Malignant
Disease:
Special Procedures
Staging
of Gynecologic
Oncology Patients With
Exploratory Laparotomy
Subclavian Port-A-Cath
Peritoneal Port-A-Cath
Application
of Vaginal
Cylinders for Intracavitary
Radiation Therapy
Application
of Uterine Afterloading Applicators
for Intracavitary Radiation Therapy
Pelvic High-Dose
Afterloader
Abdominal
Injection of Chromic Phosphate
( ) )
Supracolic
Total Omentectomy
Omental Pedicle "J"
Flap
Tube Gastrostomy
Total Vaginectomy
Radical
Vulvectomy
With Bilateral Inguinal
Lymph Node Dissection
Reconstruction
of the
Vulva With Gracilis Myocutaneous Flaps
Transverse
Rectus
Abdominis Myocutaneous
Flap and Vertical Rectus
Abdominis Myocutaneous
Flap
Radical
Wertheim
Hysterectomy With
Bilateral Pelvic Lymph
Node Dissection and With Extension of the Vagina
Anterior Exenteration
Posterior Exenteration
Total Pelvic
Exenteration
Colonic
"J" Pouch Rectal
Reservoir
Kock Pouch
Continent Urostomy
Omental "J" Flap
Neovagina
Ileocolic
Continent Urostomy (Miami Pouch)
Construction
of Neoanus
Gracilis Dynamic Anal
Myoplasty
Skin-Stretching
System Versus Skin Grafting
Gastric
Pelvic Flap for
Augmentation of Continent Urostomy or Neovagina
Control
of Hemorrhage in Gynecologic Surgery
Repair
of the Punctured
Vena Cava
Ligation
of a Lacerated
Internal Iliac Vein and
Suturing of a Lacerated Common Iliac Artery
Hemorrhage
Control in
Sacrospinous Ligament
Suspension of the Vagina
Presacral
Space
Hemorrhage Control
What
Not to Do in Case of Pelvic Hemorrhage
Packing
for Hemorrhage
Control
Control
of Hemorrhage
Associated With Abdominal Pregnancy |
Total Pelvic Exenteration
Total pelvic exenteration is indicated in those patients with carcinoma
of the cervix with recurrence after irradiation and in patients with
primary stage IV disease in which tumor has advanced into the bladder
and rectum but remains confined to the pelvis.
Total pelvic exenteration is indicated and performed more often than
anterior or posterior exenteration. Thorough preoperative evaluation,
correction of anemia and nutrition, and a thorough mechanical and antibiotic
preparation of the intestines are prerequisites to surgery.
Recently,
the EEA (end-to-end anastomosis) automatic surgical stapler has made
it possible to leave many of these patients without permanent colostomies.
For carcinoma of the cervix or vagina to invade the lower 5 cm of the
rectum and anus is rare; therefore, it is possible to leave the anus
and lower rectum in many patients without reducing their chance for
cure. The descending colon can be mobilized, brought deep into the
pelvis, formed into a "J" pouch colonic reservoir, and stapled to the
rectum. This has had a significant psychologic benefit for the cancer
patient who would otherwise require two permanent abdominal stomas.
The
urine can be diverted into a continent urostomy. Therefore, external
appliances (bags) in most patients can be eliminated. Neovagina construction
can be made for those who desire it.
The purpose of the operation is
to remove all cancer tissue from the pelvis and to construct an appropriate
diversion for the urine and stool if the colon cannot be reanastomosed
to the rectum.
Physiologic Changes. The
most significant physiologic change associated with this operation
is the removal of all cancer tissue.
Diversion of the urine may result in significant physiologic
change. It may be associated with a higher incidence of renal disease
from urinary tract infection and obstruction. These complications are
less, however, than when the ureters are implanted into an intact sigmoid
colon or when the ureters are implanted into an ileal or colonic loop.
Points of Caution. Hemorrhage can be a major complication
of total pelvic exenteration. Bleeding will be decreased significantly
by early ligation of the internal iliac artery at the bifurcation of
the common iliac artery.
The ureters should be transected as low in
the pelvis as possible to give the surgeon maximum flexibility in performing
the continent urostomy. Reconstruction should start in the posterior
pelvis with the rectal J pouch coloproctostomy, proceed anteriorly
with the neovagina, and conclude with the Kock pouch continent urostomy.
This order of surgery is needed to prevent getting boxed in "from anatomic
exposure."
Postoperative care is of paramount importance and should
be performed in a surgical intensive care unit. Intravenous hyperalimentation
given preoperatively and postoperatively can improve the patient's
metabolic balance. The nutritional status of these patients can influence
wound healing.
