Malignant
Disease:
Special Procedures
Staging
of Gynecologic
Oncology Patients With
Exploratory Laparotomy
Subclavian Port-A-Cath
Peritoneal Port-A-Cath
Application
of Vaginal
Cylinders for Intracavitary
Radiation Therapy
Application
of Uterine Afterloading Applicators
for Intracavitary Radiation Therapy
Pelvic High-Dose
Afterloader
Abdominal
Injection of Chromic Phosphate
( ) )
Supracolic
Total Omentectomy
Omental Pedicle "J"
Flap
Tube Gastrostomy
Total Vaginectomy
Radical
Vulvectomy
With Bilateral Inguinal
Lymph Node Dissection
Reconstruction
of the
Vulva With Gracilis Myocutaneous Flaps
Transverse
Rectus
Abdominis Myocutaneous
Flap and Vertical Rectus
Abdominis Myocutaneous
Flap
Radical
Wertheim
Hysterectomy With
Bilateral Pelvic Lymph
Node Dissection and With Extension of the Vagina
Anterior Exenteration
Posterior Exenteration
Total Pelvic
Exenteration
Colonic
"J" Pouch Rectal
Reservoir
Kock Pouch
Continent Urostomy
Omental "J" Flap
Neovagina
Ileocolic
Continent Urostomy (Miami Pouch)
Construction
of Neoanus
Gracilis Dynamic Anal
Myoplasty
Skin-Stretching
System Versus Skin Grafting
Gastric
Pelvic Flap for
Augmentation of Continent Urostomy or Neovagina
Control
of Hemorrhage in Gynecologic Surgery
Repair
of the Punctured
Vena Cava
Ligation
of a Lacerated
Internal Iliac Vein and
Suturing of a Lacerated Common Iliac Artery
Hemorrhage
Control in
Sacrospinous Ligament
Suspension of the Vagina
Presacral
Space
Hemorrhage Control
What
Not to Do in Case of Pelvic Hemorrhage
Packing
for Hemorrhage
Control
Control
of Hemorrhage
Associated With Abdominal Pregnancy |
Radical
Wertheim Hysterectomy With Bilateral Pelvic Lymph
Node Dissection and With Extension of the Vagina
Radical Wertheim hysterectomy is performed predominantly for stage
IB and early stage IIA carcinoma of the cervix and for stage I carcinoma
of the vagina. It is also appropriate for stage II adenocarcinoma of
the endometrium (corpus excervicus). The operation essentially includes
removal of the uterus, upper vagina, and all the parametrial tissues
to the pelvic side wall. The ureter and bladder are dissected free
and left intact. Reconstruction of the vagina, if necessary, can be
achieved by the technique of extension of the vagina, making a pocket
out of the vesical peritoneum and the rectal serosa.
Physiologic Changes. Carcinoma of the vagina, cervix,
and uterus is removed.
Points of Caution. The major complications
of the radical Wertheim hysterectomy are vesicovaginal and ureterovaginal
fistulae in approximately 1.5% of patients.
Hemorrhage can be a problem.
The danger areas from hemorrhage are the hypogastric vein and its tributaries
(internal iliac vein), the vessels in the obturator fossa, and nuisance
bleeding from the small vessels located in the tunnel of the ureter.
Postoperative urinary retention
with bladder atony is a permanent problem in less than 10% of patients.
It comes from the transection of (1) the sympathetic nerves to the
bladder in the upper portion of the web and (2) the ureterosacral ligaments.
Technique
RADICAL WERTHEIM HYSTERECTOMY
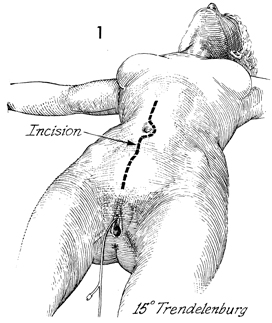
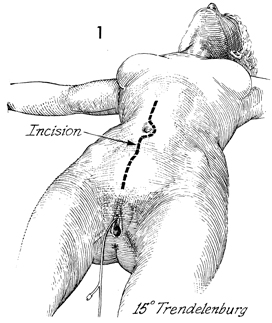
The patient is placed in the modified dorsal
supine lithotomy position (15° Trendelenburg). The bladder is
emptied with a Foley catheter. A thorough bimanual examination
is always performed. The abdomen, perineum, and vagina are surgically
prepared.
