Malignant
Disease:
Special Procedures
Staging
of Gynecologic
Oncology Patients With
Exploratory Laparotomy
Subclavian Port-A-Cath
Peritoneal Port-A-Cath
Application
of Vaginal
Cylinders for Intracavitary
Radiation Therapy
Application
of Uterine Afterloading Applicators
for Intracavitary Radiation Therapy
Pelvic High-Dose
Afterloader
Abdominal
Injection of Chromic Phosphate
( ) )
Supracolic
Total Omentectomy
Omental Pedicle "J"
Flap
Tube Gastrostomy
Total Vaginectomy
Radical
Vulvectomy
With Bilateral Inguinal
Lymph Node Dissection
Reconstruction
of the
Vulva With Gracilis Myocutaneous Flaps
Transverse
Rectus
Abdominis Myocutaneous
Flap and Vertical Rectus
Abdominis Myocutaneous
Flap
Radical
Wertheim
Hysterectomy With
Bilateral Pelvic Lymph
Node Dissection and With Extension of the Vagina
Anterior Exenteration
Posterior Exenteration
Total Pelvic
Exenteration
Colonic
"J" Pouch Rectal
Reservoir
Kock Pouch
Continent Urostomy
Omental "J" Flap
Neovagina
Ileocolic
Continent Urostomy (Miami Pouch)
Construction
of Neoanus
Gracilis Dynamic Anal
Myoplasty
Skin-Stretching
System Versus Skin Grafting
Gastric
Pelvic Flap for
Augmentation of Continent Urostomy or Neovagina
Control
of Hemorrhage in Gynecologic Surgery
Repair
of the Punctured
Vena Cava
Ligation
of a Lacerated
Internal Iliac Vein and
Suturing of a Lacerated Common Iliac Artery
Hemorrhage
Control in
Sacrospinous Ligament
Suspension of the Vagina
Presacral
Space
Hemorrhage Control
What
Not to Do in Case of Pelvic Hemorrhage
Packing
for Hemorrhage
Control
Control
of Hemorrhage
Associated With Abdominal Pregnancy |
Posterior Exenteration
Posterior exenteration is rarely indicated today in the treatment
of carcinoma of the cervix and upper vagina. The patterns of presentation
of malignancy frequently make this operation inadequate and leave the
bladder denervated; and the frequency of fistulae is significant. In
most cases, we would perform a total exenteration.
Where indicated, the opportunity for reconstruction with a permanent
diverting colostomy was dramatically improved by the advent of the
EEA (end-to-end anastomosis) automatic surgical stapler for very low
colonic anastomoses. It is now possible to achieve the anastomosis
of the descending colon to the rectum at levels at or below the levator
sling, thus allowing the en bloc removal of some pelvic cancers without
a permanent colostomy. Basically, a posterior exenteration is a combination
of a radical Wertheim hysterectomy and an anterior resection of the
colon or abdominal peritoneal resection of the rectosigmoid colon or
anus.
The purpose of this operation is to remove the uterus, tubes, ovaries,
rectosigmoid colon, and all parametrial tissue from the uterus to the
pelvic wall.
Physiologic Changes. The
predominant physiologic change is removal of the tumor from the pelvic
cavity. Denervation of the urinary bladder in most cases occurs,
but the actual loss of a small segment of rectosigmoid colon produces
little clinical or physiologic change.
Points of Caution. The procedure should not be performed
on patients with epidermoid cancer when there is metastasis to the
common iliac and aortic lymph nodes.
The proximal colon should be transected as low in the
pelvis as possible to permit the maximum amount of colon to be available
for reanastomosis and construction of a rectal "J" pouch.
The surgeon should take care to identify the left ureter when opening
the mesentery of the rectosigmoid colon.
The dissection of the ureter in the tunnel must be performed with meticulous
surgical technique to avoid vesicovaginal fistula.
Throughout this operation, hemorrhage must be carefully controlled.
