Malignant
Disease:
Special Procedures
Staging
of Gynecologic
Oncology Patients With
Exploratory Laparotomy
Subclavian Port-A-Cath
Peritoneal Port-A-Cath
Application
of Vaginal
Cylinders for Intracavitary
Radiation Therapy
Application
of Uterine Afterloading Applicators
for Intracavitary Radiation Therapy
Pelvic High-Dose
Afterloader
Abdominal
Injection of Chromic Phosphate
( ) )
Supracolic
Total Omentectomy
Omental Pedicle "J"
Flap
Tube Gastrostomy
Total Vaginectomy
Radical
Vulvectomy
With Bilateral Inguinal
Lymph Node Dissection
Reconstruction
of the
Vulva With Gracilis Myocutaneous Flaps
Transverse
Rectus
Abdominis Myocutaneous
Flap and Vertical Rectus
Abdominis Myocutaneous
Flap
Radical
Wertheim
Hysterectomy With
Bilateral Pelvic Lymph
Node Dissection and With Extension of the Vagina
Anterior Exenteration
Posterior Exenteration
Total Pelvic
Exenteration
Colonic
"J" Pouch Rectal
Reservoir
Kock Pouch
Continent Urostomy
Omental "J" Flap
Neovagina
Ileocolic
Continent Urostomy (Miami Pouch)
Construction
of Neoanus
Gracilis Dynamic Anal
Myoplasty
Skin-Stretching
System Versus Skin Grafting
Gastric
Pelvic Flap for
Augmentation of Continent Urostomy or Neovagina
Control
of Hemorrhage in Gynecologic Surgery
Repair
of the Punctured
Vena Cava
Ligation
of a Lacerated
Internal Iliac Vein and
Suturing of a Lacerated Common Iliac Artery
Hemorrhage
Control in
Sacrospinous Ligament
Suspension of the Vagina
Presacral
Space
Hemorrhage Control
What
Not to Do in Case of Pelvic Hemorrhage
Packing
for Hemorrhage
Control
Control
of Hemorrhage
Associated With Abdominal Pregnancy |
Construction
of Neoanus Gracilis
Dynamic Anal Myoplasty
In cases where the anal sphincter has become incompetent or when both
the anus and anal sphincter have been removed (as in sublevator total
pelvic exenteration or abdominoperineal resection), the surgeon may
perform a neoanus dynamic anal myoplasty. The operation has been performed
in Europe for 8 years and will come to the United States, pending Food
and Drug Administration (FDA) approval.
Physiologic Changes. The
dynamic anal myoplasty operation attempts to restore the anus so
that normal defecation can occur by using the gracilis muscle and
a modified cardiac pacemaker. The anus and anal sphincter are rebuilt
with the gracilis muscle, and a pacemaker is attached to the muscle.
When the muscle is electronically stimulated, it produces an anal
pressure that is greater than the colonic pressure, allowing the
patient to maintain continence. When the electrical current is withdrawn,
however, the gracilis muscle relaxes, the anal pressure falls to
a level below that of the colon, and the patient pushes down and
defecates. The on-and-off switch for the modified cardiac pacemaker
is a simple magnet.
Points of Caution. The