An abdominal incision is made
in the midline and extended around the umbilicus. A Foley catheter
is left in the bladder and connected to straight drainage. |
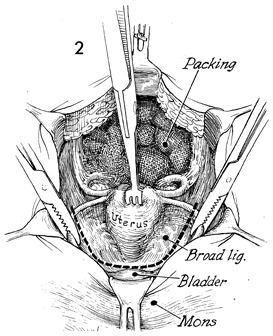
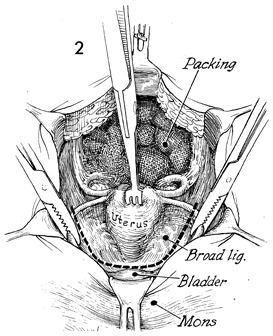
The abdomen is thoroughly explored. The peritoneum
between the cecum and terminal ileum is opened, the common iliac
and aortic area are exposed, and any suspicious lymph nodes are
removed for biopsy.
The intestine is packed off
in the upper abdomen.
A large thyroid clamp is placed on the uterine fundus and used as an elevator.
The round ligaments are clamped at both pelvic walls, incised, and tied. The
anterior leaf of the broad ligament is opened along with the vesicouterine peritoneal
fold. |
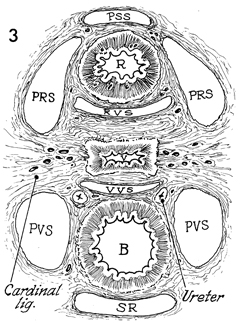
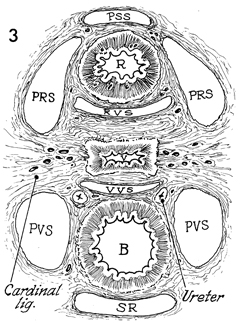
This view, which is cut through the pelvis
in the posterior-anterior plane, demonstrates the pelvic spaces
essential for all radical pelvic surgery.
In this view, the presacral
space (PSS) is at the top. Advancing anteriorly, the
surgeon finds the rectum (R) and the pararectal spaces (PRS). The
surgeon can enter this space by displacing the ureter and moving
between the ureter and internal iliac artery.
The rectovaginal
space (RVS) is the next space anterior to the rectum.
This area is entered by incising the peritoneum in the cul-de-sac
of Douglas and dissecting the posterior vaginal wall from the perirectal
fascia covering the rectum. The next space is the vagina (V).
After
the vagina comes the vesicovaginal space (VVS).
This is entered by retracting the bladder (B) anteriorly
and dissecting this space with sharp dissection along the pubovesical
cervical fascia. Note the position of the ureter and its relationship
to this space.
The next significant space is
the paravesical space (PVS). Between
the pararectal space and the paravesical space is the lateral extent
of the cardinal ligament, originally described as the "web" by
Wertheim. The web contains the venous network of the internal iliac
vein. The superior portion of the web contains the sympathetic
nerve fibers to the bladder along with the venous plexus. The inferior
portion of the web contains the parasympathetic nerve fibers to
the bladder.
In between the paravesical space is the bladder. Anterior to the
bladder is the space of Retzius (SR), the retropubic space.
Prior
to performing a radical Wertheim hysterectomy, the surgeon must
completely dissect the paravesical and pararectal spaces. |
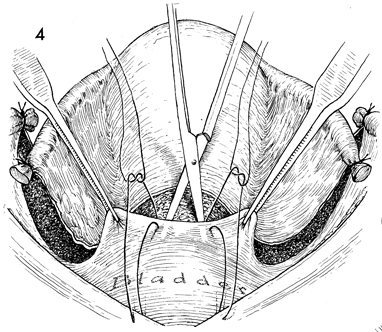
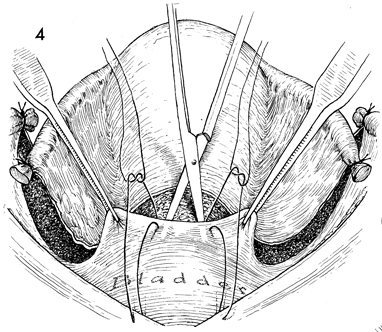
The round ligaments have been
cut and divided. The anterior leaves of the broad ligament have
been opened, and the vesicouterine peritoneum has been transected.