Technique
The patient is placed on the operating table
in the modified dorsal lithotomy position with the hips abducted
30°. A Foley catheter is inserted into the bladder. The skin
from the breast to the perineal area is surgically prepared.
The abdomen is opened through
a lower midline incision extended around the umbilicus. Pfannenstiel
incisions are not appropriate for this operation.
The abdominal
cavity should be explored, and all suspicious areas of tumor
should be identified and removed for frozen section analysis. |
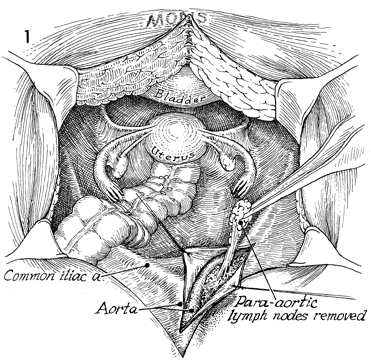
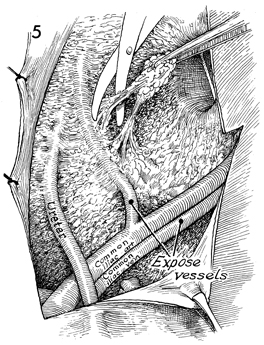
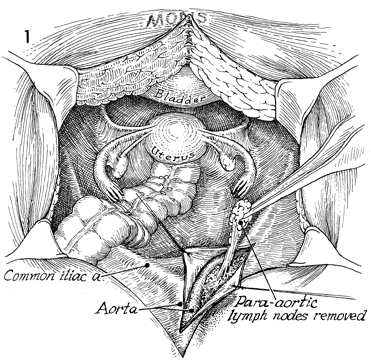
Once the decision has been made to proceed
with the operation, the peritoneum is opened along the right
common iliac artery down to the external iliac artery. All lymphatic
tissue is removed, with care taken to preserve the ureter. The
ovarian vessels seen crossing the common iliac artery will be
ligated. |
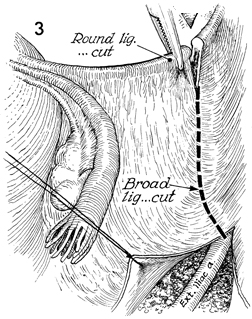
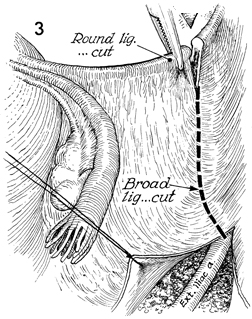
The round ligament is clamped, transected,
and tied at the pelvic wall. The posterior leaf of the broad
ligament is opened, and the entire external iliac artery is exposed. |
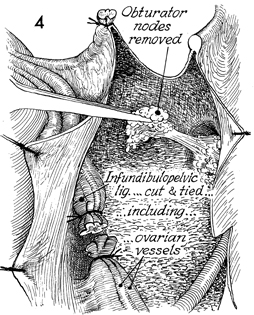