integrity of the neurovascular bundle of the gracilis muscle must
be carefully preserved, as it is dissected from the leg. Adjustment
of the cardiac pacemaker for voltage and frequency can be made externally.
Technique
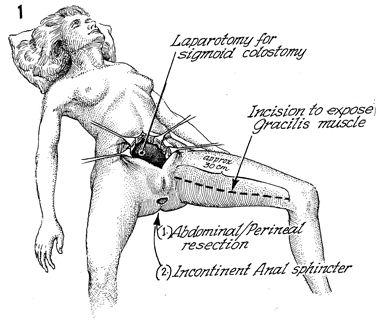
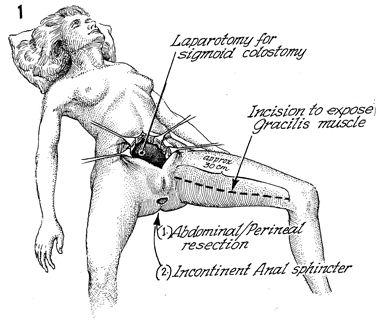
The patient is shown having had a laparotomy
following abdominal perineal resection. With the patient in the
dorsal supine modified lithotomy position with the leg extended
and knee flexed, the gracilis muscle is palpated. An incision
is made of approximately 30 cm, extending from the pubis ramus
to the tubercle on the knee. |
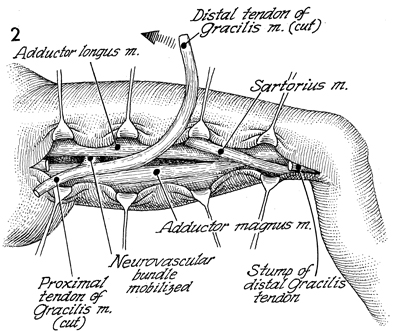
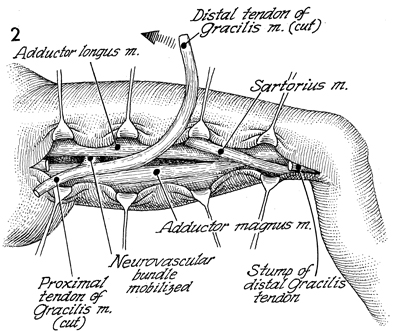
The adductor longus, the gracilis,
and the adductor magnus muscles are identified. The vital neurovascular
bundle of the gracilis muscle is located and dissected. The gracilis
muscle is transected at the so-called "goose foot" as it inserts
on the knee and is transected proximally, adjacent to the ramus
of the ischium. Care must be taken to identify the sartorius
muscle and not confuse this with the gracilis muscle. The stump
of the distal gracilis muscle tendon is seen adjacent to the
knee. |
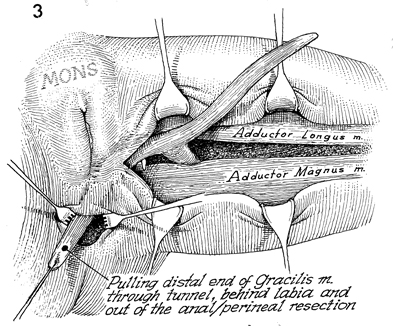
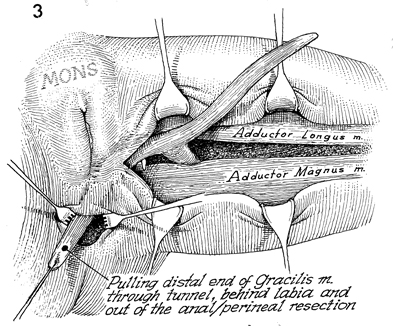
A tunnel is made under the posterior fourchette
of the vagina, under the perineal body, and around the anus with
sharp and blunt dissection. If it is a case of anal sphincter
incompetence or a pull-through procedure from a previously existing
abdominal perineal resection, the muscle is pulled through, with
the gracilis neurovascular muscle kept intact. |
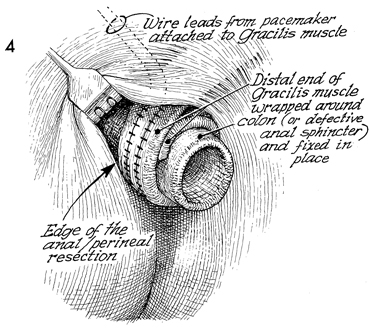
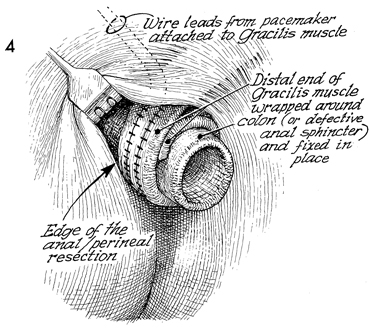
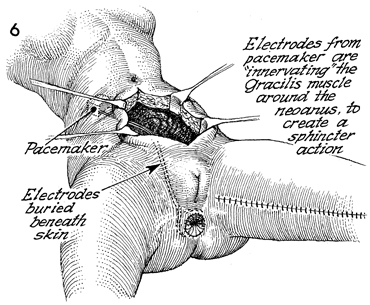
The entire gracilis muscle
is pulled through the tunnel and wrapped around the colon or
defective anal sphincter and is fixed in place with interrupted
sutures. The margin of the anal skin incision is shown for those
cases where the anus and the anal sphincter have been completely
removed. The wire leads from the modified cardiac pacemaker are
attached to the gracilis muscle at the junction of the neurovascular
bundle to the muscle and confirmed in this position by electronically
stimulating the device while the incision is open. |
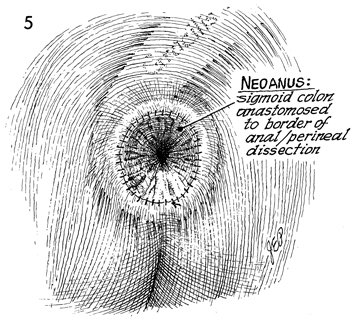
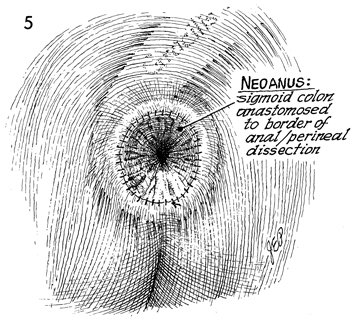
The neoanus is shown with the sigmoid colon
anastomosed to the border of the anus or perianal skin. The gracilis
muscle is shown ghosted underneath. |
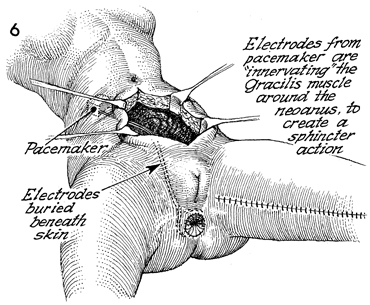
The wire leads are brought
through the subcutaneous tunnel to a site that is selected for
the modified cardiac pacemaker on the abdominal wall. The wound
in the left leg has been repaired over Jackson-Pratt suction
drains. |
|