|
||||||||||||
Malignant
Disease: Staging
of Gynecologic Application
of Vaginal Application
of Uterine Afterloading Applicators Abdominal
Injection of Chromic Phosphate Radical
Vulvectomy Reconstruction
of the Transverse
Rectus Colonic
"J" Pouch Rectal Ileocolic Continent Urostomy (Miami Pouch) Construction
of Neoanus Skin-Stretching
System Versus Skin Grafting Gastric
Pelvic Flap for Control
of Hemorrhage in Gynecologic Surgery Repair
of the Punctured Ligation
of a Lacerated Hemorrhage
Control in Presacral
Space What
Not to Do in Case of Pelvic Hemorrhage |
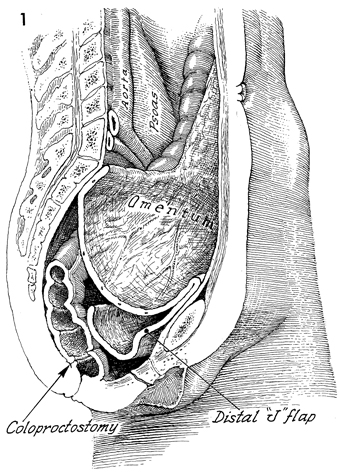
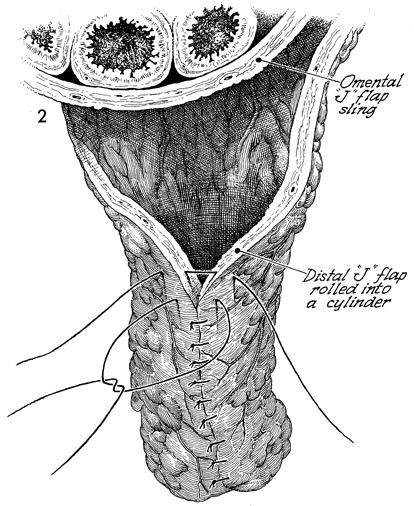
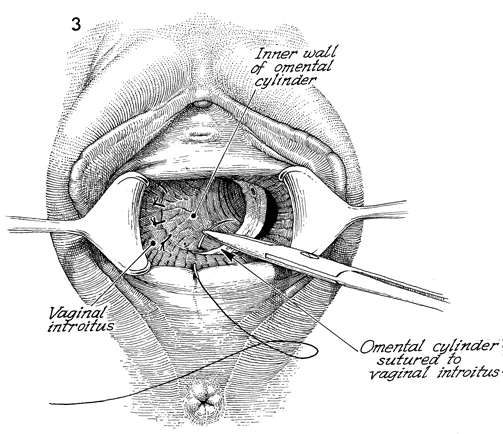
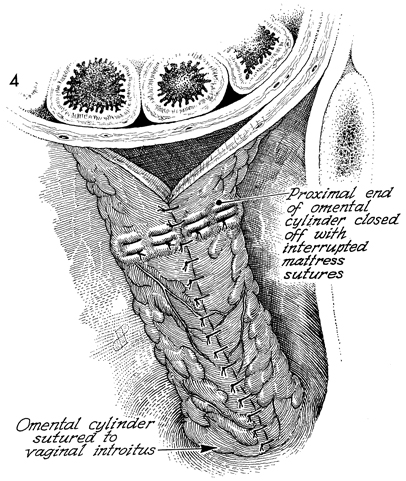
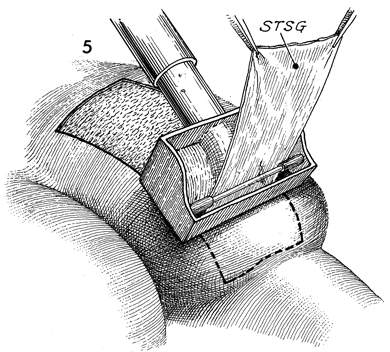
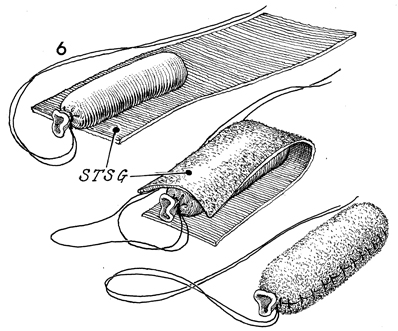
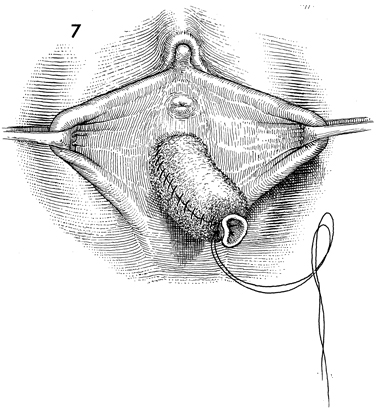
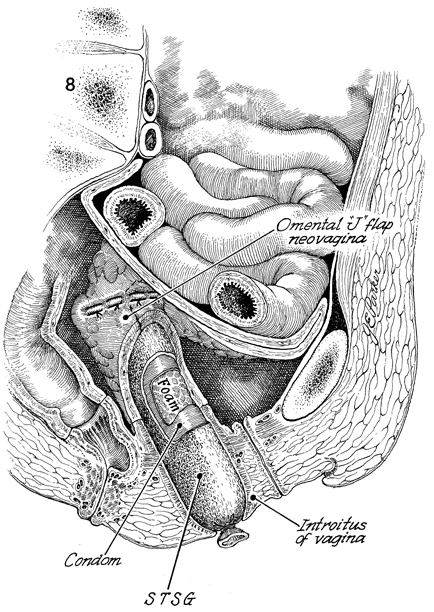
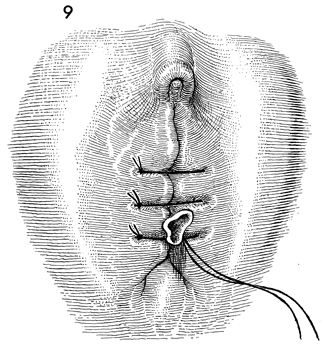
Omental "J" Flap Neovagina Construction of a neovagina has been an accepted gynecologic procedure for many years. McIndoe (see Vagina and Urethra) has described surgical techniques for construction of a neovagina when the bladder is in position anteriorly and the rectum and colon are in position posteriorly. These techniques are inapplicable, however, when patients have undergone total pelvic exenteration with or without low coloproctostomy. Under these circumstances, Berek and Hacker demonstrated that the anterior wall of the neovagina could be made from an omental flap. By modifying the omental flap, which is normally used to close off the pelvic inlet after total pelvic exenteration with or without low coloproctostomy, the surgeon can create a cylinder providing anterior, posterior, and lateral walls for the neovagina. When the cylinder is sutured to the introitus and lined with a skin