The vesical peritoneum is grasped with two forceps and elevated.
Scissors are used to dissect the vesicovaginal space between
the bladder and the anterior vaginal wall. Elevation of the bladder
can be facilitated by the placement of two sutures through the
vesicoperitoneum to the skin incision above the symphysis pubis. |
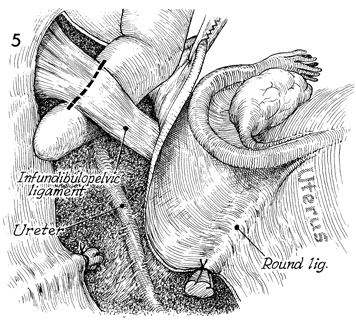
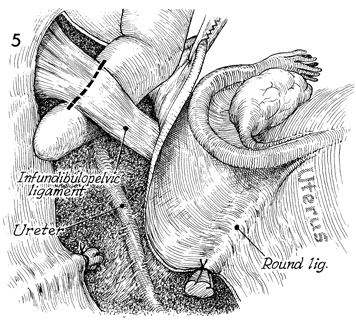
The posterior leaf of the broad ligament
is opened, exposing the infundibulopelvic ligament in the area
of the pelvic brim. A finger is inserted under the infundibulopelvic
ligament. The ureter is identified and dissected free of the
infundibulopelvic ligament. Three clamps are applied to the infundibulopelvic
ligament, and it is transected and doubly tied. The same procedure
is carried out on the opposite side. |
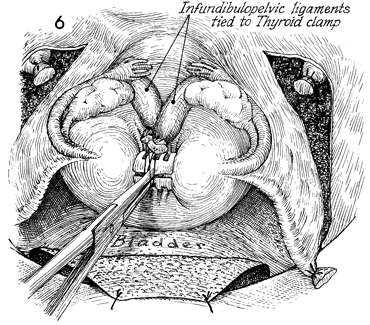
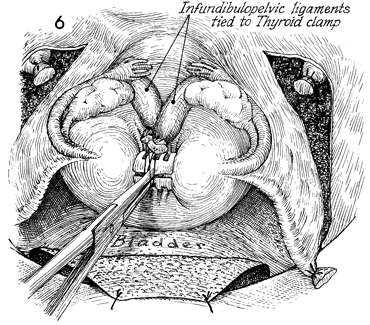
The infundibulopelvic ligament,
tubes, ovaries, and round ligaments are all tied to the thyroid
clamp placed on the middle of the fundus. The surgical field
is kept free of excessive instruments. |
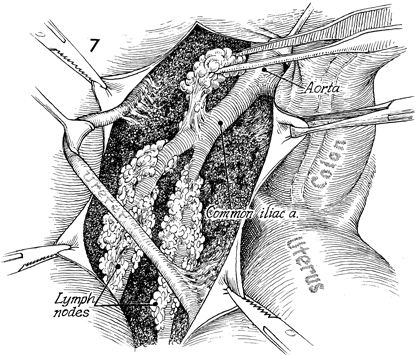
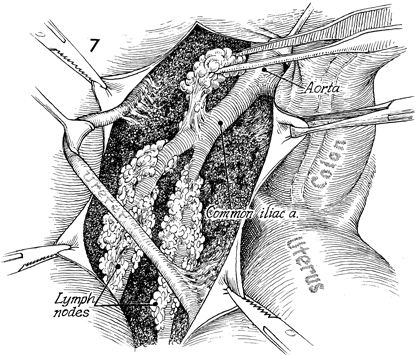
The uterus is retracted caudad and medially.
