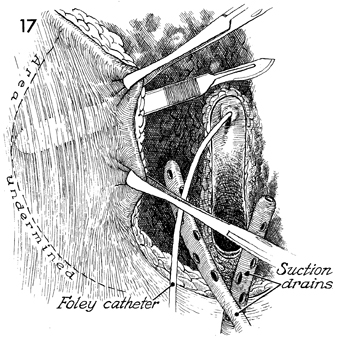
Tissue lateral to the margin
of the wound is undermined by sharp and blunt dissection. Closed
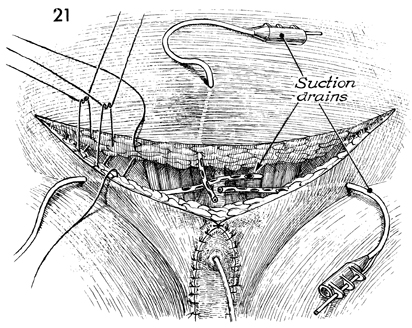
suction drains are placed in the ischial rectal fossa. |
Closure of the wound is begun in the perineal body by suturing
the subcutaneous tissues for 3 or 4 cm up to the posterior fourchette
of the vagina.
The subcutaneous tissue of the thigh is sutured to the paravaginal
tissue up to the level of the urethral meatus.
No attempt is made to suspend the
urethral meatus to the fascia and periosteum of the pubic symphysis
or use it for wound closure. Such a course is apt to produce postoperative
urinary incontinence.
The subcutaneous tissue, from both
sides of the incision lateral to the labia majora up to the pubic
tubercle, is closed to the paravaginal tissue with interrupted
2-0 synthetic absorbable sutures.
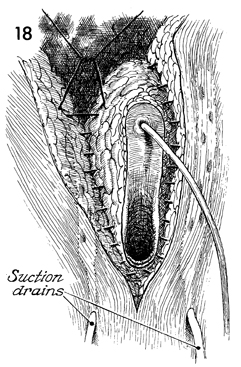
Closed suction drains are placed in the ischial rectal fossa and
under the closure of the vagina to the skin of the thigh. |
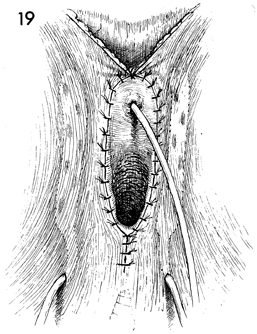
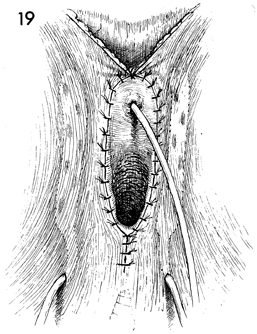
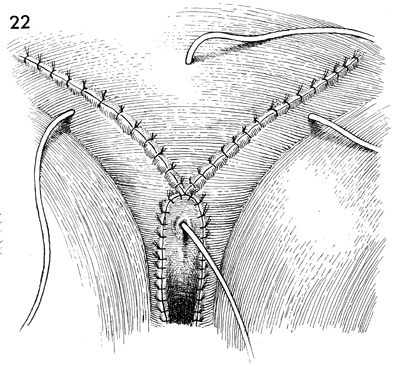
The skin of the perineal body is approximated
with interrupted 3-0 nylon suture. The vaginal mucosa is sutured
to the squamous epithelium around the entire introitus and vestibule
with interrupted 3-0 nylon suture. The skin edges above the urethral
meatus are sutured together for at least 3-4 cm with interrupted
3-0 nylon sutures. |
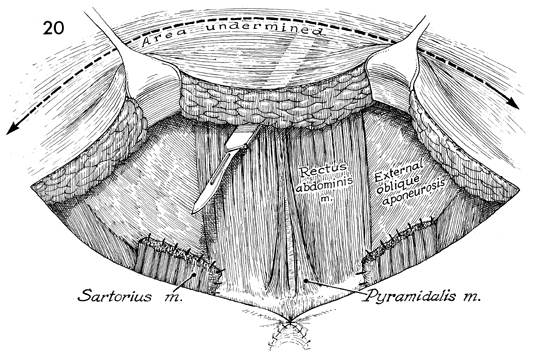
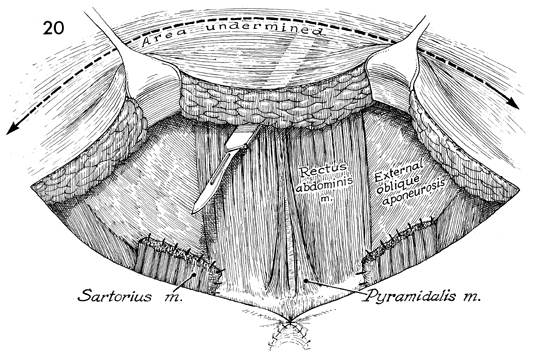
The skin of the lower abdomen is mobilized
up to the umbilicus. There must be no tension on the suture line
between the incision overlying the inguinal ligament and the
margin of the skin of the lower abdomen. |
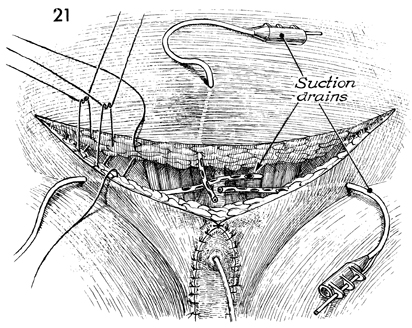
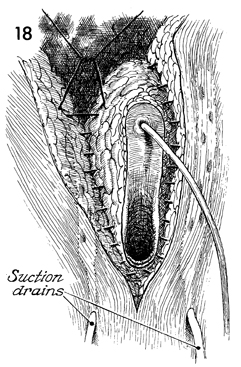
Suction drains are placed in the area of
each sartorius muscle. These are usually sutured to the fascia
with 4-0 synthetic absorbable suture to prevent accidental dislodgement.
They are, however, easily removed with a gentle tug when they
have ceased draining.
The mobilized lower abdomen
is pulled down and sutured to the inguinal area in two layers. |
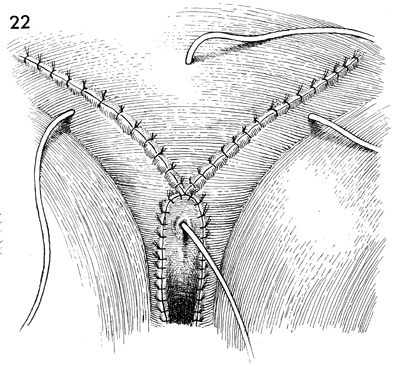
The skin margins have been approximated with
interrupted mattress sutures of 3-0 nylon. Suction drains have
been placed in each inguinal area and through the lower abdomen.
A Foley catheter has been placed in the bladder.
Intermittent pneumonic pressure
cuffs are applied to the lower leg for thromboembolic prophylaxis.
The patient is kept at bed rest for 10 days. |
|