Malignant
Disease:
Special Procedures
Staging
of Gynecologic
Oncology Patients With
Exploratory Laparotomy
Subclavian Port-A-Cath
Peritoneal Port-A-Cath
Application
of Vaginal
Cylinders for Intracavitary
Radiation Therapy
Application
of Uterine Afterloading Applicators
for Intracavitary Radiation Therapy
Pelvic High-Dose
Afterloader
Abdominal
Injection of Chromic Phosphate
( ) )
Supracolic
Total Omentectomy
Omental Pedicle "J"
Flap
Tube Gastrostomy
Total Vaginectomy
Radical
Vulvectomy
With Bilateral Inguinal
Lymph Node Dissection
Reconstruction
of the
Vulva With Gracilis Myocutaneous Flaps
Transverse
Rectus
Abdominis Myocutaneous
Flap and Vertical Rectus
Abdominis Myocutaneous
Flap
Radical
Wertheim
Hysterectomy With
Bilateral Pelvic Lymph
Node Dissection and With Extension of the Vagina
Anterior Exenteration
Posterior Exenteration
Total Pelvic
Exenteration
Colonic
"J" Pouch Rectal
Reservoir
Kock Pouch
Continent Urostomy
Omental "J" Flap
Neovagina
Ileocolic
Continent Urostomy (Miami Pouch)
Construction
of Neoanus
Gracilis Dynamic Anal
Myoplasty
Skin-Stretching
System Versus Skin Grafting
Gastric
Pelvic Flap for
Augmentation of Continent Urostomy or Neovagina
Control
of Hemorrhage in Gynecologic Surgery
Repair
of the Punctured
Vena Cava
Ligation
of a Lacerated
Internal Iliac Vein and
Suturing of a Lacerated Common Iliac Artery
Hemorrhage
Control in
Sacrospinous Ligament
Suspension of the Vagina
Presacral
Space
Hemorrhage Control
What
Not to Do in Case of Pelvic Hemorrhage
Packing
for Hemorrhage
Control
Control
of Hemorrhage
Associated With Abdominal Pregnancy |
Reconstruction of the Vulva
With Gracilis Myocutaneous Flaps
The gracilis myocutaneous flap is useful in those cases of large denudated
defects in the perineum following radical vulvectomy or perineal surgery
in which primary closure would likely result in postoperative dehiscence
of the wound incision. It is not substitute for the simpler Z-plasty
pedicle flap that gives adequate results except when an extended area
must be covered.
The principle of a myocutaneous flap is the creation of an island flap
that depends on the underlying muscle for its vascular supply. Of course,
the blood supply to the muscle underneath the flap must remain intact
and viable, or the graft will not survive.
The purpose of the operation is to cover the vulvar
defect with a cutaneous structure having its own non-irradiated or
traumatized blood supply that can produce a healed wound per primam
with a normal functioning vulva.
Physiologic Changes. The predominant physiologic
change is the production of a vulva that is healed per primam without
scarring or contracture.
Points of Caution. Care must be taken to accurately
identify the gracilis muscle and not mistake it for the sartorius muscle.
This is facilitated by extending the knee of the patient while abducting
the hip 30°. With the patient in this position, the gracilis muscle
is generally palpable.
Care must be taken to determine the size of flap needed prior to making
the skin incision over the gracilis muscle. One of the most important
points in the operation is to ensure that the neurovascular bundle
of the gracilis muscle is preserved.
