Malignant
Disease:
Special Procedures
Staging
of Gynecologic
Oncology Patients With
Exploratory Laparotomy
Subclavian Port-A-Cath
Peritoneal Port-A-Cath
Application
of Vaginal
Cylinders for Intracavitary
Radiation Therapy
Application
of Uterine Afterloading Applicators
for Intracavitary Radiation Therapy
Pelvic High-Dose
Afterloader
Abdominal
Injection of Chromic Phosphate
( ) )
Supracolic
Total Omentectomy
Omental Pedicle "J"
Flap
Tube Gastrostomy
Total Vaginectomy
Radical
Vulvectomy
With Bilateral Inguinal
Lymph Node Dissection
Reconstruction
of the
Vulva With Gracilis Myocutaneous Flaps
Transverse
Rectus
Abdominis Myocutaneous
Flap and Vertical Rectus
Abdominis Myocutaneous
Flap
Radical
Wertheim
Hysterectomy With
Bilateral Pelvic Lymph
Node Dissection and With Extension of the Vagina
Anterior Exenteration
Posterior Exenteration
Total Pelvic
Exenteration
Colonic
"J" Pouch Rectal
Reservoir
Kock Pouch
Continent Urostomy
Omental "J" Flap
Neovagina
Ileocolic
Continent Urostomy (Miami Pouch)
Construction
of Neoanus
Gracilis Dynamic Anal
Myoplasty
Skin-Stretching
System Versus Skin Grafting
Gastric
Pelvic Flap for
Augmentation of Continent Urostomy or Neovagina
Control
of Hemorrhage in Gynecologic Surgery
Repair
of the Punctured
Vena Cava
Ligation
of a Lacerated
Internal Iliac Vein and
Suturing of a Lacerated Common Iliac Artery
Hemorrhage
Control in
Sacrospinous Ligament
Suspension of the Vagina
Presacral
Space
Hemorrhage Control
What
Not to Do in Case of Pelvic Hemorrhage
Packing
for Hemorrhage
Control
Control
of Hemorrhage
Associated With Abdominal Pregnancy |
Hemorrhage
Control in Sacrospinous Ligament Suspension of the
Vagina
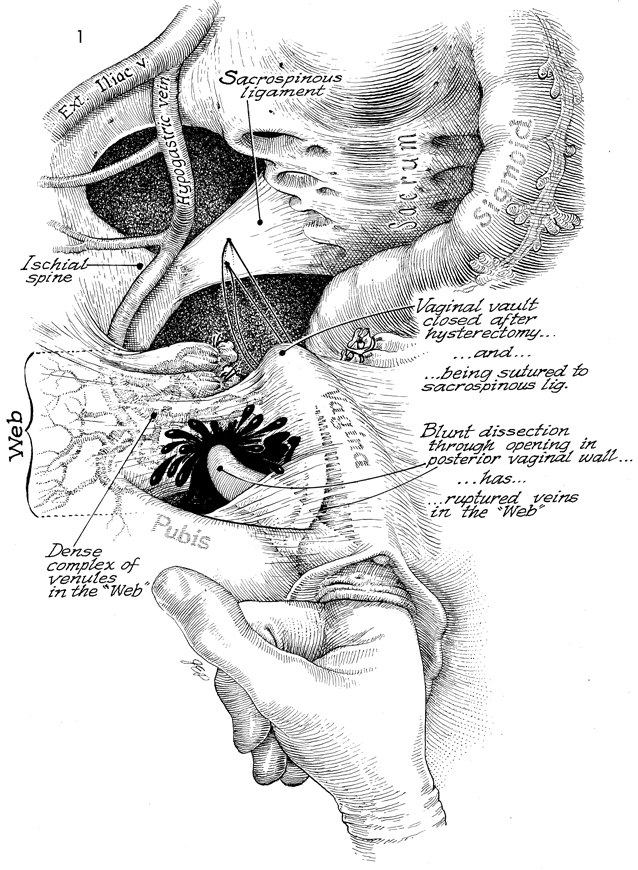
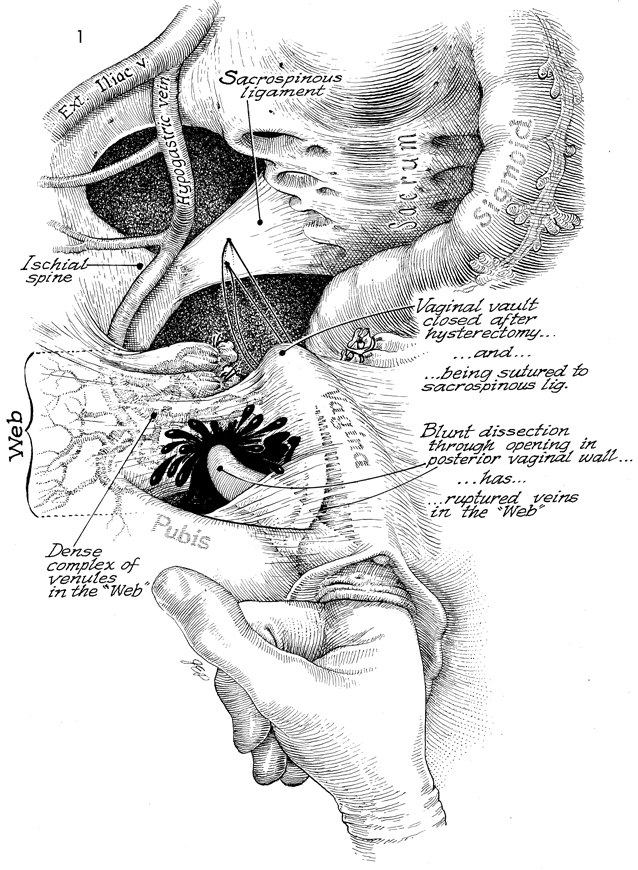
Control of hemorrhage from branches of the internal iliac vein in
sacrospinous ligament suspension of the vagina can be difficult. Dissection
anterior to the iliac spine can enter the lateral extension of the
cardinal ligament (the web). This structure is filled with branches
of the internal iliac veins. Disruption of these veins produces copious
hemorrhage.
Technique
|
Figure
1 illustrates the anatomy in the posterior pelvis. At the top
is the external iliac vein with the internal iliac vein (hypogastric
vein) coming off cephalad to the sacrospinous ligament. The
ischial spine is seen with the attached sacrospinous ligament
traveling to the sacrum. The sigmoid colon is located on the
left. The surgeon has placed sutures in the top of the prolapsed
vagina and the pulley stitch as well as the secure stitch to
the sacrospinous ligament approximately 4 cm (2 finger widths)
from the ischial spine to avoid the pudendal artery nerve and
