Malignant
Disease:
Special Procedures
Staging
of Gynecologic
Oncology Patients With
Exploratory Laparotomy
Subclavian Port-A-Cath
Peritoneal Port-A-Cath
Application
of Vaginal
Cylinders for Intracavitary
Radiation Therapy
Application
of Uterine Afterloading Applicators
for Intracavitary Radiation Therapy
Pelvic High-Dose
Afterloader
Abdominal
Injection of Chromic Phosphate
( ) )
Supracolic
Total Omentectomy
Omental Pedicle "J"
Flap
Tube Gastrostomy
Total Vaginectomy
Radical
Vulvectomy
With Bilateral Inguinal
Lymph Node Dissection
Reconstruction
of the
Vulva With Gracilis Myocutaneous Flaps
Transverse
Rectus
Abdominis Myocutaneous
Flap and Vertical Rectus
Abdominis Myocutaneous
Flap
Radical
Wertheim
Hysterectomy With
Bilateral Pelvic Lymph
Node Dissection and With Extension of the Vagina
Anterior Exenteration
Posterior Exenteration
Total Pelvic
Exenteration
Colonic
"J" Pouch Rectal
Reservoir
Kock Pouch
Continent Urostomy
Omental "J" Flap
Neovagina
Ileocolic
Continent Urostomy (Miami Pouch)
Construction
of Neoanus
Gracilis Dynamic Anal
Myoplasty
Skin-Stretching
System Versus Skin Grafting
Gastric
Pelvic Flap for
Augmentation of Continent Urostomy or Neovagina
Control
of Hemorrhage in Gynecologic Surgery
Repair
of the Punctured
Vena Cava
Ligation
of a Lacerated
Internal Iliac Vein and
Suturing of a Lacerated Common Iliac Artery
Hemorrhage
Control in
Sacrospinous Ligament
Suspension of the Vagina
Presacral
Space
Hemorrhage Control
What
Not to Do in Case of Pelvic Hemorrhage
Packing
for Hemorrhage
Control
Control
of Hemorrhage
Associated With Abdominal Pregnancy |
Anterior Exenteration
When irradiation has failed in the treatment of pelvic cancers in
the anterior plane of the pelvis, anterior exenteration may be performed.
The operation is also efficacious for some cases of carcinoma of the
urethra and bladder in which the vagina or cervix was invaded.
The purpose
of the operation is to remove the bladder, urethra, vagina, uterus,
and all tissues lateral to the pelvic side wall, including the tissue
in the obturator fossa. The rectum and colon are left intact.
Physiologic Changes. The predominant physiologic
alteration is elimination of the bladder and lower ureters and the
formation of an urinary diversion.
Points of Caution. As soon as possible, the hypogastric
artery on both sides should be identified and ligated to reduce blood
loss. The ureter should not be transected until the surgeon is absolutely
confident that the tumor is resectable. When the ureter is cut, it
should be cut as low in the pelvis as possible, leaving ample ureter
for construction of the urinary diversion.
The pelvis should be closed
with a lid from an omental flap to prevent small bowel contents from
falling into the denuded pelvis and adhering to the radiated tissue
therein.
If the pelvis has been adequately irradiated, a complete lymphadenectomy
is not performed.
Technique

The patient is placed on the operating table
in the modified dorsal lithotomy position with the hips abducted
approximately 30°, exposing the perineum. The entire abdominal
wall, vulva, perineal area, and vagina are surgically prepared.
A Foley catheter is inserted in the bladder.
The abdomen is opened through
a large lower midline incision that is extended around the umbilicus.
The abdomen is thoroughly explored for tumor.