Technique
The patient is placed on the operating table in the
modified dorsal lithotomy position with the legs abducted 30°. The
surgical preparation is carried from the breast over the mons pubis
to the tip of the coccyx. A Foley catheter is left in the bladder,
and urine output is monitored until the ureters are transected.
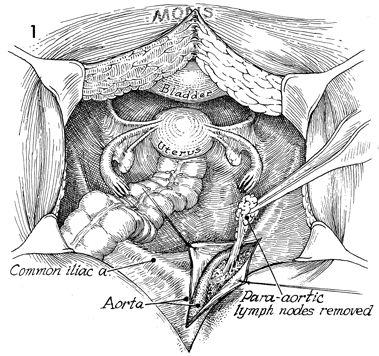
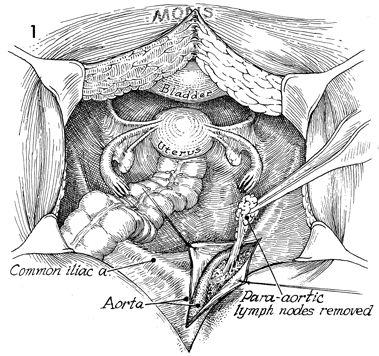
The abdomen is entered through a low midline
incision that is extended around the umbilicus. A thorough exploration
of the upper abdomen is made, particularly along the aorta and
common iliac arteries. The peritoneum below the terminal ileum
and cecum is opened. The right common iliac artery and vein are
identified. The incision into the peritoneum is extended along
the aorta until the renal vessels are located. Occasionally,
the third portion of the duodenum requires mobilization for exposure.
The aortic lymph nodes are palpated, and any suspicious lymph
node is removed for pathologic analysis. |
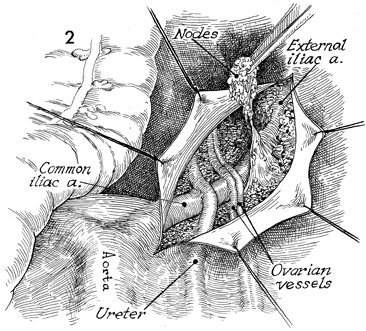
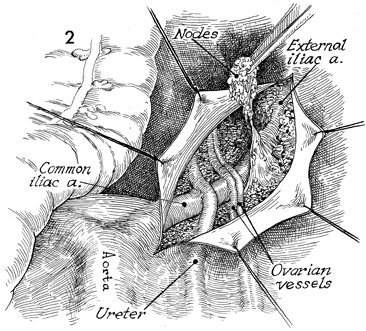
The peritoneal incision is extended caudad
along the external iliac vessels to the femoral canal. All lymphatic
tissue is dissected from the common and external iliac arteries
and veins. |
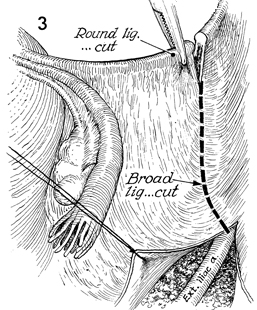
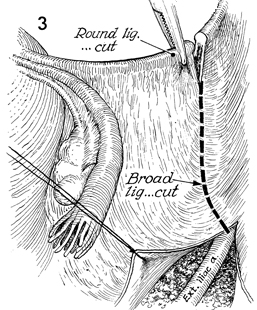
The round ligaments are cut