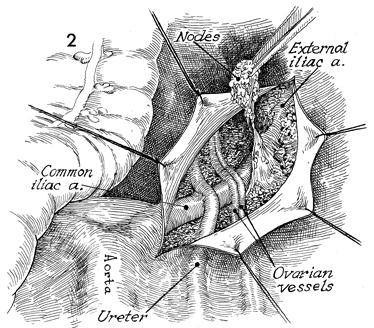
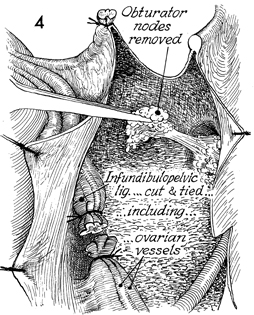
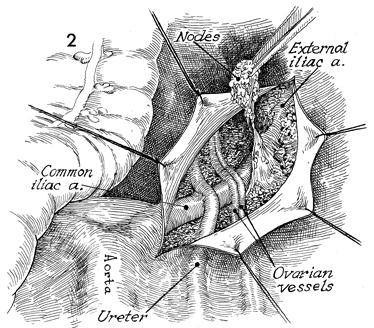
The lymph nodes are removed
from the external iliac artery, vein, and obturator fossa. The
ovarian vessels are clamped, transected, and tied. The same procedure
is performed on the other side. |
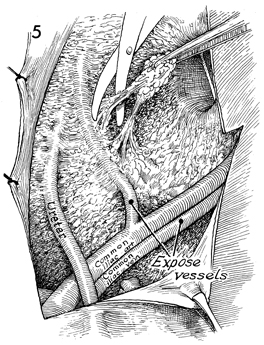
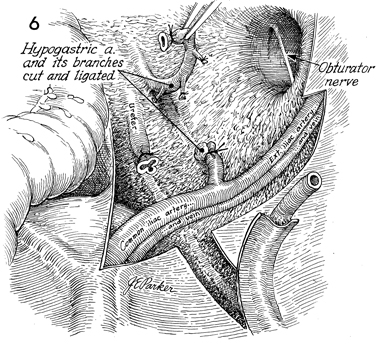
The hypogastric artery is cleaned of lymph
node tissue. The ureter can be seen medial to the hypogastric
artery crossing the common iliac artery. The obturator nerve
is seen in the obturator fossa. |
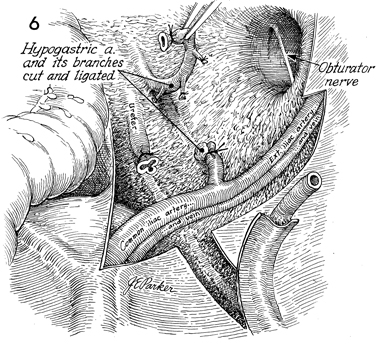
The obturator fossa has been
cleaned of lymph nodes, and the obturator nerve has been preserved.
The hypogastric artery is clamped, ligated, and incised with
its branches. The same procedure is carried out on the opposite
side. |
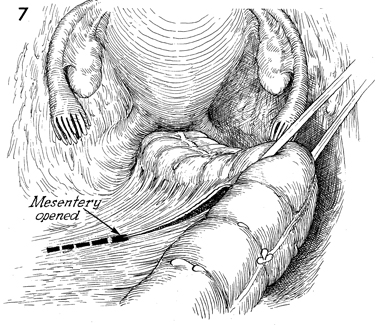
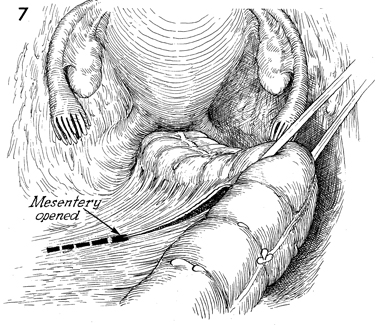
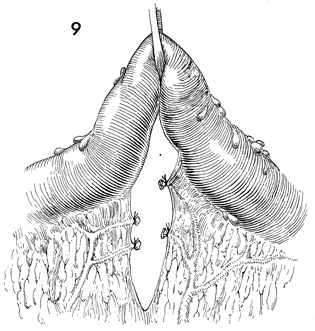
The mesentery of the rectosigmoid colon is
opened in an avascular area, and a rubber drain is passed through
this opening as a source of traction on the colon. The peritoneum
covering the mesentery is opened. Care is taken at this point