The bowel is packed
off, exposing the pelvic brim. The peritoneum below the cecum
and terminal ileum is opened, and the common iliac artery and aorta
are exposed. The aorta is explored all the way to the renal vessels,
and any suspicious lymph nodes are removed. |
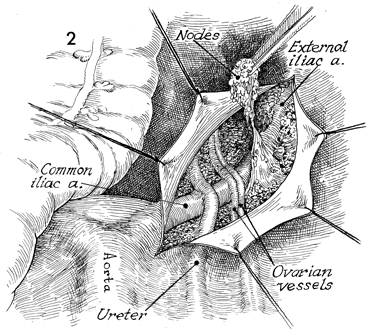
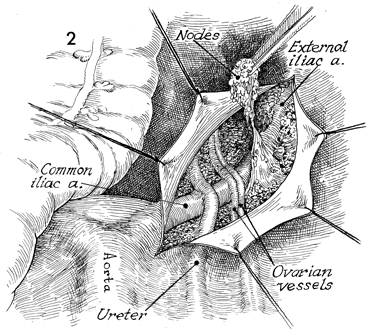
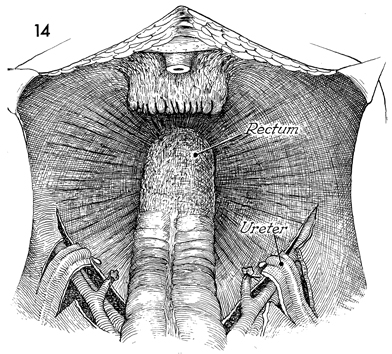
The peritoneum has been opened from the bifurcation
of the aorta to the femoral canal, and suspicious lymph nodes
have been dissected off the common iliac artery. The ureter crosses
the common iliac artery on the right side, medial and inferior
to the ovarian vessels. |
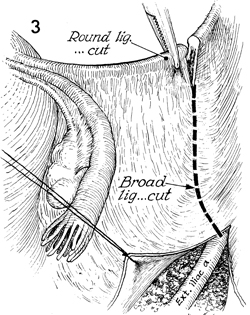
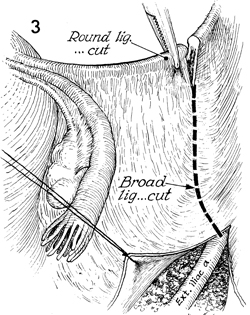
The round ligaments on each side are cut
at the pelvic wall, and the posterior and anterior leaves of
the broad ligament are completely opened. |
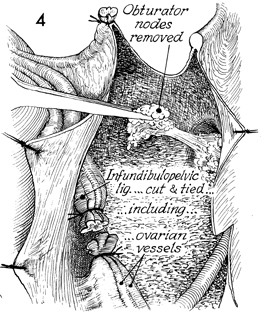
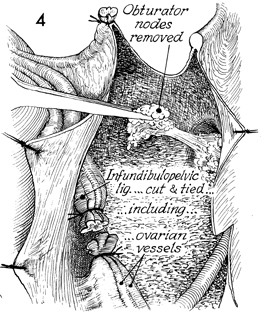
The external iliac vein is
deviated laterally, exposing the obturator fossa from which all
lymph nodes suspected of bearing tumor are removed. The ovarian
vessels are clamped and doubly tied at the pelvic brim. |
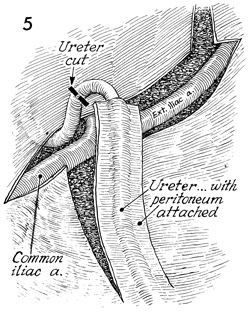
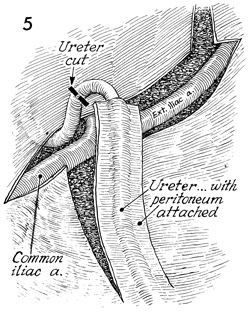
The ureter, with a generous portion of its
peritoneal attachment left intact, is transected below the common
iliac artery. |