Technique
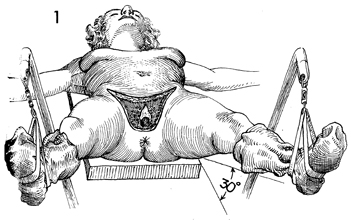
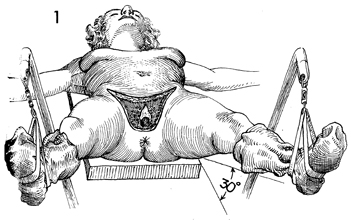
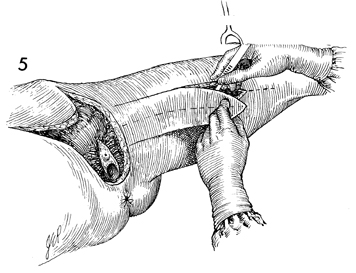
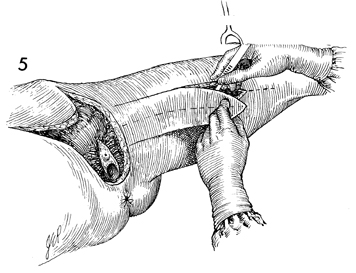
This patient has had a radical vulvectomy
necessitating extensive removal of pelvic tissue. The patient
is in a modified lithotomy position in which the hips are slightly
flexed and the knee is extended but elevated approximately 30° off the operating table. The legs are abducted approximately
30° at the hip joint to give adequate exposure to the perineum
and the skin of the inner thigh. |
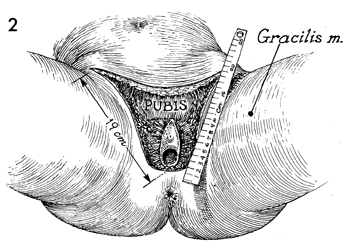
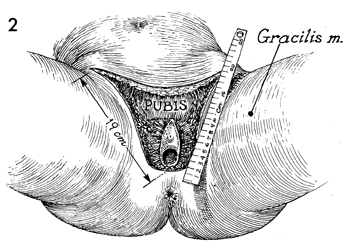
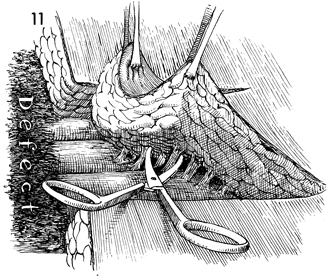
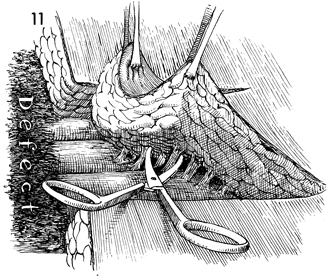
The area of the defect is measured in centimeters
to determine the size of graft needed. With the legs in this
position, the gracilis muscle stands out. Its origin is on the
ischial rami, and its insertion is at the knee. |
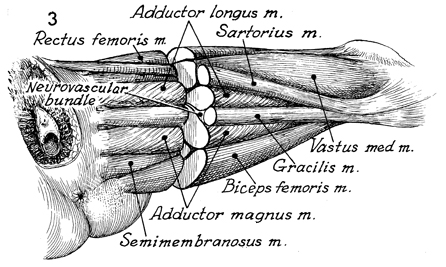
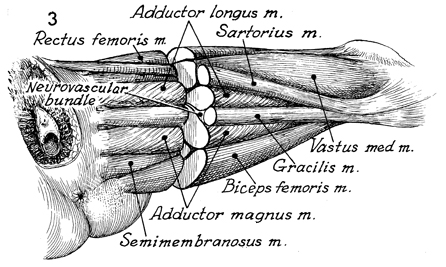
The anatomy of the inner thigh and vulva
is shown, and the important anatomic landmarks are noted. The
gracilis muscle is shown with its insertion on the ischial rami,
with a cross section of the leg demonstrating the location of
the essential neurovascular bundle that enters at the upper third
of the gracilis muscle and exits between the adductor longus
and adductor magnus muscles. Because of this consistent anatomic
arrangement, the gracilis muscle is an ideal structure for the
myocutaneous flap. |
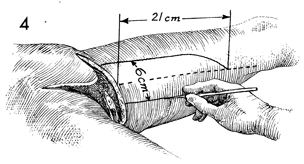
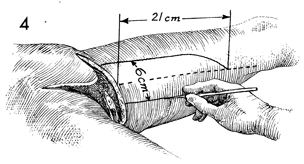
After the measurements taken
in Step 2 are recorded, a line is drawn on the skin down the
middle of the gracilis muscle. A skin flap matching the dimensions