The base of the aorta is exposed, and the lymphatic tissue surrounding
the common iliac artery and vein is removed with sharp dissection.
The ureter is identified, dissected free of the artery, and retracted
laterally. All lymphatic tissue surrounding the external iliac
and common iliac blood vessels is removed from the bifurcation
of the aorta to the inguinal ligament at the femoral canal.
The lymph nodes are carefully
isolated in individual specimen containers for precise pathologic
analysis. |
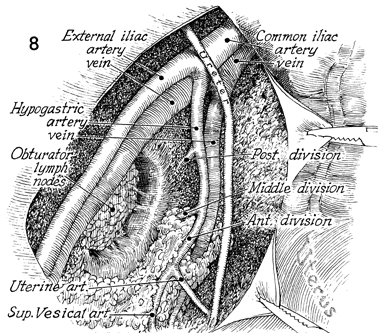
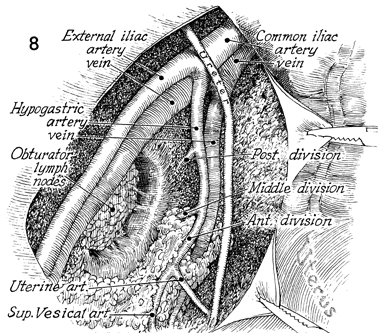
The common iliac, external iliac and upper
hypogastric vessels have been stripped of all lymphatic-bearing
tissue. The obturator fossa and the lower branches of the hypogastric
artery remain to be dissected. |
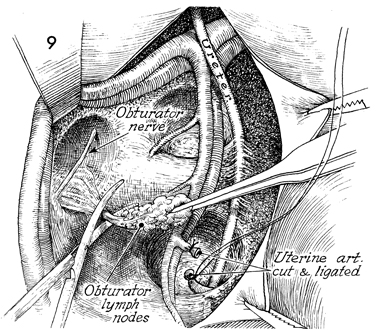
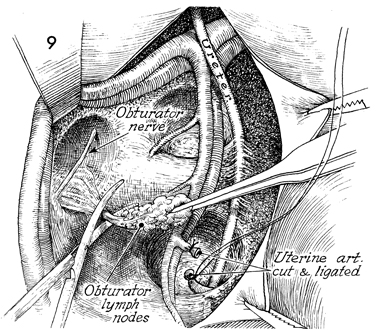
A vein retractor is
used to retract the external iliac artery and vein laterally,
and all lymphatic tissue is removed from behind these vessels
and from the obturator fossa. The obturator nerve is preserved.
Vessels deep in the obturator fossa may be ligated with hemoclips.
The uterine artery is identified as it comes off the anterior
division of the hypogastric artery before it enters the tunnel.
It is transected and tied with 2-0 suture.
The same procedure is carried out
on the left side. |
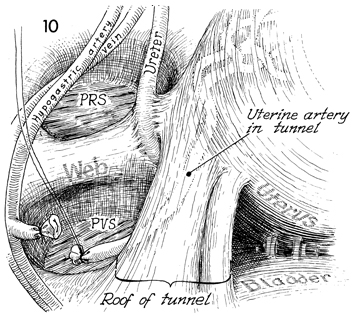
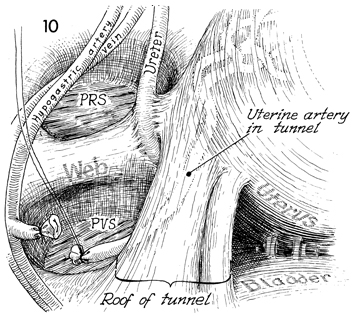
The pararectal space (PRS) and the
paravesical space (PVS) are shown with the intervening
web, which is the lateral extent of the cardinal ligament. The
uterine artery on both sides has been transected and deviated
medially. The distal stump of the uterine artery is seen as it
enters the tunnel. Its relationship to the ureter within the
tunnel is ghosted in this view. The ureter is seen as it enters
the tunnel. |
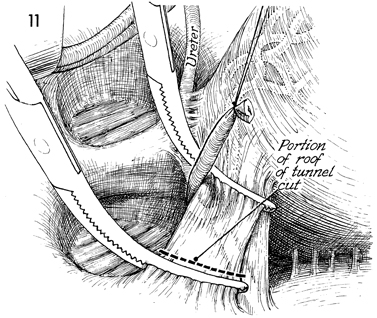
The relationship of the ureter to the uterine
artery is shown in the tunnel. The uterine artery has been transected
as it branches from the anterior division of the hypogastric
artery. It enters the tunnel laterally and crosses the ureter.