and tied at the pelvic wall, and the broad ligaments are opened. |
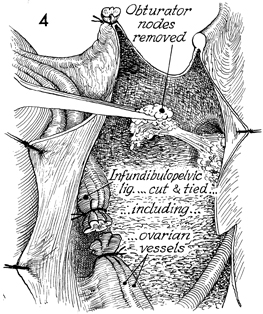
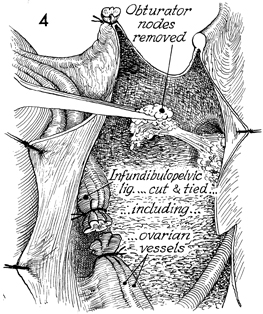
All lymphatic tissue is removed
from the obturator fossa. The infundibulopelvic ligaments with
the ovarian vessels are clamped, cut, and tied at the pelvic
brim. |
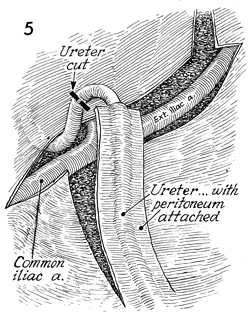
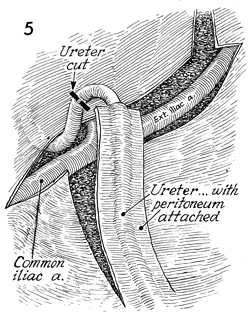
The right ureter is transected below the
pelvic brim. Steps 1-5 are then repeated on the left side. |
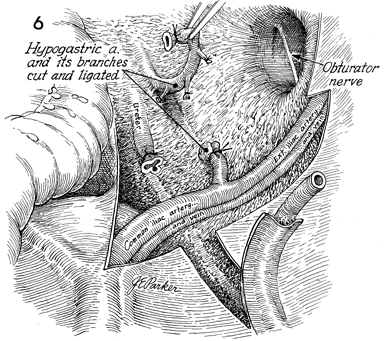
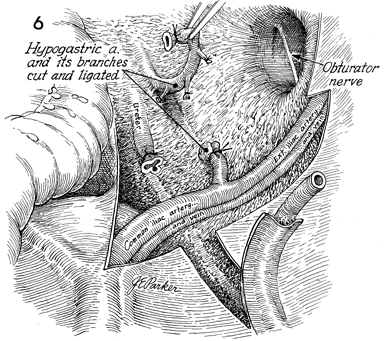
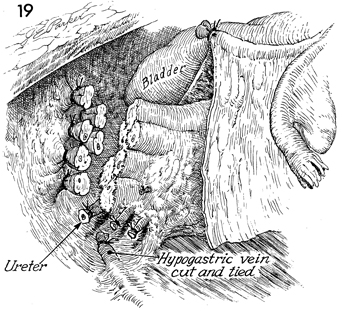
The obturator fossa external
iliac and common iliac artery and veins have been cleaned of
all lymphatic tissue. The hypogastric artery and vein are clamped
and tied at the bifurcation of the common iliac vessels. The
ureter has been cut, the distal segment has been tied, and the
proximal segment is left open and free. |
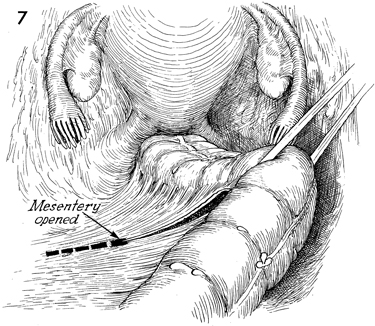
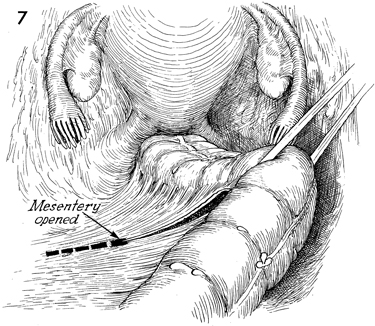
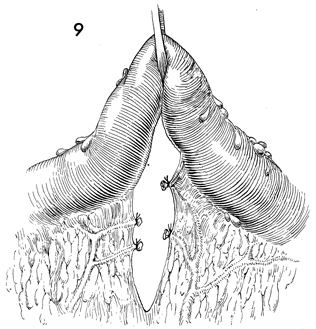
The peritoneum of the mesentery of the rectosigmoid
colon is opened. A soft Silastic drain is placed through an avascular
opening in the mesentery and used for retraction of the colon. |
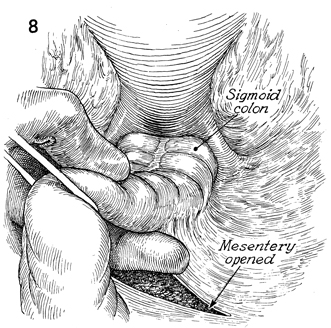
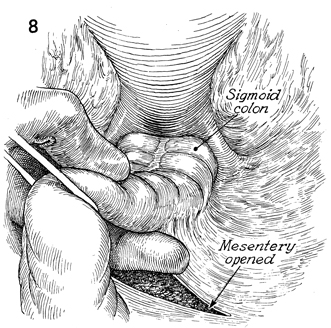
The peritoneum of the mesentery on the medial
side of the rectosigmoid colon is opened. |