to identify the left ureter because the mesentery of the rectosigmoid
colon generally points to the left ureter at its base. |
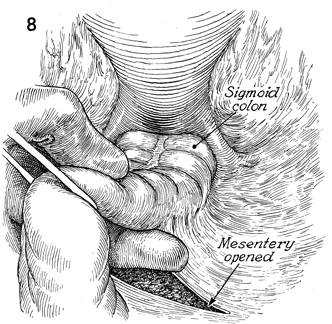
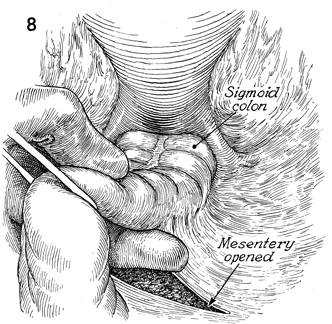
The colon is retracted caudad. A finger has
been inserted in the opening of the mesentery under the rectosigmoid
colon. The peritoneum covering the medial side of the mesentery
is opened. |
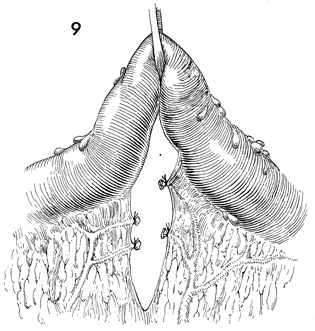
The vessels in the mesentery of the rectosigmoid
colon have been clamped and tied with 2-0 suture. |
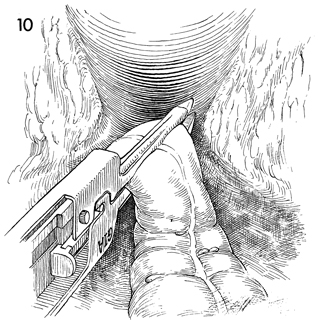
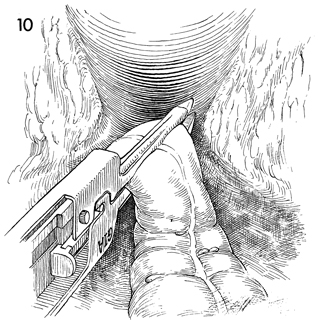
The linear stapler has been applied to the
rectosigmoid colon slightly below the sacral promontory. It is
activated, transecting the rectosigmoid colon between double
rows of staples. |
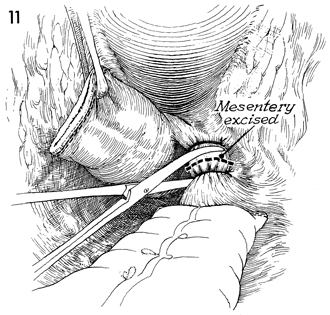
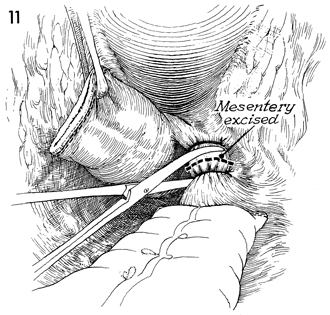
The remaining portion of the mesentery attached
to the rectum is clamped, incised, and tied with 2-0 suture. |
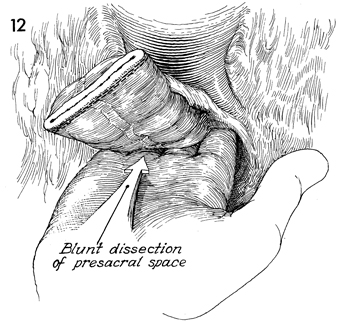
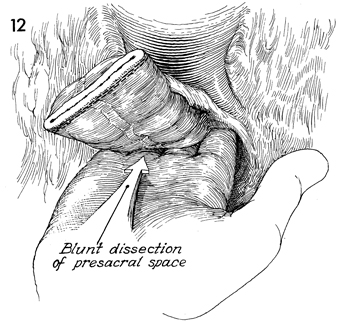
Cephalad retraction is made on the combined
specimen of the uterus and rectosigmoid colon. A hand is inserted
into the presacral space to dissect the rectum from the sacrum
down to the coccyx.