of the defect is outlined on the inner thigh. The maximum flap
that can survive from the neurovascular bundle feeding the gracilis
muscle is approximately 24 x 8 cm. Such a large flap, however,
is rarely required for gynecologic purposes. As demonstrated
in Step 2, the defect in this case measures 19 cm in length and
6 cm in width. Therefore, a flap 21 cm long is drawn, leaving
2 cm of "overage." |
An incision is made full thickness through
the skin and subcutaneous fat down to the muscular bundles. |
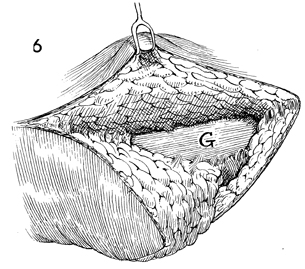
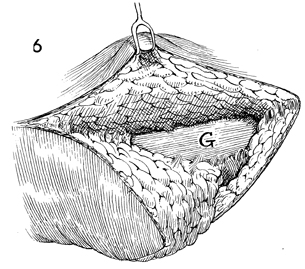
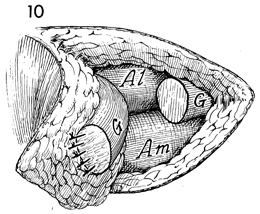
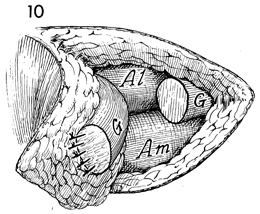
The gracilis muscle (G) must
be identified after the distal skin incisions are made, prior
to extension of the skin incision proximal to the vulvar defect.
Otherwise, skin may be included in the flap that is not supplied
by the gracilis muscle. |
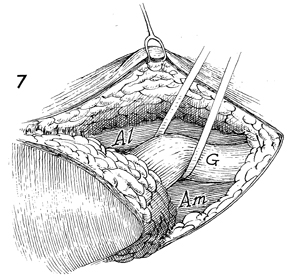
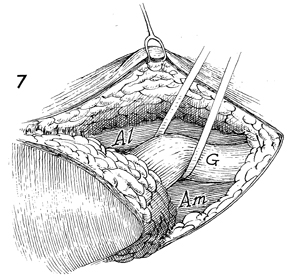
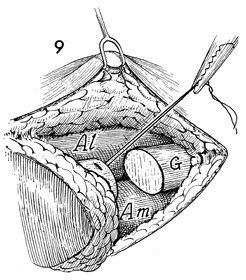
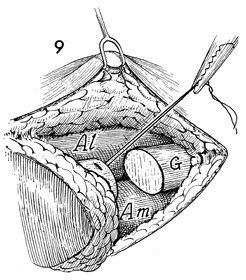
The gracilis muscle (G) is isolated
with an umbilical tape. The adductor longus (Al) and
adductor magnus (Am) muscles are identified. |
 |
|
| The
gracilis muscle is transected. |
The gracilis muscle is sutured
to the overlying subcutaneous flap by interrupted 4-0 synthetic
absorbable sutures. |
The vulvar defect is seen on
the left, and the full-thickness flap is dissected off the underlying
muscle with small Metzenbaum scissors. Extreme care is taken
as the area of the neurovascular bundle is approached. |
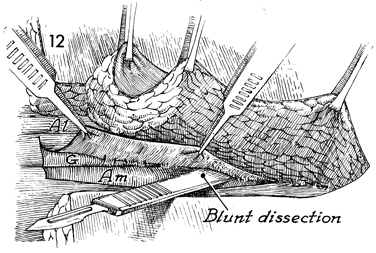
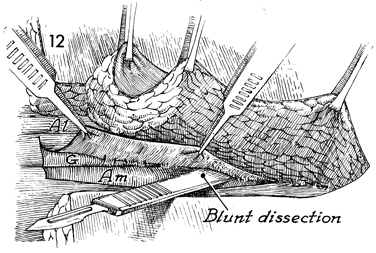
Locating the neurovascular bundle
of the gracilis muscle is vital to success of the procedure.