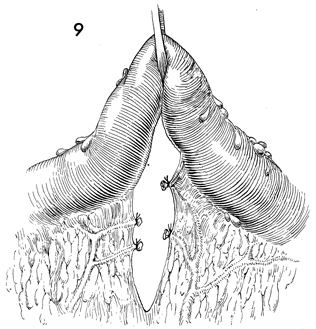
The vascular tissue in the mesentery is cross-clamped
in successive pedicles, incised, and tied with 2-0 suture. |
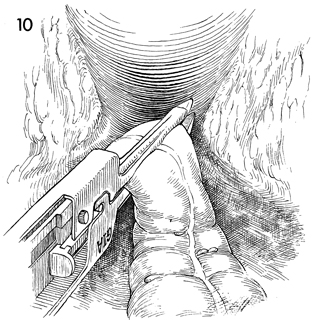
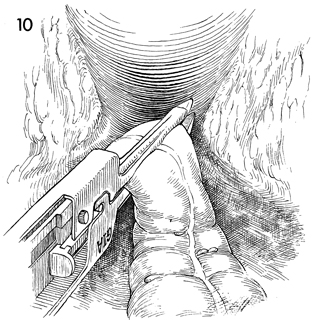
The rectosigmoid colon is clamped and transected
with the gastrointestinal anastomosis (GIA) automatic surgical
stapler. This transects the colon and seals the distal and proximal
segments. |
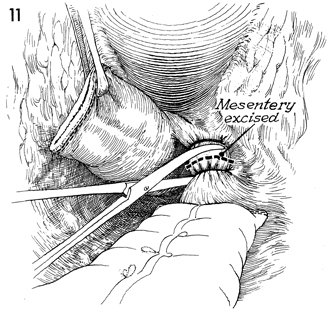
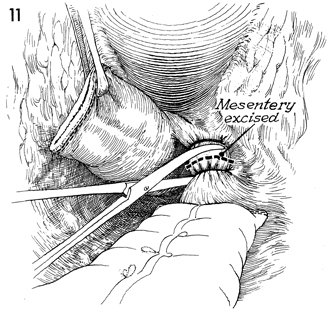
The remaining mesentery of the rectosigmoid
colon is clamped and incised down to the sacrum. |
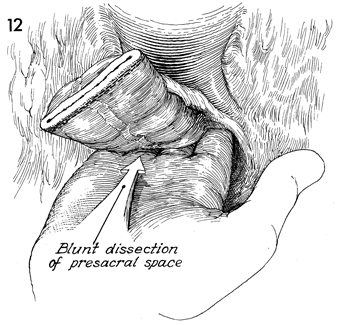
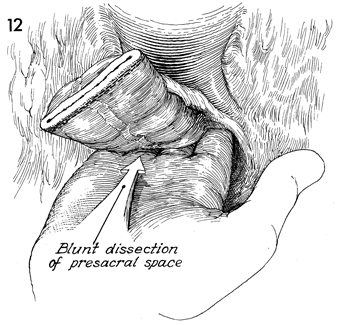
The rectum is dissected off the sacrum and
coccyx by blunt dissection. This is performed by retracting the
uterus and distal segment of the rectum anterior and cephalad,
inserting a hand behind the rectum in the presacral space, and
freeing the rectum down to the coccyx.
It is important to allow the
blunt dissection to proceed laterally, since the presacral veins
may then be lacerated and may retract in to the presacral foramen,
causing copious bleeding. |
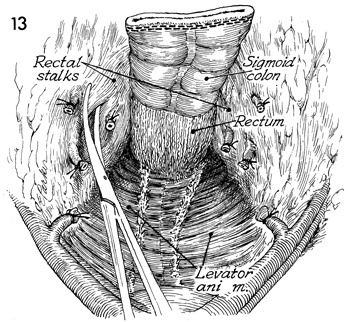
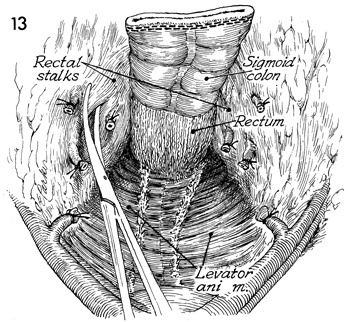
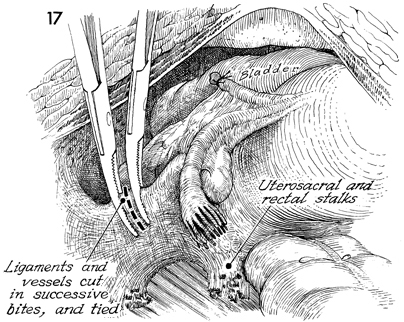
The rectal stalks on each side are clamped,
incised, and tied with 2-0 sutures down to the levator muscles.