It is important to keep the
dissecting hand in the midline to prevent evulsion of the presacral
veins on the lateral margin of the sacrum. These can be a source
of troublesome bleeding if lacerated. |
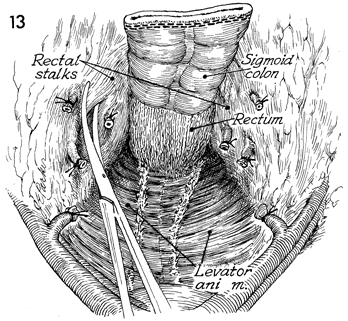
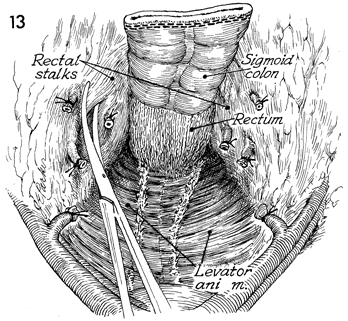
The stalks of each side of the rectum are
progressively clamped, incised, and tied with 2-0 suture. This
frees the rectum from its lateral attachments. |
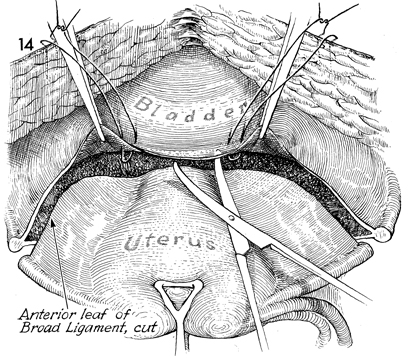
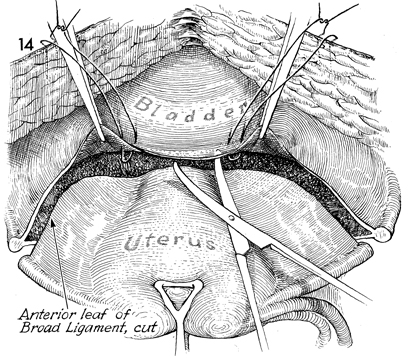
The anterior leaf of the broad ligament is
incised down and across the bladder peritoneum. The vesicoperitoneum
is elevated and sutured to the skin for retraction, and the bladder
is dissected off the lower uterine cervix and anterior vagina
for a distance of at least 6-8 cm below the tumor level. |
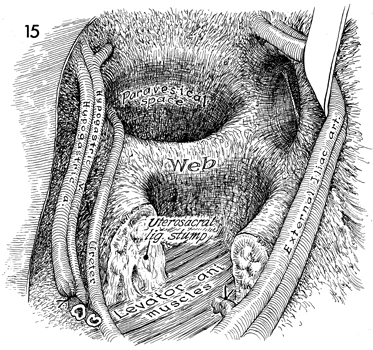
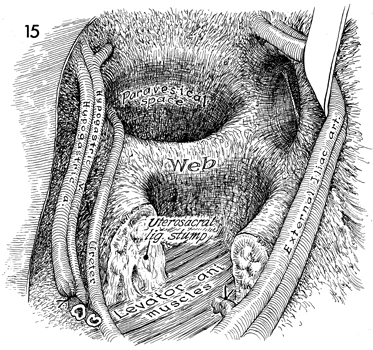
The uterus is retracted medially. The paravesical
and pararectal spaces are dissected. Notice that in taking down
the rectal stalks the posterior wall of the pararectal space
has been removed. The ureter crosses the superior medial portion
of the web as it enters the tunnel. The hypogastric artery and
vein have been retracted medially. The external iliac artery
and vein have been retracted laterally, revealing the obturator
fossa and nerve. |
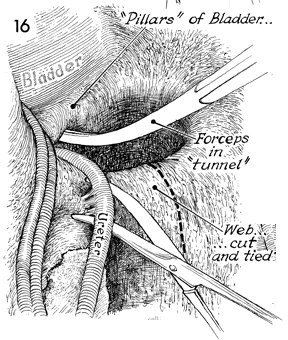
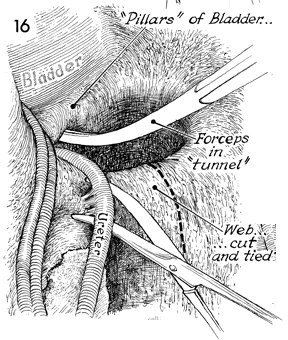
The dissection of the ureter is carried down
to the web by delicately elevating the ureter with a vein retractor.