Two horizontal curved clamps are inserted on top of the ureter
beneath the roof of the tunnel to include the uterine artery
and vein. The tissue in the roof of the tunnel, consisting of
the uterine artery and vein, is clamped, incised, and tied. In
some patients, this may be performed in one step; in others,
two to three successive bites with horizontal curved clamps on
the roof of the tunnel are needed. |
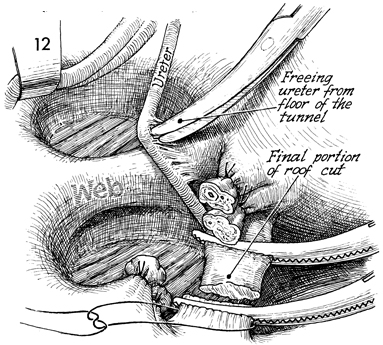
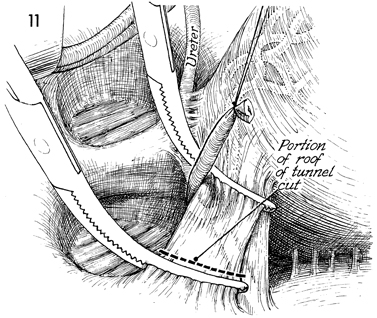
The ureter is elevated with a small retractor.
The filmy adhesions between the ureter and the floor of the tunnel
connecting the ureter to the superior portion of the web are
gently lysed and dissected laterally. The pararectal and the
paravesical spaces, with the web in between, are visualized.
The hypogastric artery and vein, along with the external iliac
artery and vein, are retracted laterally. Note that in this particular
patient the roof of the tunnel has been taken down in three successive
bites between the horizontal curved clamps and been incised and
tied. |
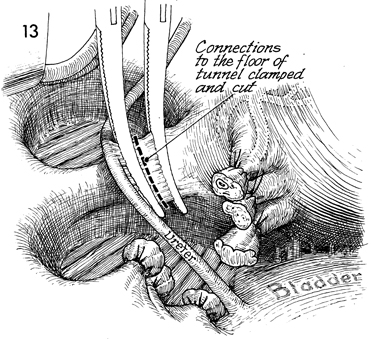
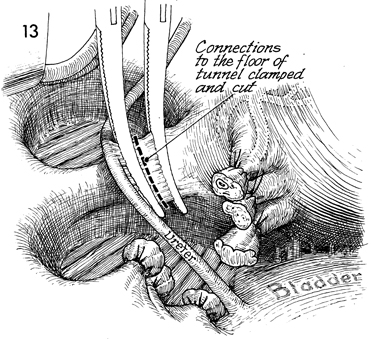
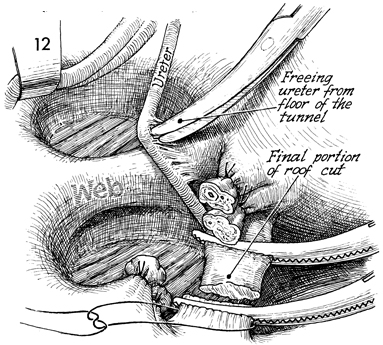
The external iliac artery and vein and the
hypogastric artery and vein are retracted medially. The pararectal
and the paravesical spaces are exposed. After the ureter has
been dissected laterally (Fig. 12), the floor of the tunnel can
be visualized. Two horizontal curved clamps are placed across
the floor of the tunnel and excised. This completely frees the
ureter from any attachment to the web. |
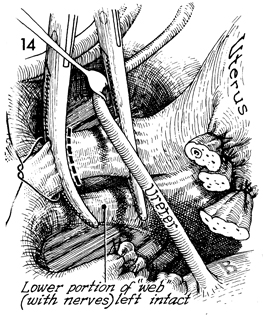
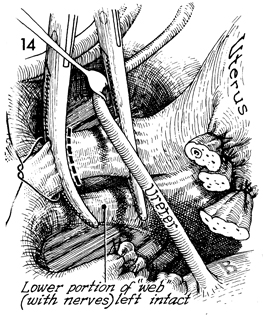
The uterus and the stumps of the tunnel, roof, and floor are
seen on the right. The ureter is retracted laterally with a vein
retractor.
