Malignant
Disease:
Special Procedures
Staging
of Gynecologic
Oncology Patients With
Exploratory Laparotomy
Subclavian Port-A-Cath
Peritoneal Port-A-Cath
Application
of Vaginal
Cylinders for Intracavitary
Radiation Therapy
Application
of Uterine Afterloading Applicators
for Intracavitary Radiation Therapy
Pelvic High-Dose
Afterloader
Abdominal
Injection of Chromic Phosphate
( ) )
Supracolic
Total Omentectomy
Omental Pedicle "J"
Flap
Tube Gastrostomy
Total Vaginectomy
Radical
Vulvectomy
With Bilateral Inguinal
Lymph Node Dissection
Reconstruction
of the
Vulva With Gracilis Myocutaneous Flaps
Transverse
Rectus
Abdominis Myocutaneous
Flap and Vertical Rectus
Abdominis Myocutaneous
Flap
Radical
Wertheim
Hysterectomy With
Bilateral Pelvic Lymph
Node Dissection and With Extension of the Vagina
Anterior Exenteration
Posterior Exenteration
Total Pelvic
Exenteration
Colonic
"J" Pouch Rectal
Reservoir
Kock Pouch
Continent Urostomy
Omental "J" Flap
Neovagina
Ileocolic
Continent Urostomy (Miami Pouch)
Construction
of Neoanus
Gracilis Dynamic Anal
Myoplasty
Skin-Stretching
System Versus Skin Grafting
Gastric
Pelvic Flap for
Augmentation of Continent Urostomy or Neovagina
Control
of Hemorrhage in Gynecologic Surgery
Repair
of the Punctured
Vena Cava
Ligation
of a Lacerated
Internal Iliac Vein and
Suturing of a Lacerated Common Iliac Artery
Hemorrhage
Control in
Sacrospinous Ligament
Suspension of the Vagina
Presacral
Space
Hemorrhage Control
What
Not to Do in Case of Pelvic Hemorrhage
Packing
for Hemorrhage
Control
Control
of Hemorrhage
Associated With Abdominal Pregnancy |
Ileocolic Continent Urostomy
(Miami Pouch)
Continent urostomy of the ileal or ileocolic variety
(Miami pouch) has become an essential part of urinary diversion in
oncology patients. The mechanical engineering phenomenon of a pouch
that has pressure lower than the ureteral pressure entering it and
pressure lower than the efferent bowel limb leaving it, has the advantage
of having no urinary reflux. That, in turn, should reduce the incidence
of chronic subclinical pyelonephritis among these patients, and consequently,
reduce the loss of upper renal units. The continent efferent system
allows a better quality of life for a patient and avoids the social
disadvantages of a urinary ostomy bag.
Physiologic Changes. The
continent urostomy should be a low pressure pouch with pressures
in the range of 30 cm of water. At the same time, there should be
a nonrefluxing ureteral anastomosis into the pouch. If the normal
ureter has pressures of approximately 60 cm of water, there should
be little reflux from the pouch to the kidney. The combination of
these pressure differentials should allow the patient to be continent
and have little or no urinary reflux to the kidney.
Removal of a large portion of the right colon, a significant
portion of the transverse colon, and a portion of the terminal ileum
can cause various physiologic phenomena in the gastrointestinal tract.
Removal of the right colon and some of the transverse colon may produce
a watery diarrheal stool. Removal of the terminal ileum results in
problems with bowel salt metabolism, and absorption of fat-soluble
vitamins and vitamin B12. Loss of the ileocecal valve may involve reflux
of contaminated stool back into the proximal ileum, which, in turn,
can lead to problems with chronic small bowel infection and various
metabolite changes.
Points of Caution. The blood
supply to the Miami pouch is dependent on the ileocolic artery, particularly
the right colic branch of the ileocolic artery, and the middle colic
artery. These arteries connect with the marginal artery of the colon.
Extreme care must be exercised so that the ileocolic or middle colic
artery is not compromised. When performing the anastomosis, the surgeon
must be careful to place the ureter into the colonic pouch. The ureter
must prolapse 3 cm into the pouch to reduce urinary reflux. We have
changed the point of exteriorization of the efferent limb onto the
abdominal wall from the right lower quadrant to the umbilicus. This
gives a better cosmetic effect and also reduces incontinence of the
efferent bowel limb.