The specimen should now be free
posteriorly. |
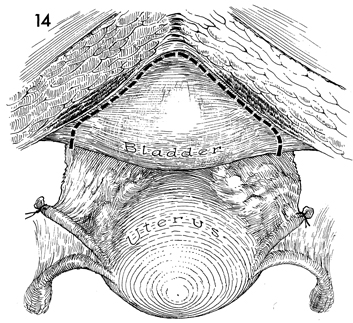
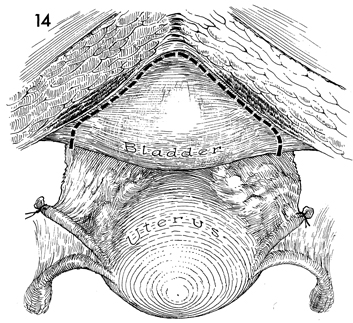
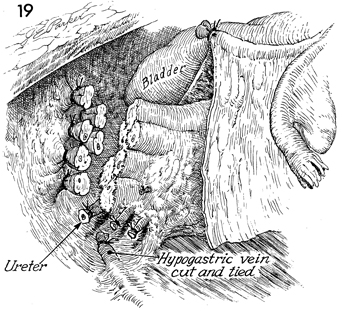
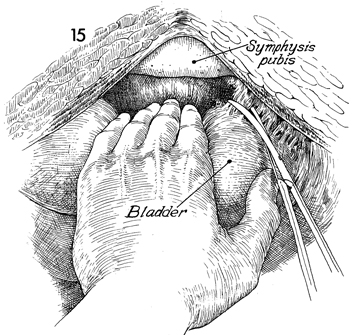
The bladder is separated from the pubic symphysis
where the dotted line appears. |
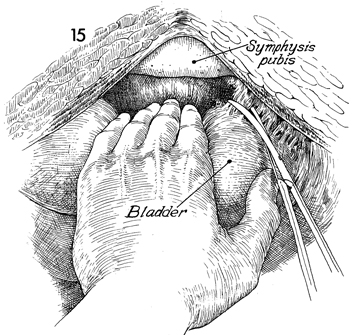
The space of Retzius is entered, and the
bladder and proximal two-thirds of the urethra are freed. The
lateral attachments of the bladder are clamped and incised on
both sides. The entire specimen can now be freed laterally, forming
one large lateral attachment of bladder, rectum, and uterine
parametria to the pelvic wall. |
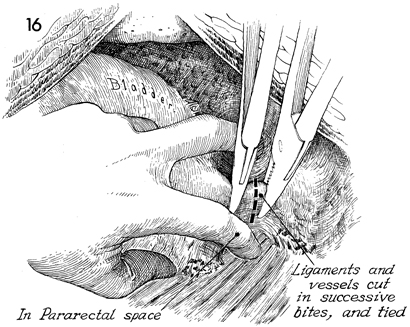
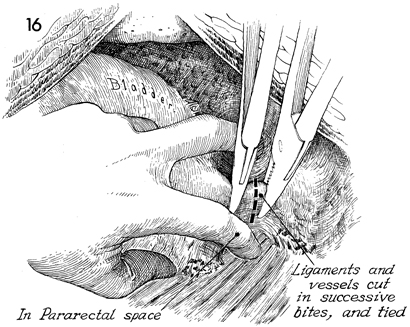
The first and second fingers have been inserted
into the paravesical and pararectal spaces, identifying both
sides of the large lateral attachment to the pelvic wall. The
anterior wall of the paravesical and the posterior wall of the
pararectal space have been removed with dissection of the rectal
stalks and bladder attachments. The large pedicle contains the
plexus of hypogastric veins. No attempt is made to isolate each
vein individually. The pedicle is clamped, incised, and tied
on the pelvic wall. Several successive bites are required to
transect the pedicle to the levator ani muscle. |
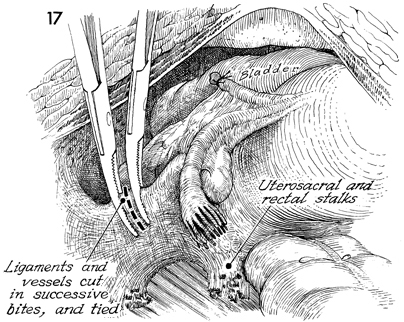