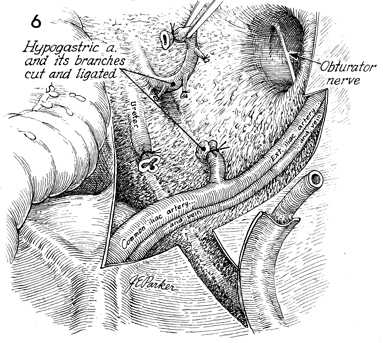
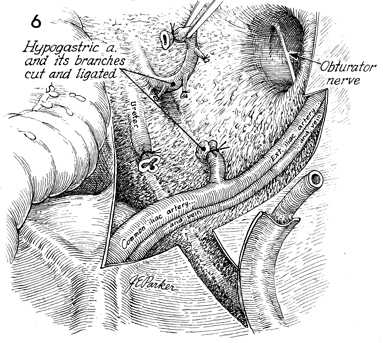
The ureter has been transected,
and the distal ureter has been ligated. The obturator fossa has
been cleaned of all contents. The hypogastric artery is cross-clamped,
transected, and tied with 2-0 suture. The distal portion of the artery
is elevated, and its branches are identified, clamped, and tied. |
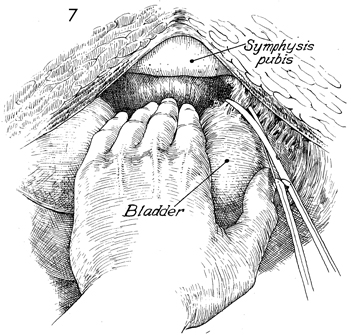
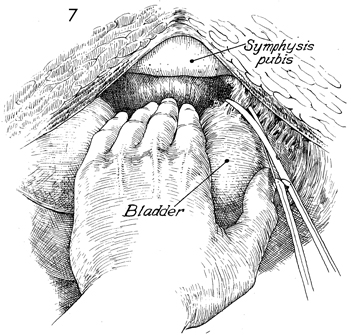
Attention is directed to the space of Retzius
where the bladder is separated from the rectopubic space. Fine
adhesions to the pelvic wall can be lysed with Metzenbaum scissors;
and any small vessels in the plexus of Santorini can be clamped
and tied with suture, or hemoclips may be applied. |
This view illustrates the pelvic
spaces. In an anterior exenteration, both the paravesical spaces
(PVS) and the pararectal spaces (PRS) are seen. The lateral extent
of the cardinal ligament (the web) is demonstrated with countertraction
from the first two fingers of the surgeon's hand. The web is
clamped, incised, and tied at the pelvic wall. B, bladder; PSS,
presacral space; R, rectum; RVS, rectovaginal
space; SR, space of Retzius; and VVS, vesicovaginal
space. |
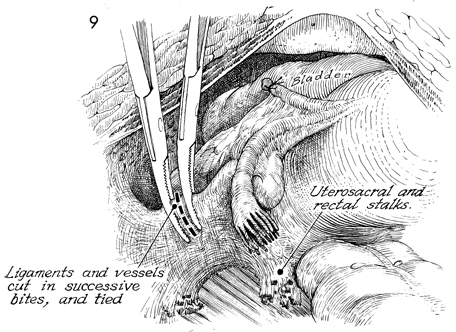
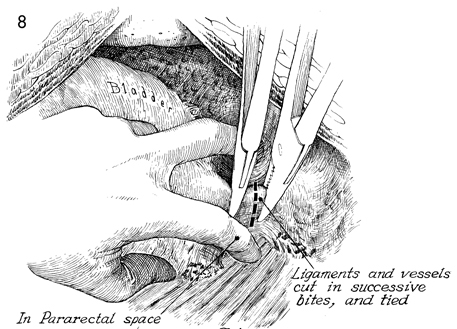
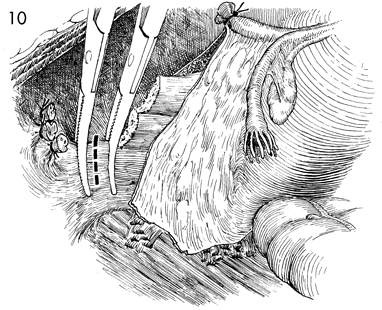
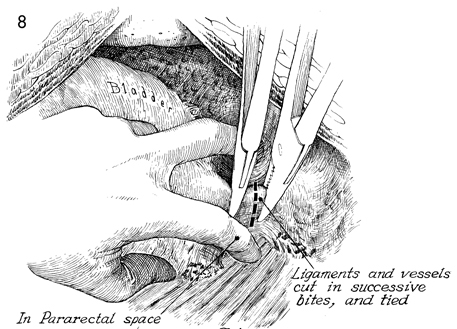