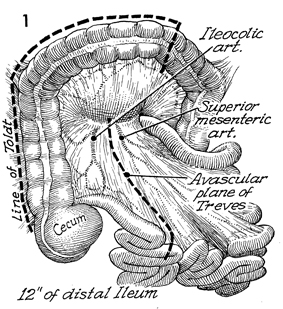
Technique
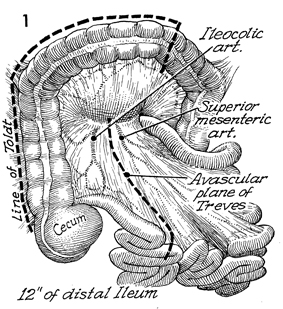
An outline of the colon and the small bowel
is shown with the key anatomical points: the ileocolic artery,
the superior mesenteric artery, the avascular plane of Treves
between the superior mesenteric artery and the ileocolic artery,
the terminal ileum, and the right and transverse colon. The line
of Toldt is outlined in the pericolic gutter (dotted line). The dotted
line shows the incisions to be made to create the pouch.
In these cases, the larger portion of transverse colon is used
to create a larger pouch. In radiated bowel, a large pouch will
have a lower pouch pressure because irradiated bowel lacks compliance
and, therefore, larger volumes of urine create excessive pouch
pressure. |
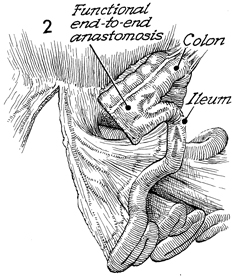
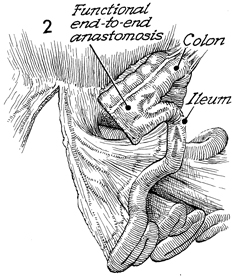
The midileum is anastomosed to the transverse
colon in a functional end-to-end anastomosis using the stapler. |
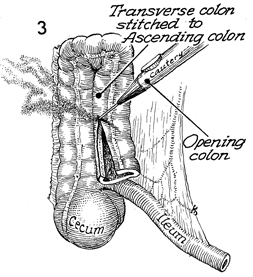
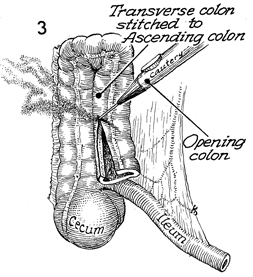
The transverse colon is brought along the
side of the right colon and sutured with several interrupted
3-0 synthetic absorbable sutures. The colon is then opened in
the midline with the cautery. |
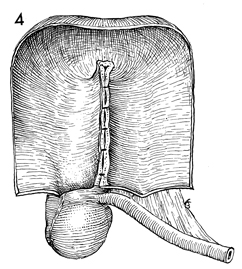
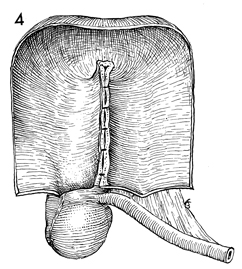
After opening the colon down
to the cecum, the surgeon sutures the posterior wall of the pouch
with interrupted 3-0 synthetic absorbable sutures. |
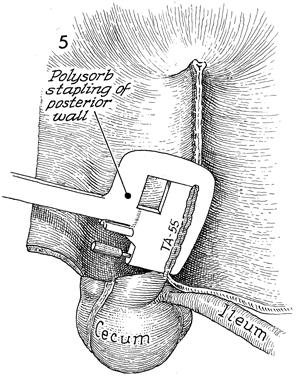
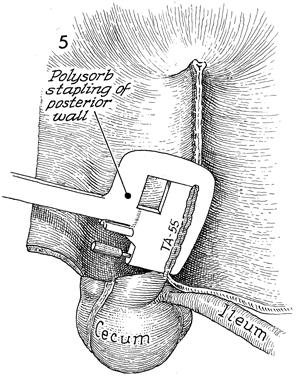
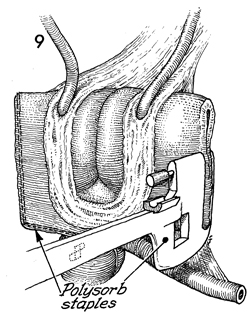
The posterior wall of the colon can be either
sutured or stapled. It is faster and easier to staple it with
a TA-55 Polysorb staple using multiple bites and suturing in
between each application of the stapler. |
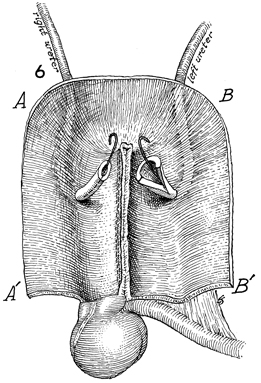