graft, it becomes a satisfactory functional vagina. Physiologic Changes. The omentum that is enervated by the vagus nerve forms the wall of the neovagina. Normally, tugging or pulling on the omentum does not produce a sensation of pleasure that one would associate with sexual intercourse. Approximately 40% of the patients who have undergone this procedure, however, report that they experience sexual orgasm. Another physiologic change is the development of estrogen hormone receptors on the split-thickness skin graft. Derived from skin on the buttocks or thigh that normally has no hormonal properties, the graft eventually becomes indistinguishable from normal vaginal mucosa on biopsy. At present, it is unknown whether the maturation index of the graft can be influenced by the administration of systemic estrogen, as can occur in normal vaginal mucosa. Points of Caution. If the construction of the neovagina immediately follows total pelvic exenteration, it is important to ensure hemostasis in the pelvic wound before applying the skin graft. If hemostasis is uncertain, the omental neovagina should be packed with gauze or foam rubber covered by a contraceptive condom. Then, when hemostasis is maintained, in approximately 6-12 postoperative days a skin graft can be taken and applied to the vaginal form. After the skin graft has been inserted, the neovagina must remain dilated with a vaginal form until healing is complete. Thereafter, a soft Silastic vaginal form should be worn for 6 months except during intercourse. After this time, the soft Silastic vaginal form is worn only at night if sexual intercourse is not a part of the patient's life. Technique
|
|||||||||||
Copyright - all rights reserved / Clifford R. Wheeless,
Jr., M.D. and Marcella L. Roenneburg, M.D.
All contents of this web site are copywrite protected.