|
||||||
Malignant
Disease: Staging
of Gynecologic Application
of Vaginal Application
of Uterine Afterloading Applicators Abdominal
Injection of Chromic Phosphate Radical
Vulvectomy Reconstruction
of the Transverse
Rectus Colonic
"J" Pouch Rectal Ileocolic Continent Urostomy (Miami Pouch) Construction
of Neoanus Skin-Stretching
System Versus Skin Grafting Gastric
Pelvic Flap for Control
of Hemorrhage in Gynecologic Surgery Repair
of the Punctured Ligation
of a Lacerated Hemorrhage
Control in Presacral
Space What
Not to Do in Case of Pelvic Hemorrhage |
Application
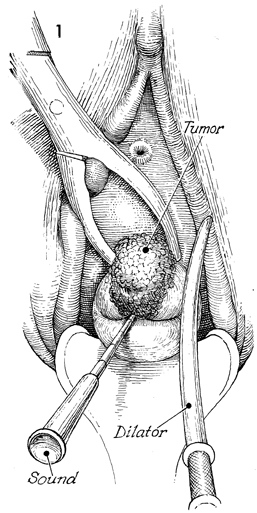
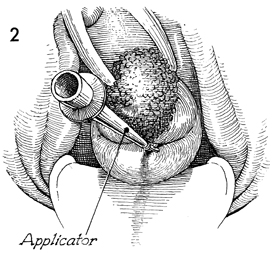
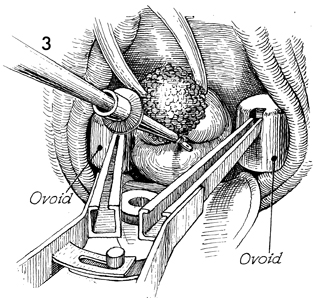
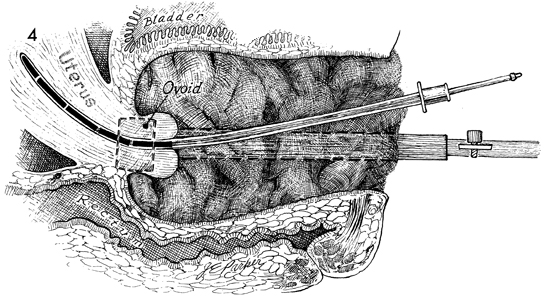
of Uterine Afterloading Therapy for carcinoma of the cervix can be achieved with pelvic irradiation. It is difficult to deliver appropriate doses of ionizing irradiation to the cervix with external beam therapy alone. Therefore, the proper application of intracavitary radiation therapy to the cervix in a manner that produces an isodose curve that will deliver maximum irradiation to the cervix, lower uterine segment, parametrium, and upper vagina is vital. It is not the purpose of intracavitary therapy to irradiate the pelvic wall. This must be done by external beam therapy. To date, a combination of properly applied paracervical and intrauterine irradiation along with external beam therapy has given the best results for cure of carcinoma of the cervix in advanced stages. The purpose of this operation is to apply a uterine tandem with symmetrically placed paracervical ovoids in a manner that will deliver maximum irradiation to the cervix without excessive irradiation to the base of the bladder or rectum. Physiologic Changes. Physiologic changes in this operation are those of ionizing irradiation passing through malignant tissue. Points of Caution. It is vital that the cervical os be identified and the endocervical canal and endometrial cavity be sounded prior to insertion of the intracavitary therapy applicators. This can be one of the most difficult parts of this procedure. The cervical os is generally more posterior than it would seem because the malignant tissue expands from the anterior lip and distorts the configuration of the cervix. The uterine tandem should be inserted into
the entire length of the endometrial canal. The ovoids should be positioned so that they are in the vaginal fornices and there is approximately 3.0 cm between the surfaces of the two ovoids. The upper vagina should not be stretched. Gauze packing should be applied in a manner that gives maximum distance between the sources and the base of the bladder and rectum. Technique
|
|||||
Copyright - all rights reserved / Clifford R. Wheeless,
Jr., M.D. and Marcella L. Roenneburg, M.D.
All contents of this web site are copywrite protected.