Both portions of the web are noted. The superior
portion of the web, containing the hypogastric venous plexus
and sympathetic nerves to the bladder, is separated from the
lower portion containing the parasympathetic nerves to the bladder.
In most cases, transection of only the upper portion is required
to achieve the goal of the radical Wertheim hysterectomy.
We prefer to place a straight vascular
clamp medial to the ureter on the medial portion of the web.
A curved clamp can be placed on the lateral portion of the web
at the pelvic wall. The superior portion of the web is transected
and tied. The lower portion is left intact. |
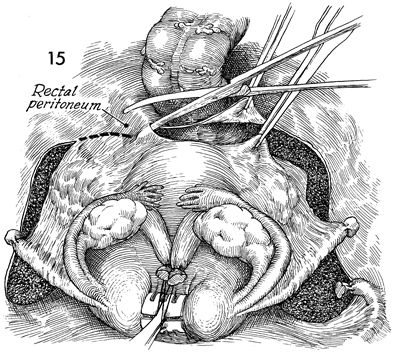
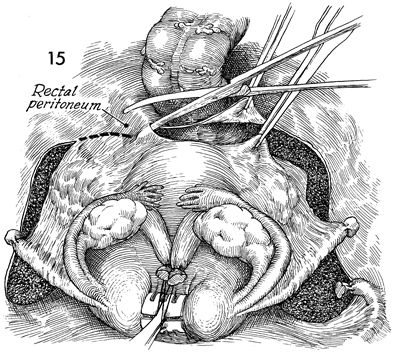
The uterus is retracted upward and caudad.
The incision in the posterior leaf of the broad ligament is extended
across the cul-de-sac and peritoneum overlying the cul-de-sac
between the cervix and rectum. |
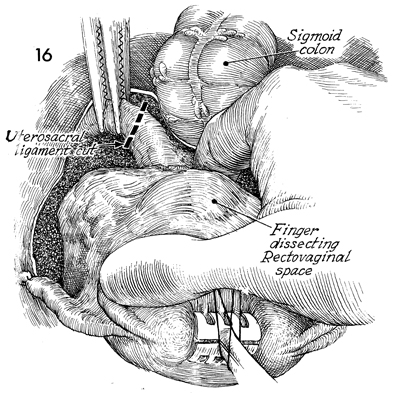
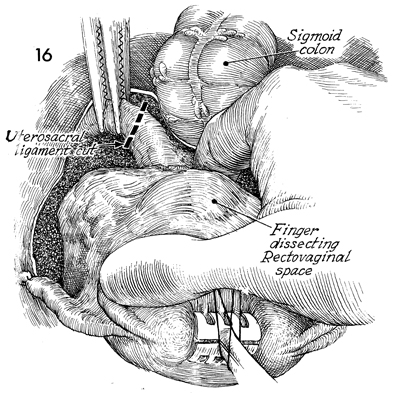
The uterus is retracted cephalad, a finger
is inserted between the uterosacral ligaments, and the posterior
wall of the vagina is dissected off the anterior rectal wall.