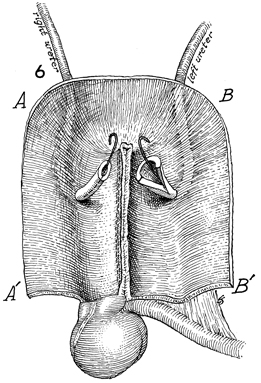
The right and left ureters
have been mobilized and are brought through the posterior wall
of the pouch via Leadbetter anastomotic technique. The ureters
must prolapse 3 cm inside the colon after being anastomosed to
allow protection from urinary reflux. Finney double-J Silastic
catheters are inserted up the ureters into the kidney and brought
out into the pouch. |
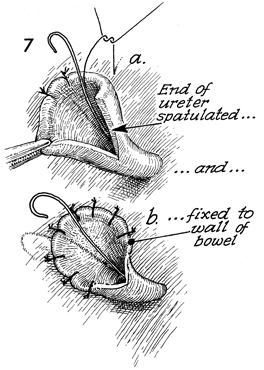
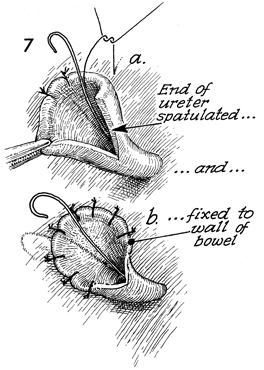
The Leadbetter anastomosis is demonstrated
by a mucosa-to-mucosa anastomosis after spatulating the ureter
to prevent iris contracture postoperatively. |
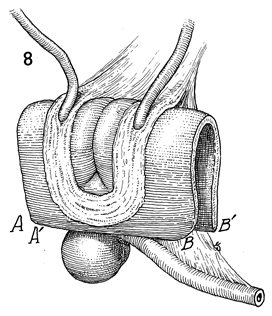
The pouch is folded over on
itself, point
A is brought alongside point A', and point
B is brought alongside point B'. The segment
of terminal ileum that will eventually become the efferent
bowel limb is shown. |
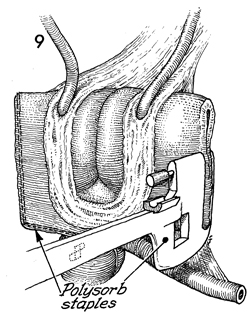
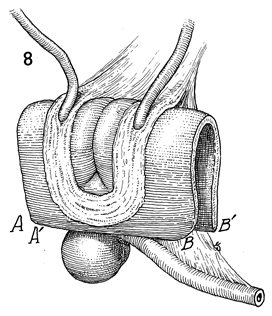
The ureters have been anastomosed to the
pouch. The TA-55 polysorb stapler is used to close the margins
of the pouch. |
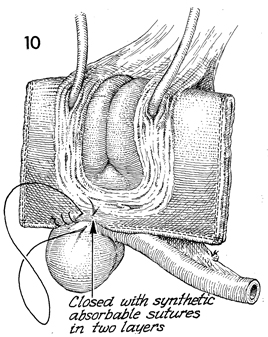
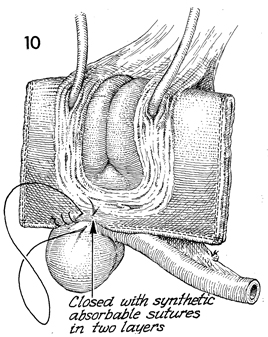
The ureters have been implanted. The margins
of the pouch have been stapled with a polysorb stapler. Small
areas that are awkward for the stapler to anastomose can be sutured
with 3-0 synthetic absorbable suture. |
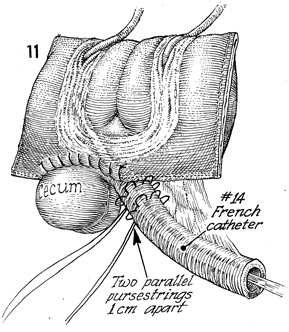
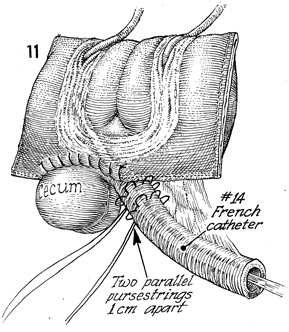
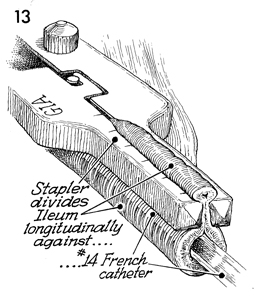
Attention is turned to the efferent bowel
limb. A No. 14 French catheter is inserted down the terminal
ileum into the pouch. Two parallel pursestring sutures 1 cm apart
are placed at the ileocecal junction with delayed synthetic absorbable
suture. |
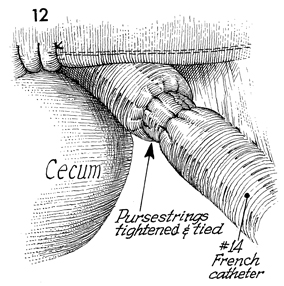
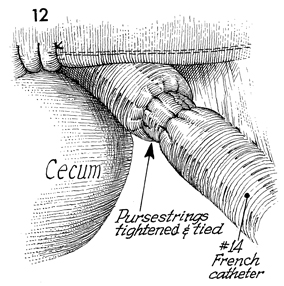
The pursestring sutures have been placed.