vein. The vaginal vault has been closed after the hysterectomy
has been performed; the pedicles from the hysterectomy are
shown tied. The so-called web, the lateral extent of the cardinal
ligament, is shown in the brackets between the pararectal space
and the rectovaginal space. This web contains a dense complex
of veins that are branches of the internal iliac (hypogastric)
vein.
Hemorrhage can occur by blunt
dissection through opening the posterior vaginal wall. The
dissection enters the rectovaginal space. This can occur when
the surgeon carries the dissection too far anteriorly rather
than extending the finger dissector posteriorly toward the
sacrum and palpating the ischial spine. When the dissection
is carried into the web and the branches of the internal iliac
(hypogastric) vein have been lacerated, copious hemorrhage
will occur through the vagina. Individual identification with
clamping and tying of individual venous branches of the hypogastric
vein is rarely possible.
|
The
solution to this problem is the placing of packs immediately
into the pararectal space against the bleeding branches of
the veins. When hemorrhage is under control the packs can be
rolled slightly laterally and inferiorly. With a long Allis
clamp the branches of these veins can be picked up individually.
It is extremely difficult to tie off each branch separately.
Therefore, a fine synthetic absorbable suture is used to suture-ligate
the plexus. After each lacerated venous plexus has been sutured,
the pack is further rolled inferiorly and laterally until all
branches of the hypogastric vein have been grasped with the
long thoracic Allis clamp and each one of the branches is sutured
with fine synthetic absorbable suture. This procedure carries
some risk to the ureter. At this point, the anesthesiologist
should administer 1 ampule of indigo carmine dye intravenously.
A water cystoscope should be inserted transurethrally into
the bladder. The ureteral orifice on the affected side should
be observed for the production of blue urine through the ureteral
orifice. If after 10 minutes of observation no urine is seen,
a ureteral catheter should be inserted up the ureter on the
affected side. If the hemorrhage is controlled and the ureter
has been sutured, the surgeon faces two possibilities: (1)
to individually unligate the sutured veins until the ureter
can be identified and a ureteral stent passed up to the kidney,
or (2) to proceed above, open the abdomen, and dissect out
the ureter, removing the offending sutures. The veins can be
religated under direct observation after opening the paravesical
and pararectal spaces. |
|