Retraction on the uterus is changed to the anterior caudad position,
placing the uterosacral ligaments on tension. The upper portion
of the uterosacral ligaments is clamped, incised, and tied. The
lower portion of the uterosacral ligaments, containing the parasympathetic
nerves to the bladder, is left. |
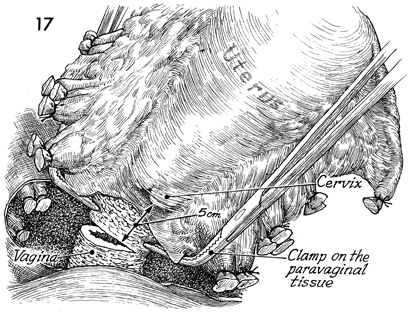
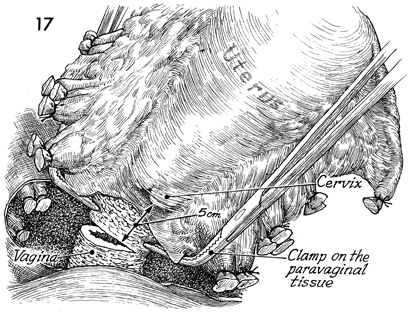
The lateral, posterior, and
anterior attachments of the uterus and its parametria have all
been transected and tied. Two right-angle Heaney clamps are placed
on the paravaginal tissue on each side, and a scalpel is used
to transect the remaining paravaginal tissue and vagina between
these clamps. The paravaginal tissue pedicle is tied with a 0
synthetic absorbable suture.Approximately 5 cm of vagina
should be removed. |
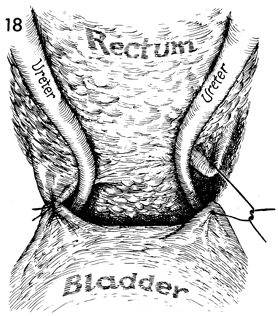
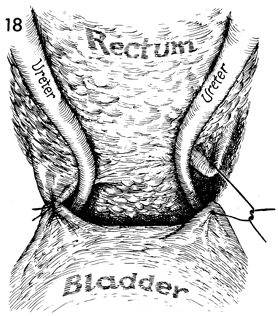
The Sakamoto sling suspends the ureters medially,
out of the dissected pararectal and paravesical spaces. Several
0 synthetic absorbable sutures are used for this maneuver, which
prevents the ureter from forming adhesions deep in the lateral
pelvic wall spaces. |
EXTENSION OF THE VAGINA
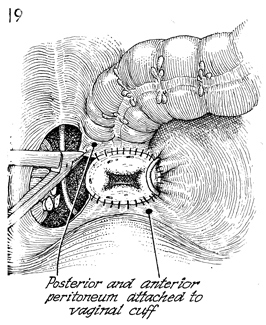
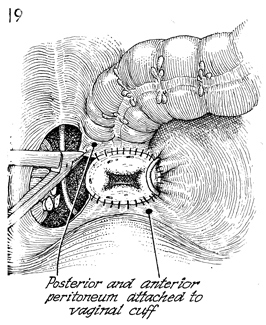
This view shows, on the patient's
left, the Sakamoto sling shown in Figure 18. If in younger patients
following radical Wertheim hysterectomy in which 4-5 cm of upper
vagina were excised a longer vagina is desired, the following
steps can be performed. The vesical peritoneum coming off the
bladder can be sutured to the anterior vaginal cuff. The serosa
from the rectosigmoid colon can be sutured to the posterior vaginal
cuff. |
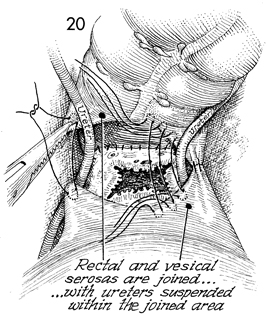
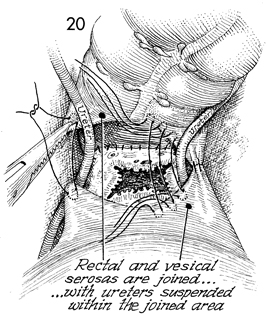
On the patient's right, the
Sakamoto sling is completed from the serosa of the rectum to
the vesical peritoneum. Synthetic absorbable sutures are being
placed in a row in the serosa of the rectum 5 cm from the posterior
vaginal cuff to a site chosen on the vesical peritoneum 5 cm