The stumps of the ureterosacral ligament
are seen transected adjacent to the pelvic wall, which includes
the hypogastric venous plexus. Successive bites on the web at
the pelvic wall are made with clamps and incised down to the
levator ani muscles. The rectum remains intact. |
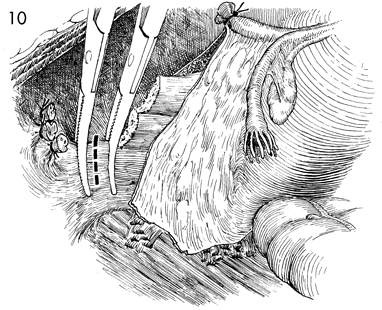
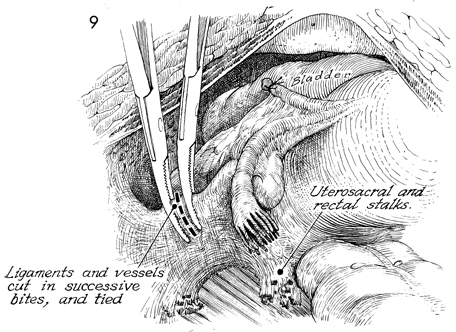
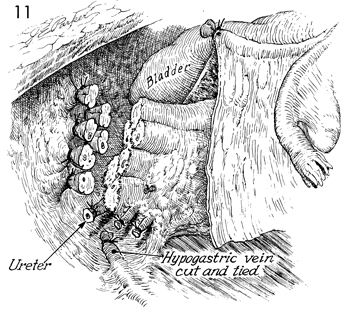
The hypogastric vein and artery have been
cut and tied. The stumps of the web are seen on the pelvic wall.
The specimen has been completely freed down to the levator sling
and is retracted medially. The ureterosacral ligaments have been
cut and tied at the pelvic wall. The peritoneum of the cul-de-sac
of Douglas has been transected, and the posterior vaginal wall
has been dissected off the rectum. |
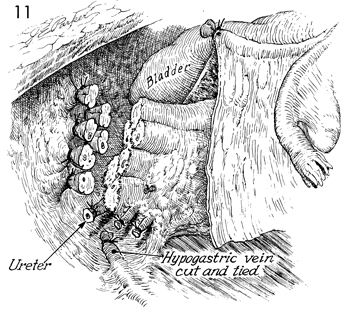
The same procedure is carried out on the
opposite side. The ligated ureter is seen. The specimen (bladder,
uterus, tubes, ovaries, and vagina) has been freed from the anterior
lateral pelvic wall. |
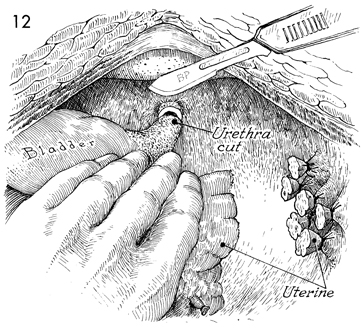
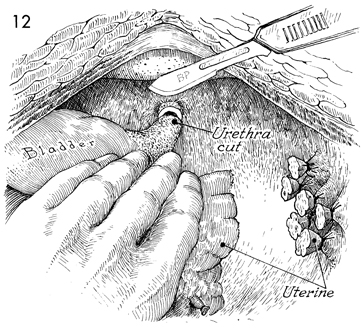
The specimen is now retracted cephalad. A
scalpel is used to transect the urethra at the meatus. |
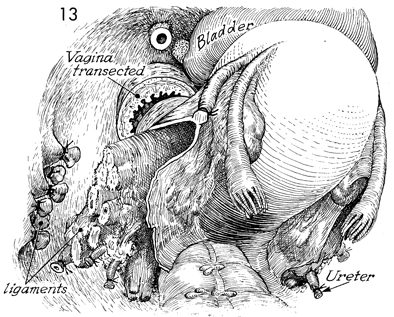
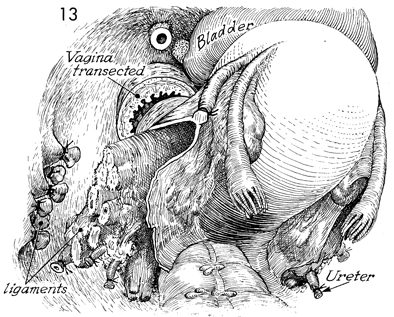
The vagina is transected across the introitus