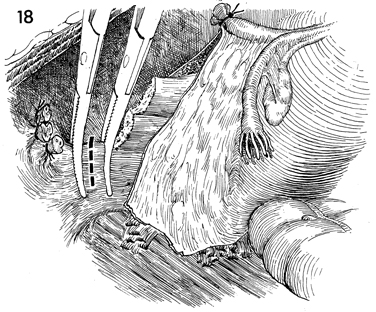
This is a posterior view of the same step
performed on the opposite side. |
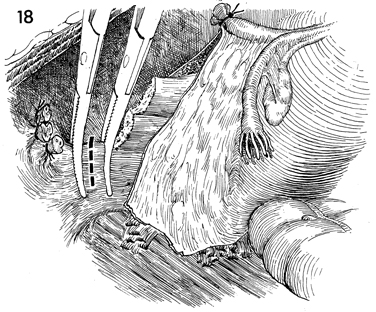
The lateral attachment of the specimen is
transected in successive bites. It is helpful for the assistant
to retract the specimen medially during this maneuver. |
All lateral wall attachments have been clamped,
incised, and ligated on each side. The specimen has been freed
posteriorly, laterally, and anteriorly. The remaining attachments
are the urethra, vagina, and rectum. |
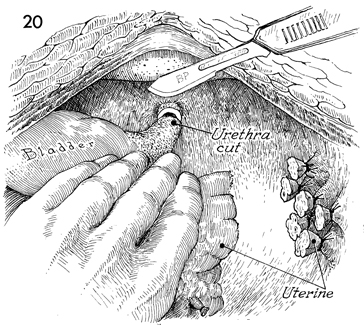
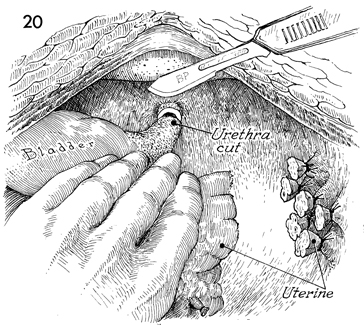
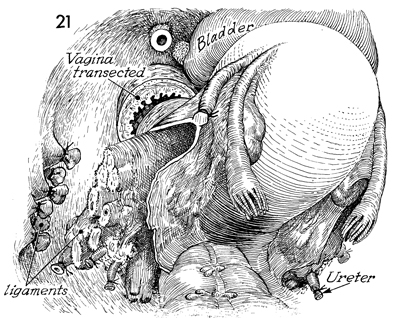
By cephalad retraction on the specimen, the
urethra can be exposed and transected at the level of the levator
sling. |
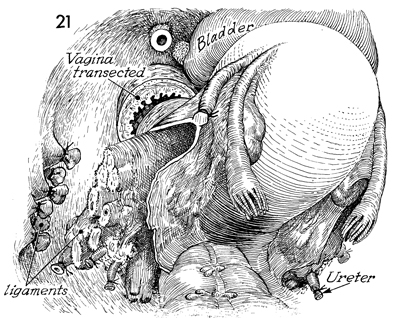
The vagina is transected. |
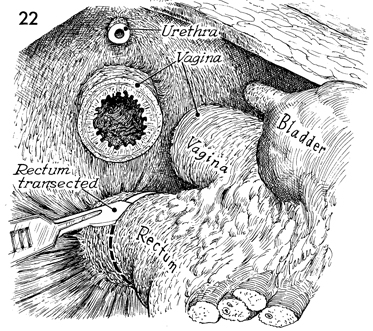
The rectum is transected at the level of
the levator muscles or higher if an adequate margin from the
tumor can be achieved. |
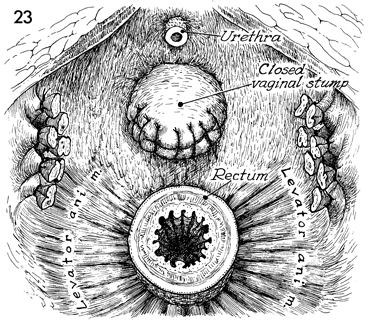
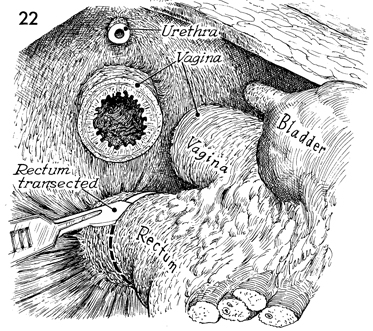
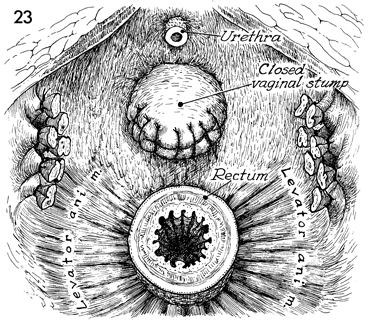
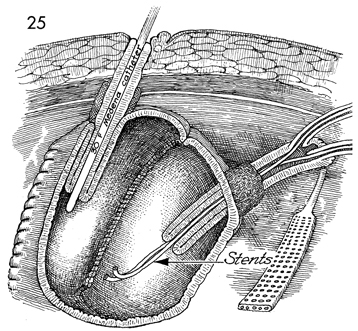
The exenterated pelvis is shown
with the urethra transected near its meatus. The vagina has been
transected and closed with 0 absorbable suture. The rectum is
available for anastomosis for the descending colonic J pouch.