from the anterior vaginal cuff. When this row of sutures is completed,
there will be an extension of the vagina from the vaginal cuff
up to the new apex of the vagina that initially will be lined
by mesothelium. After several months, this mesothelium will undergo
squamous metaplasia, and the upper vaginal extension will be
similar to the traditional vagina. |
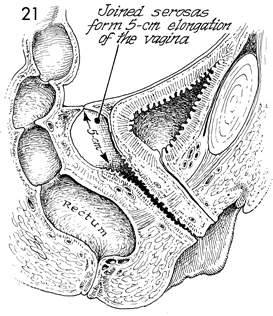
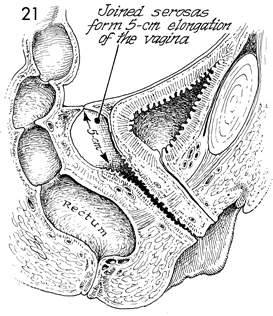
This sagittal view shows the 5-cm extension
to the vagina lined initially by mesothelium from the vesical
peritoneum and the serosa of the colon. We insert a soft foam
rubber form covered with condoms to keep this extension open
for 6 weeks following Wertheim hysterectomy. Sexual intercourse
is allowed after the form has been removed in 6 weeks. |
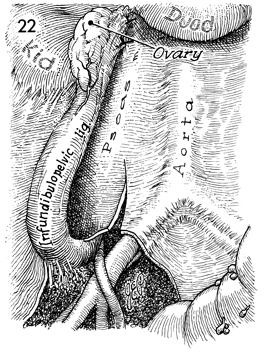
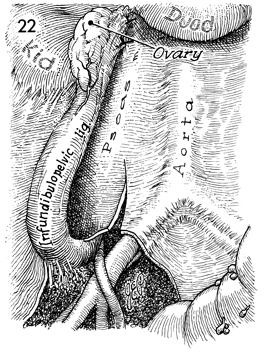
In young women, one or both
ovaries can be preserved by dissecting out the infundibulopelvic
ligament with its ovarian artery and vein and suspending the
ovary to the psoas muscle high in the abdomen under the inferior
pole of the kidney. This removes the ovary from any potential
field of radiation that may be utilized postoperatively. |
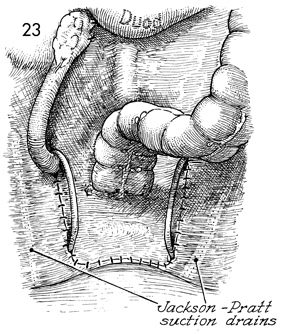
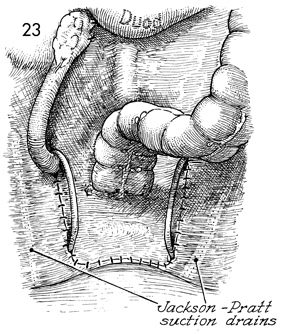
The third portion of the duodenum is seen
at the top. The ovary is suspended under the inferior pole of
the right kidney to the psoas muscle by several interrupted absorbable
sutures. The pelvic peritoneum has been closed with interrupted
absorbable sutures. Note that Silastic Jackson-Pratt closed suction
drains are inserted into the paravesical and pararectal spaces
on each side. These are brought retroperitoneally to the anterior
abdominal wall. |
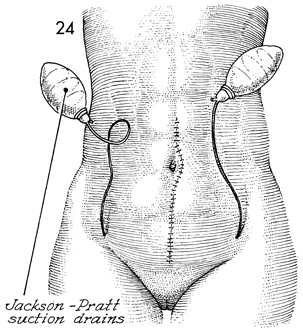
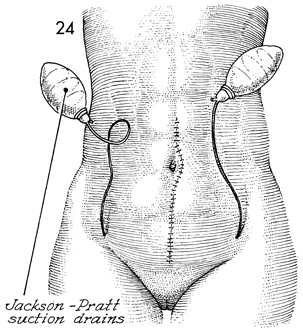
The Silastic closed suction
drains are brought out, respectively, through the right and left
lower quadrants of the abdominal wall. The midline incision,
extended around the umbilicus, is closed in layers. |
|