The attachments of the ureter to the web are lysed with Metzenbaum
scissors. A Kelly clamp is inserted on top of the ureter underneath
the tunnel toward the bladder. The dotted line indicates
the incision to be made in the web adjacent to the pelvic wall. |
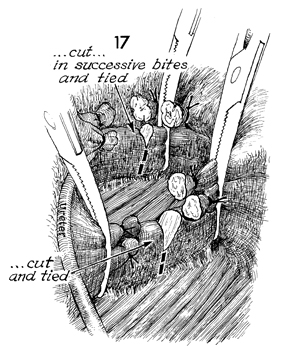
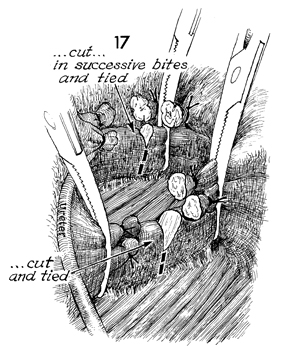
The tunnel is taken down in successive bites
and tied with 3-0 synthetic absorbable suture. When the tunnel
has been completely transected, the course of the ureter can
be seen all the way to the ureterosacral junction. The web is
taken down in successive bites and tied with 0 suture all the
way to the levator muscle. |
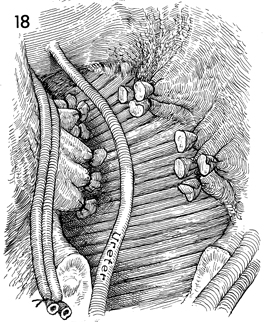
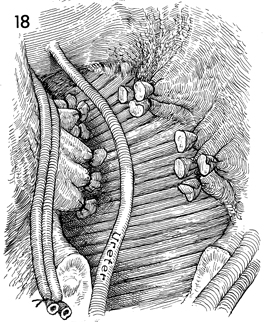
The specimen is free of lateral attachments
to the pelvic wall and, posteriorly, from the sacrum. The specimen,
consisting of the uterus, its lateral attachments, rectum, and
the ureterosacral and rectal stalk ligaments along with the hypogastric
artery, vein, and its branches, can be elevated. The ureter is
freed all the way to the bladder. |
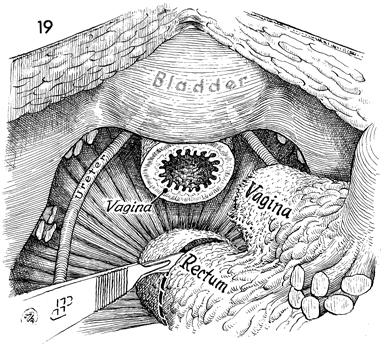
By firm cephalad traction on
the specimen, the vagina has been transected with a scalpel at
the level of the levator muscle. The rectum is transected below
the tumor but preferably above the levator sling. |
