Malignant
Disease:
Special Procedures
Staging
of Gynecologic
Oncology Patients With
Exploratory Laparotomy
Subclavian Port-A-Cath
Peritoneal Port-A-Cath
Application
of Vaginal
Cylinders for Intracavitary
Radiation Therapy
Application
of Uterine Afterloading Applicators
for Intracavitary Radiation Therapy
Pelvic High-Dose
Afterloader
Abdominal
Injection of Chromic Phosphate
( ) )
Supracolic
Total Omentectomy
Omental Pedicle "J"
Flap
Tube Gastrostomy
Total Vaginectomy
Radical
Vulvectomy
With Bilateral Inguinal
Lymph Node Dissection
Reconstruction
of the
Vulva With Gracilis Myocutaneous Flaps
Transverse
Rectus
Abdominis Myocutaneous
Flap and Vertical Rectus
Abdominis Myocutaneous
Flap
Radical
Wertheim
Hysterectomy With
Bilateral Pelvic Lymph
Node Dissection and With Extension of the Vagina
Anterior Exenteration
Posterior Exenteration
Total Pelvic
Exenteration
Colonic
"J" Pouch Rectal
Reservoir
Kock Pouch
Continent Urostomy
Omental "J" Flap
Neovagina
Ileocolic
Continent Urostomy (Miami Pouch)
Construction
of Neoanus
Gracilis Dynamic Anal
Myoplasty
Skin-Stretching
System Versus Skin Grafting
Gastric
Pelvic Flap for
Augmentation of Continent Urostomy or Neovagina
Control
of Hemorrhage in Gynecologic Surgery
Repair
of the Punctured
Vena Cava
Ligation
of a Lacerated
Internal Iliac Vein and
Suturing of a Lacerated Common Iliac Artery
Hemorrhage
Control in
Sacrospinous Ligament
Suspension of the Vagina
Presacral
Space
Hemorrhage Control
What
Not to Do in Case of Pelvic Hemorrhage
Packing
for Hemorrhage
Control
Control
of Hemorrhage
Associated With Abdominal Pregnancy |
Subclavian Port-A-Cath
Oncology patients frequently require central venous access by catheter
for chemotherapy, parenteral nutrition, and blood withdrawal. In some
patients, after multiple surgical procedures and/or chemotherapy, venous
access to the arms rapidly becomes unavailable. The same technique
for Port-A-Cath can be used for Hickman and Gresbourg catheters required
for total parenteral nutrition.
Physiologic Changes. Because there is greater blood
flow through the central veins than through the peripheral veins, parenteral
nutrition and chemotherapy can be administered through the central
lines with less risk of causing chemical phlebitis.
Points of Caution. The patient must
be placed in the Trendelenburg position. This increases the central
venous pressure and avoids the possibility of an air embolism rising
in the central venous system.
The guidewire or catheter should not be
left in the atrium because its presence may cause arrhythmia.
The Silastic catheter should never be pulled back through the shaft
of a needle. The tip of the needle can lacerate the catheter and release
it as a foreign body within the venous system.
To prevent the development
of a gas embolus, all syringes or catheters that are placed in the
central venous system should be filled with a heparinized saline solution.
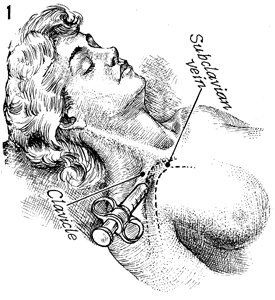
Technique
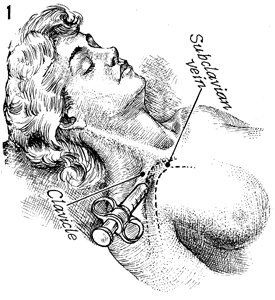
The patient is placed in a 15° Trendelenburg position to increase central venous pressure and
thereby reduce the chances of air embolism. The subclavian vein
has greater exposure if the shoulders are hyperextended over
a rolled towel placed longitudinally between the scapula under
the thoracic spine. The head should be turned to the opposite
side. Under these conditions, the subclavian vein becomes more
accessible. The skin over the neck and upper thorax is prepped
in a routine fashion. Aseptic technique should be followed. A
2-inch, 14-gauge needle attached to a 10-mL syringe with 2-3
mL of heparinized saline solution in the syringe should be inserted
through the skin with the bevel of the needle pointing down.