below the level of the levator sling. Any remaining rectal stalks
attaching the posterior vaginal wall to the rectum are lysed,
and the specimen is removed. |
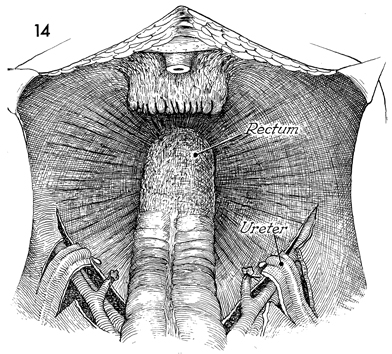
The vaginal cuff has been closed with an
interrupted 0 absorbable suture. The ureters are seen below the
pelvic brim. The urethra has been transected at the meatus. Maximum
attention at this stage is turned toward hemostasis within the
pelvis. |
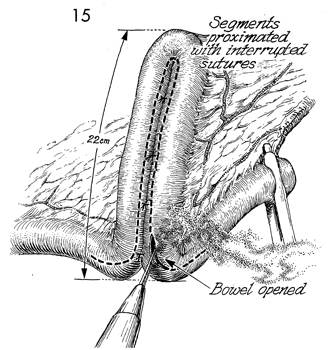
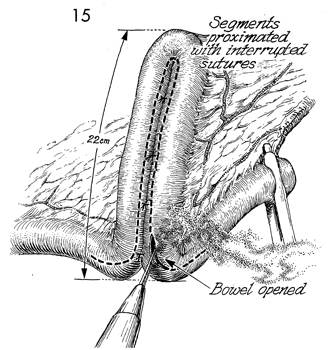
A continent urinary diversion (Kock pouch)
will be made from small bowel. The terminal ileum with the respective
links in centimeters for construction of the pouch is shown (see
the Kock Pouch Continent Urostomy). |
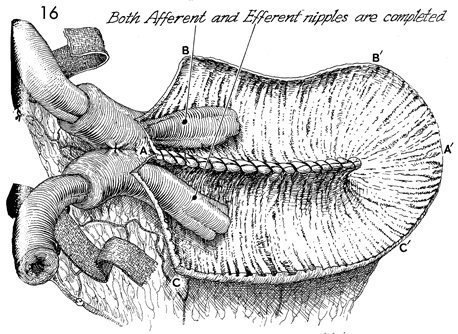
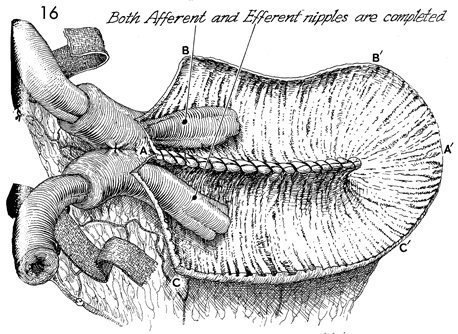
The Kock pouch continent urostomy
with afferent and efferent nipples has been completed. The letters A to A', B to B', C to C' delineate
the order of suture that produces a spherical pouch. |
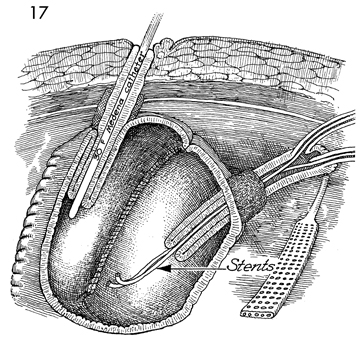
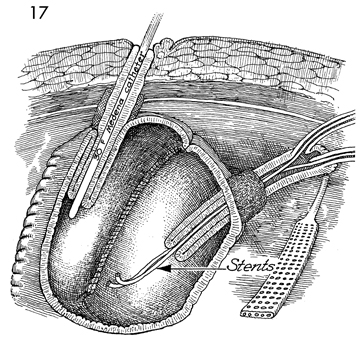
The continent pouch has been completed. The
stoma is sutured to the subcuticular layer of the skin of the
umbilicus with 3-0 polyglycolic acid (PGA) sutures. A
No. 30 French Medena catheter has been placed through the stoma
down the efferent limb and exits the efferent nipple into the