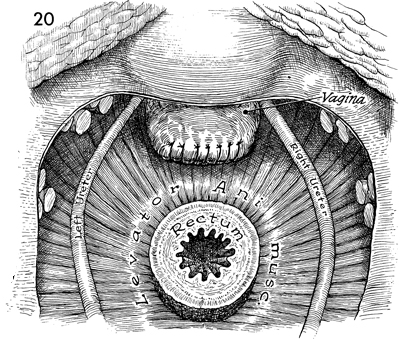
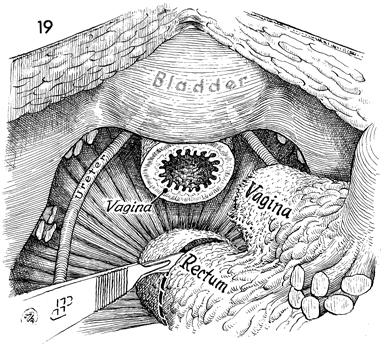
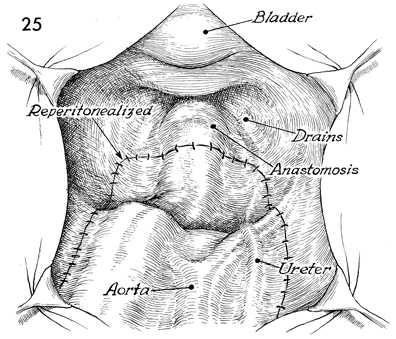
The completed operative field, the stumps
of the various lateral attachments of the uterus and rectum,
the dissected ureters, and the intact bladder are shown. The
vaginal cuff is reefed with a 0 suture and left open. The rectum
is available for reanastomosis of the descending colon. |
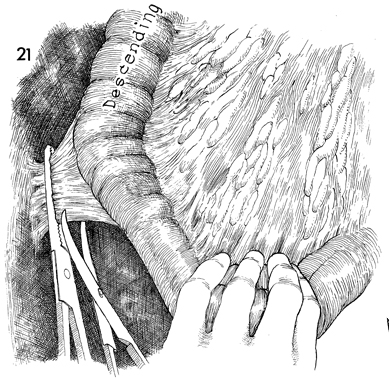
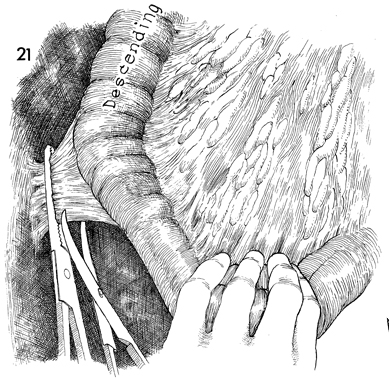
The descending colon is mobilized. The splenocolic
ligament is clamped and tied. The peritoneum lateral to the descending
colon is opened along the line of Toldt to the pelvic brim. |
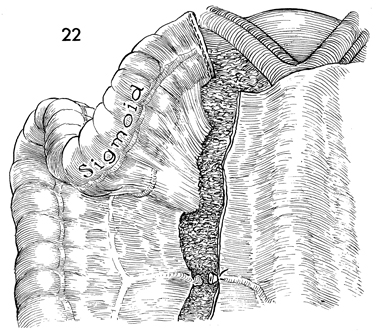
The surgeon mobilizes the rectosigmoid and
descending colon further by transecting the left colic branch
of the inferior mesenteric artery. An attempt should be made
to preserve as many of the branches of the inferior mesenteric
artery as possible to give maximum blood supply to the descending
colon at its anastomosis with the rectum. If the marginal artery
of the colon is intact, however, the inferior mesenteric artery
itself may be clamped and tied at the aorta to produce complete
mobility of the colon. There must be no tension on the J pouch