The ideal site for the puncture is at the inferior border of
the middle of the clavicle directed toward a fingertip pressed
firmly into the suprasternal notch. The needle should be passed
beneath the inferior margin of the clavicle in a horizontal plane
and directed toward the anterior margin of the trachea at the
level of the suprasternal notch. The needle and syringe are kept
parallel to the surface of the patient's bed and adjacent to
the anterior wall of the subclavian vein in the direction of
its long axis. The accuracy of the placement into the subclavian
vein can be demonstrated by a copious flow of blood into the
barrel of the syringe with slight negative pressure. The syringe
is removed from the hub of the needle, and the thumb is immediately
placed over the hub. |
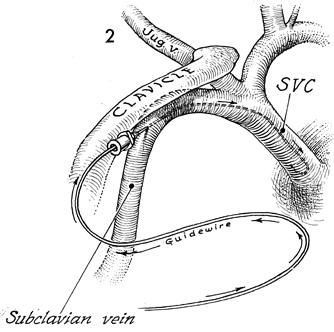
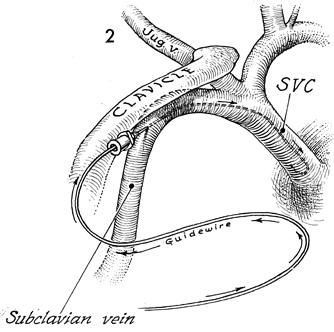
A flexible guidewire is inserted through
the hub of the needle and passes into the superior vena cava
(SVC).
When the guidewire is securely
in the superior vena cava, the needle is withdrawn over the guidewire
and removed. |
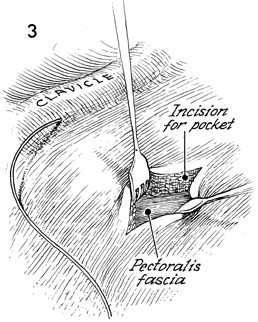
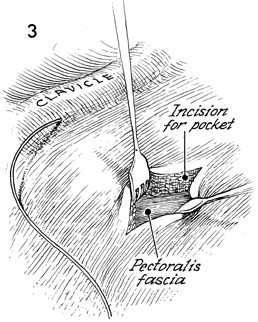
The guidewire is shown as it enters the skin
under the clavicle. The ideal site for the Port-A-Cath chamber
is selected; it is between two ribs, approximately 8cm from the
point where the guidewire enters the skin. A 4-cm incision is
made in this area, and a pocket is created under the subcutaneous
fat on top of the pectoralis fascia. Hemostasis in this pocket
is essential. |
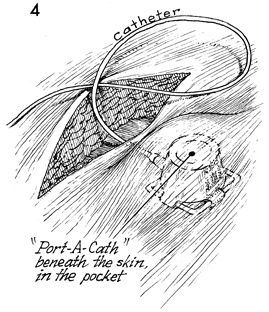
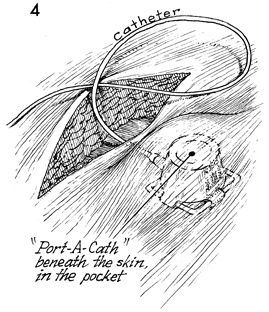
The subcutaneous pocket is
demonstrated by placing the Port-A-Cath, with the catheter attached,
into the pocket. At this point, the eyes on the Port-A-Cath flange
are sutured to the fascia of the pectoralis muscle with 3-0 nylon
sutures.