A continent urostomy Kock pouch (see Kock Pouch Continent Urostomy)
will be constructed. |
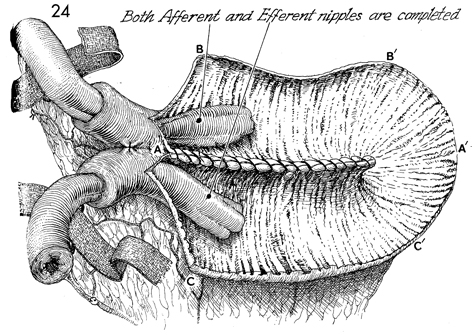
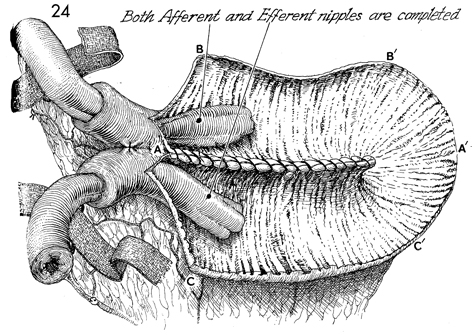
Both afferent and efferent nipples
have been completed. Note that the two strips of the polyglycolic
acid (PGA) mesh pass through the windows of Deaver in the mesentery
of both the efferent and afferent bowel limbs adjacent to the
nipples. The letters A to A', B to B',
C to C' delineate the order of suture placement
that will produce a spherical rather than tubular pouch shape. |
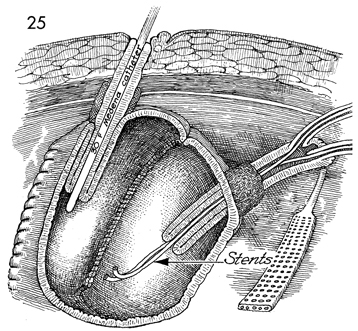
The continent pouch has been completed. The
stoma is sutured to the subcuticular layer of the skin with 3-0
PGA sutures. The stoma is sutured to the subcuticular skin of
the umbilicus with 3-0 PGA sutures. A No. 30 French Medena catheter
has been placed through the stoma down the efferent limb and
exits the efferent nipple into the pouch. This catheter has been
securely sutured in place with a No. 1 nylon suture that includes
the margin of the skin, the entire intestinal wall of the stoma,
the opposite intestinal wall, and the opposite margin of skin;
it is securely tied around the Medena catheter with multiple
half-hitch knots to hold the catheter in the pouch without spillage
for 3 weeks. A second No. 1 nylon suture is placed on the other
side.