colorectal anastomosis. The marginal artery of the colon allows
sacrifice of the superior hemorrhoidal and left colic branches
of the inferior mesenteric artery if needed to achieve a tension-free
anastomosis. |
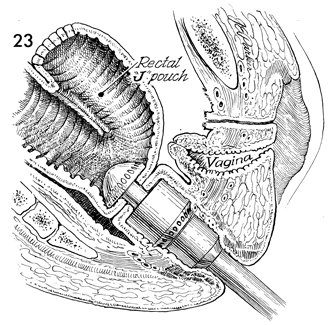
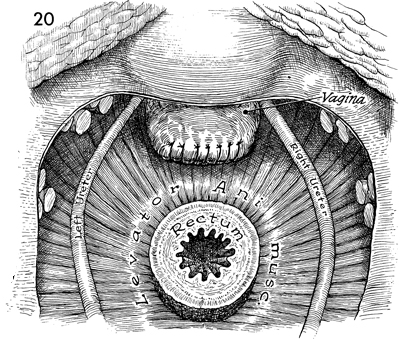
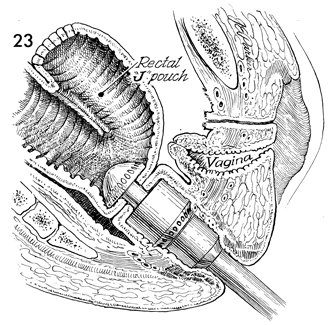
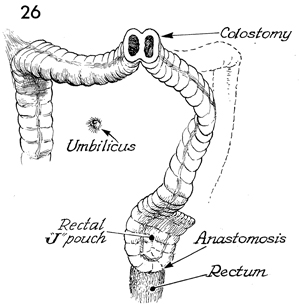
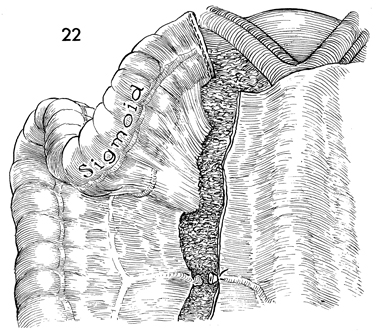
A rectal reservoir colonic J pouch has been
constructed. The opening in the inferior portion of the J pouch
is stapled to the rectal stump with the automatic surgical stapler
(EEA stapler) inserted through the anus and activated. |
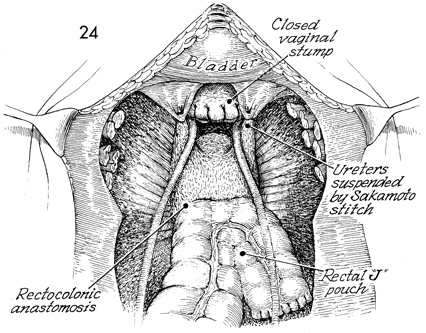
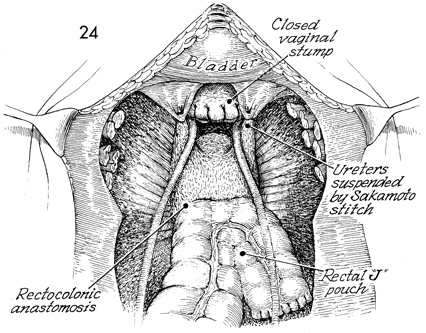
The descending colon has been formed into
a rectal J pouch colonic reservoir and stapled to the rectum.
The vaginal cuff has been closed. The ureters have been suspended
with the Sakamoto stitch. |
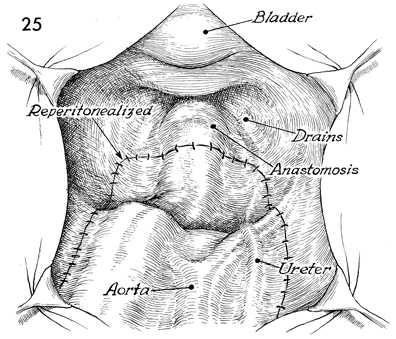
Maximum peritonealization has been achieved. |
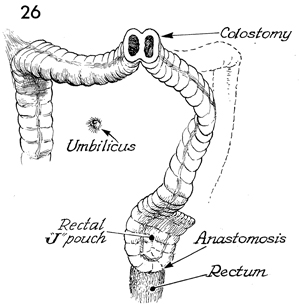
In all radiated cases, and in any case in
which there is some doubt about the healing properties of the
anastomosis, a protective temporary diverting loop colostomy
should be performed. This may be closed in 2-3 months, after
the rectal J pouch colonic reservoir has healed. |
|