The Port-A-Cath and the catheter
are filled with heparinized saline solution. This is achieved
by inserting a Huber needle attached to a syringe of heparinized
saline. The entire Port-A-Cath and catheter are filled with saline
solution before any attempt is made to insert the catheter into
the venous system. |
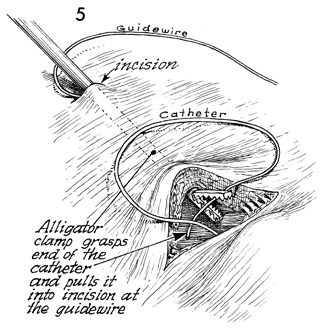
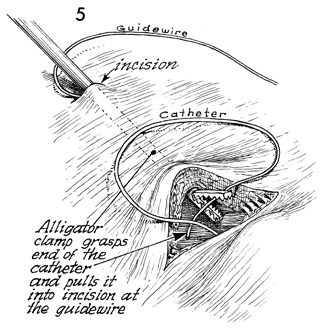
A 1-cm incision is made adjacent to the guidewire
underneath the clavicle. An alligator-mouth grasping forceps
is tunneled through the small incision down to the larger subcutaneous
pocket. The alligator-mouth jaws grasp the catheter and pull
it through the subcutaneous pocket, out through the incision
next to the guidewire in the subclavian vein. |
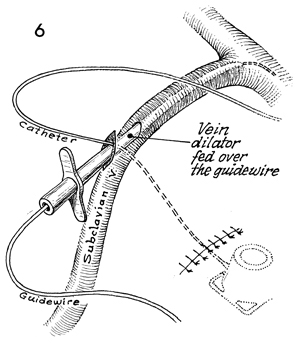
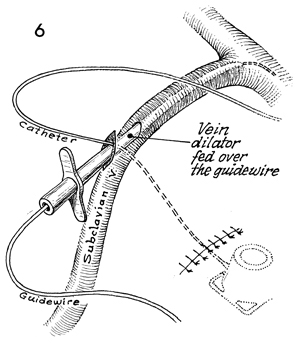
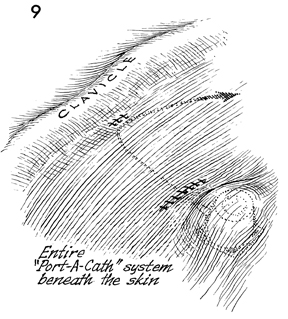
The Port-A-Cath chamber is
shown at the lower right. The skin incision over the Port-A-Cath
is closed with fine suture or the skin stapler. At this point,
a vein dilator sheath is inserted over the guidewire through
the 1-cm skin incision under the clavicle and down into the subclavian
vein. Note that the catheter exits the skin adjacent to the vein
dilator sheath. |
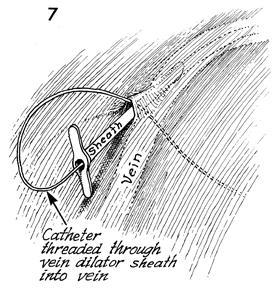
The guidewire is withdrawn through the vein
dilator sheath and removed. A finger is inserted over the vein
dilator to prevent air from entering the subclavian vein. The
Port-A-Cath catheter is measured from the subcutaneous pocket
up to the subclavian vein and down an estimated distance in the
superior vena cava. The excess catheter is cut away with sharp
scissors.
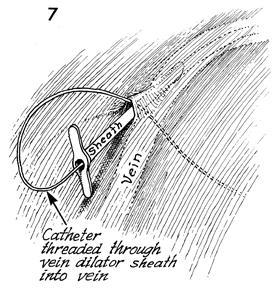
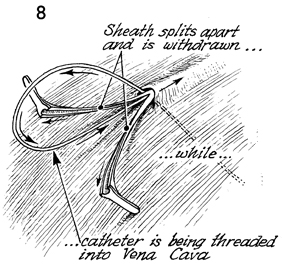
The catheter is threaded through
the vein dilator sheath into the subclavian vein and, ultimately,
into the superior vena cava. |
|
 |
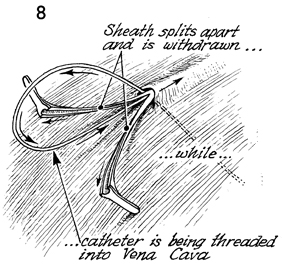
The
vein dilator sheath is constructed so that it will tear away
as it is pulled out of the subclavian vein. This is achieved
by placing the finger on each flange of the vein dilator sheath.
An assistant threads the catheter farther into the superior vena
cava. The sheath is withdrawn as it is split apart. The vein
dilator sheath is removed entirely.
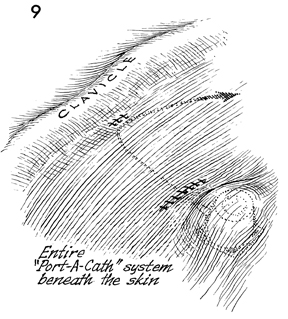
At this time an x-ray picture is taken (either
by fluoroscopy or from the flat plate of the chest) to ascertain
the position of the catheter. If it is in the right atrium, it
is withdrawn 4-5 cm through the skin incision. When the catheter
is in the appropriate position, the skin incision is closed with
fine suture or skin staples. A heparinized saline solution in a
10-mL syringe with a Huber needle is placed through the skin into
the Silastic diaphragm Port-A-Cath, and the entire system is flushed
with 10mL of heparinized saline solution. |
|