pouch. This Medena catheter has been securely sutured in place
with No. 1 nylon suture that includes the margins of the skin,
the entire intestinal wall of the stoma, the opposite intestinal
wall, and the opposite margin of skin; it is securely tied around
the Medena catheter with multiple half-hitch knots to hold the
catheter in the pouch without slippage for 3 weeks. A second
suture of No. 1 nylon is placed on the opposite side.
A Jackson-Pratt closed suction
drain has been placed adjacent to the Kock pouch and is brought
out through the abdominal wall. It is sutured with a 3-0 PGA
suture to prevent removal for 3 weeks. Note that the afferent
limb of the bowel and the afferent nipple have the ureters sutured
in a mucosa-to-mucosa fashion with No. 8 French Finney "J" Silastic
stents in place. The abdomen is closed. The Medina catheter is
irrigated every 2-4 hours for the next 3 weeks to prevent mucus
obstruction. |
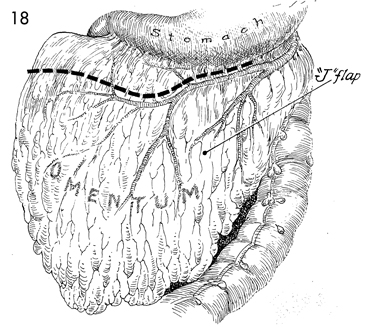
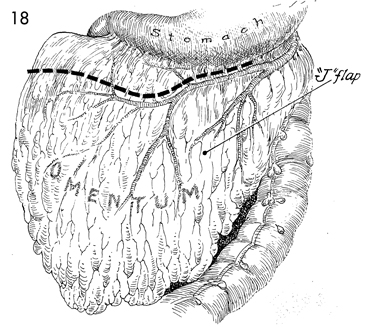
An omental vascular pedicle
"J" flap is created. |
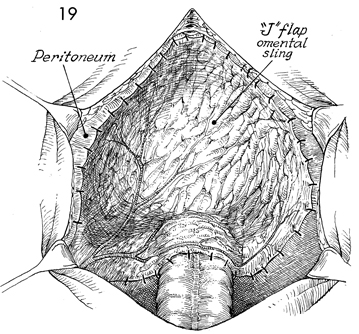
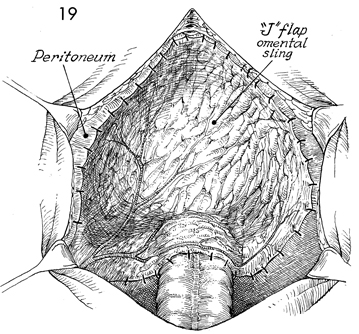
The omental "J" flap is brought
into the pelvis and sutured around the ileopectineal line and
across the rectosigmoid colon as a pelvic lid. The abdomen is
closed in layers. A sump nasogastric tube or a feeding gastrostomy
tube is inserted in the stomach. |
|
|