A Jackson-Pratt closed suction
drain has been placed adjacent to the Kock pouch and brought
out through the abdominal wall. It is sutured with a 3-0 PGA
suture to prevent removal for 3 weeks. Note that the afferent
limb of bowel and the afferent nipple have the ureters sutured
in a mucosa-to-mucosa fashion with No. 8 French Finney "J" Silastic
stents in place. The abdomen is closed. The Medena catheter is
irrigated every 2-4 hours for the next 3 weeks to prevent mucus
obstruction. |
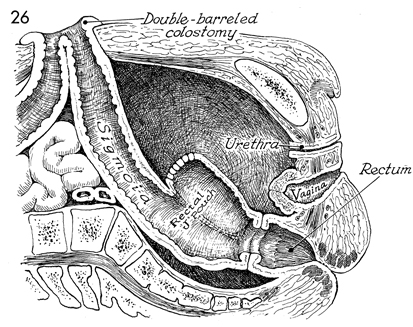
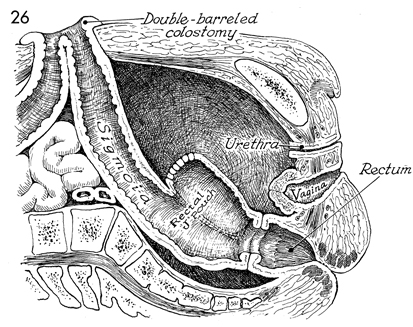
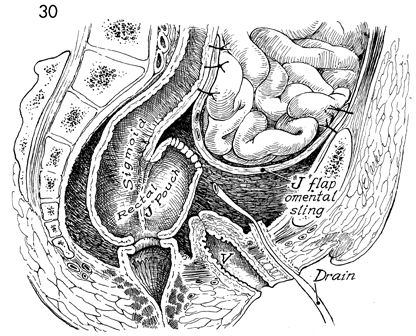
A sagittal view is shown. The rectal J pouch
has been stapled to the rectum with the EEA stapler. A diversionary
loop colostomy has been performed. |
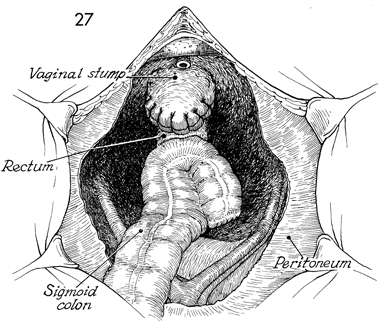
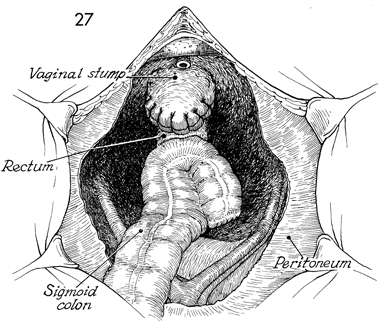
A pelvic view shows the rectal J pouch anastomosed
to the rectum. The vagina is shown closed with suture. |

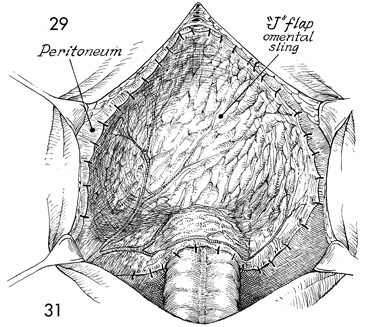
An omental J flap is initiated by transecting
the omentum off the greater curvature of the stomach. The gastroepiploic
artery is preserved. |
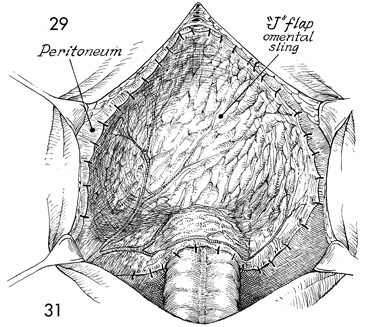
The omental J flap is sown into the pelvis
as a lid. |
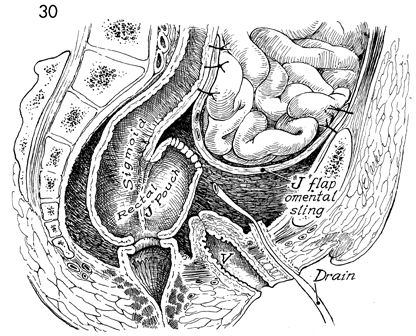
This sagittal view shows the omental J flap
as a lid for the pelvis. It contains the small intestine and
displaces it out of the pelvis in a sling made from omentum.
The colonic J pouch reservoir
is anastomosed to the rectum. V, vagina. |
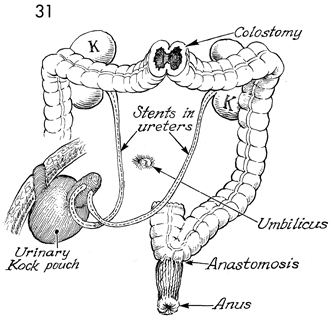
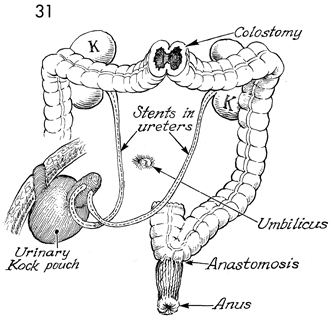
This shows the loop diversion colostomy placed
in the transverse colon. The urine has been diverted into a continent
Kock pouch. The colonic J pouch has been anastomosed to the rectum. K,
kidney. |
|
|