The No. 14 French catheter is seen traversing the efferent bowel
limb into the pouch. |
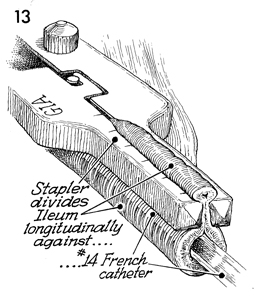
The GIA stapler with 4.8 staples is used
to taper the terminal ileum on its antimesenteric border to narrow
the lumen of the efferent bowel limb to the size of a No. 14
French catheter. This dramatically raises the pressure inside
the lumen, such that the pressure in the lumen of the efferent
bowel limb is more than twice the pressure in the pouch. |
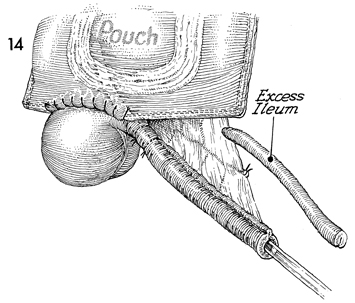
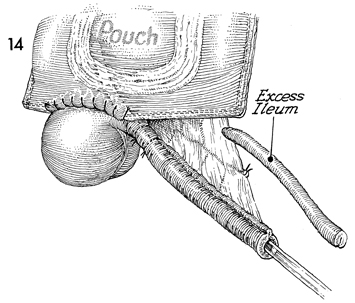
The efferent bowel limb has been tapered
with the stapler. Excessive ileum is discarded. |
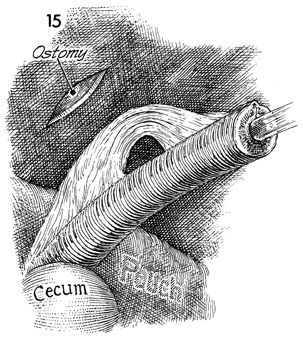
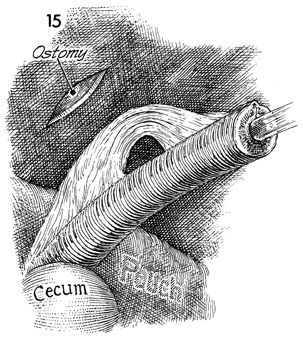
The inferior rim of the umbilicus is excised
enough to allow the efferent bowel limb to be pulled through
the abdominal wall at that site. |
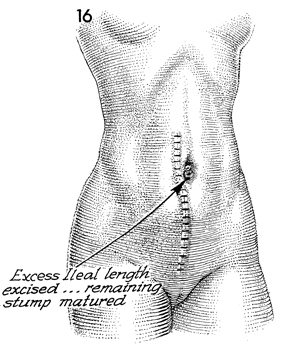
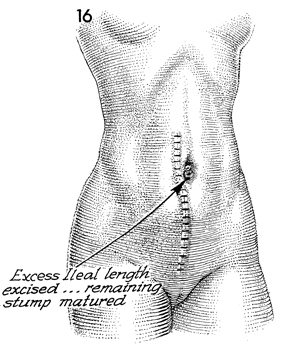
The efferent bowel limb has been brought
through the inferior rim of the umbilicus, and the excessive
ileal length has been excised. The remaining stump is sutured
with 3-0 synthetic absorbable suture. |
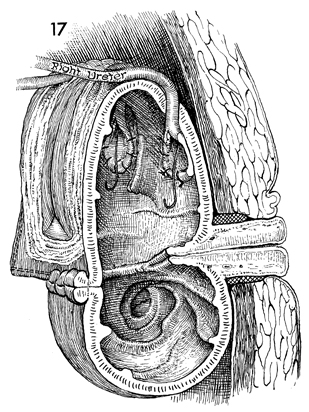
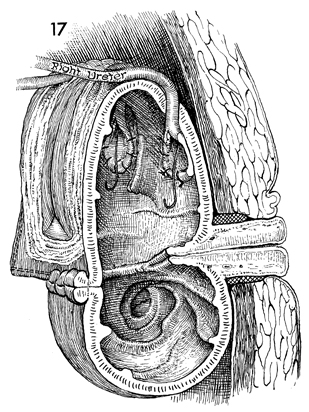
In this transverse view of the completed
Miami pouch, the ureters are implanted and prolapsed into the
pouch. Finney J Silastic stents are placed in the pouch, and
the efferent bowel limb has been sutured to the umbilicus. It
is best to leave an indwelling Medena catheter inserted through
the efferent bowel limb into the pouch for at least 2 weeks to
allow complete healing of all suture lines. The pouch should
be protected by a Jackson-Pratt closed suction cannula and irrigated
every four hours with 30 mL of warm saline. |
|
|