Identification is facilitated by incising the fascia over the
adductor magnus muscle and dissecting this fascia medially with
a blunt instrument. |
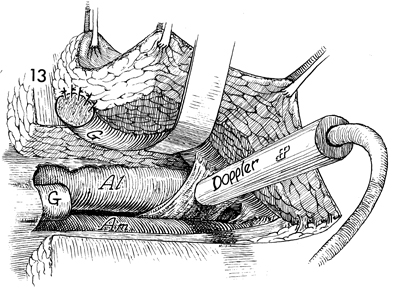
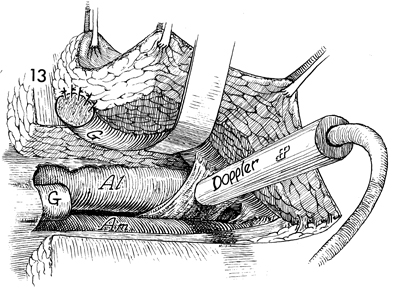
Assistance can be obtained from
a small ultrasound Doppler that can probe each possible pedicle
for the exact location of the gracilis artery and vein. The proximal
portion of the gracilis muscle is transected from the ischial
rami and sutured to the subcutaneous tissue of the graft. At
this point, the gracilis muscle is totally isolated and completely
dependent on its vascular supply that enters from the border
of the adductor longus and adductor magnus muscles. |
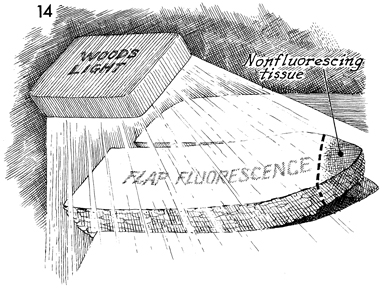
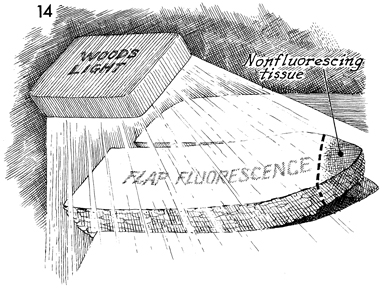
After the flap on the opposite
thigh has been developed, the patient is given 1 g of fluorescein
dye intravenously. After 3-5 minutes, the operating room is darkened,
a Wood's lamp is focused on the myocutaneous flap, and the viable
area of the flap will fluoresce with a brilliant yellow color.
Nonviable areas are rendered as dark purple and should be excised
at this time, as shown in Figure 14. |
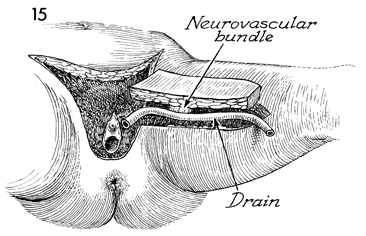
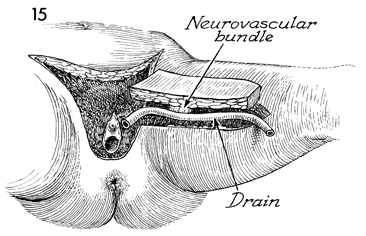
The flap is completely isolated.
The neurovascular bundle is identified. A closed suction drain
is placed in the space previously occupied by the gracilis muscle
and is brought out at the distal end of the leg incision. |
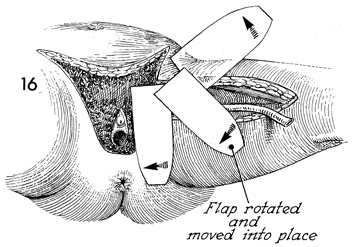
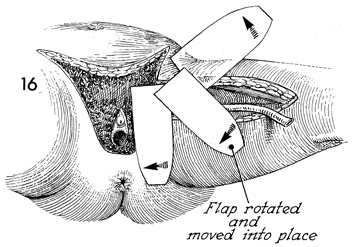
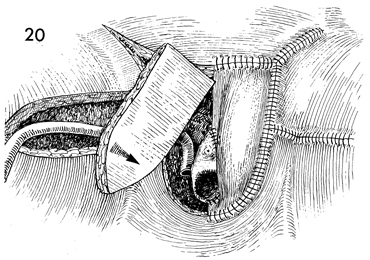
The flap may be rotated clockwise
or counterclockwise, at the discretion of the surgeon, to provide
the best coverage for the vulvar defect. |
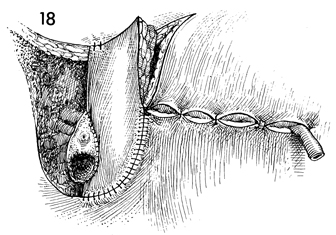
The flap is rotated into place,
and a subcutaneous 3-0 synthetic absorbable suture is placed
between the flap and the edge of the defect. Fine skin sutures
of 4-0 Prolene are placed between the skin and the vulvar defect.
Some surgeons prefer a subcuticular suture of 4-0 Dexon, finding
it less compromising to the vasculature of the flap edge. |
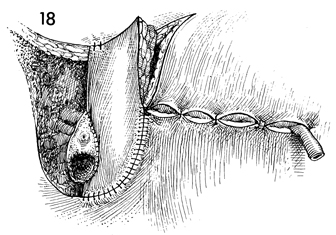
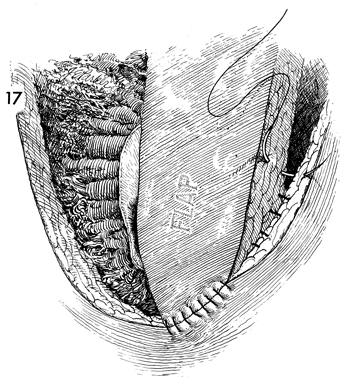
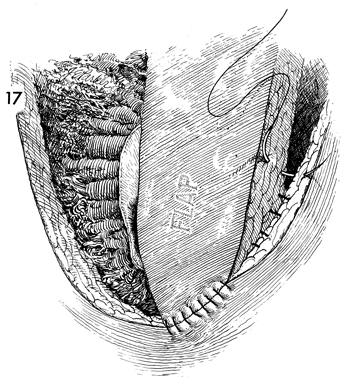
The defect in the leg is closed
in layers with a synthetic absorbable suture. The drain is brought
out through the distal end of the incision. The proximal end
of the drain is placed under the flap. The medial border of the
flap is sutured to the edge of the vagina. |
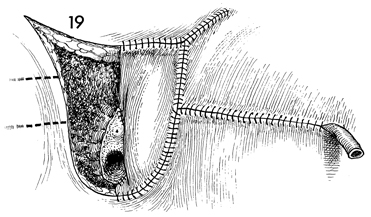
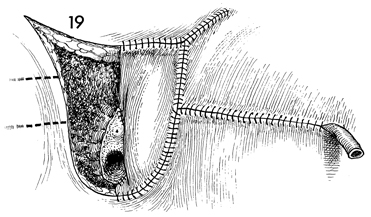
The remaining portion of the
inguinal lymph node dissection has been closed primarily. The
flap on the opposite side has now been drawn on the skin, and
the same procedure is performed from Figures 2 through 18. |
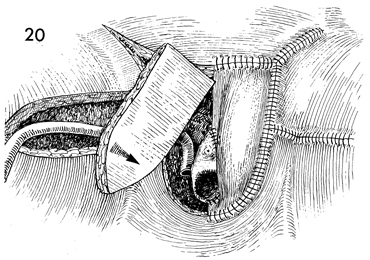
A drain is placed in the space
previously occupied by the gracilis muscle on this side, and
this flap is rotated into position. |
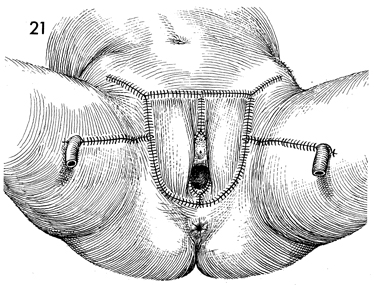
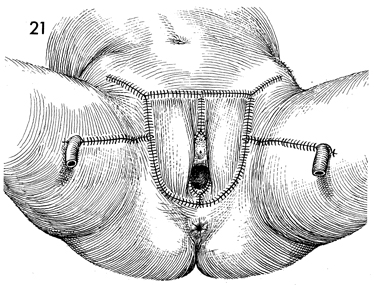
Closure of the vulvar defect
is completed. The leg opening on the opposite side is closed.
The closed suction drains are removed the eighth and twelfth
postoperative days. Sutures are also removed during this time,
depending on the condition of the edges of the flap. |
|
|