|
||||||
Malignant
Disease: Staging
of Gynecologic Application
of Vaginal Application
of Uterine Afterloading Applicators Abdominal
Injection of Chromic Phosphate Radical
Vulvectomy Reconstruction
of the Transverse
Rectus Colonic
"J" Pouch Rectal Ileocolic Continent Urostomy (Miami Pouch) Construction
of Neoanus Skin-Stretching
System Versus Skin Grafting Gastric
Pelvic Flap for Control
of Hemorrhage in Gynecologic Surgery Repair
of the Punctured Ligation
of a Lacerated Hemorrhage
Control in Presacral
Space What
Not to Do in Case of Pelvic Hemorrhage |
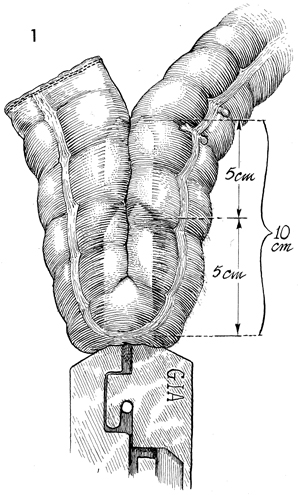
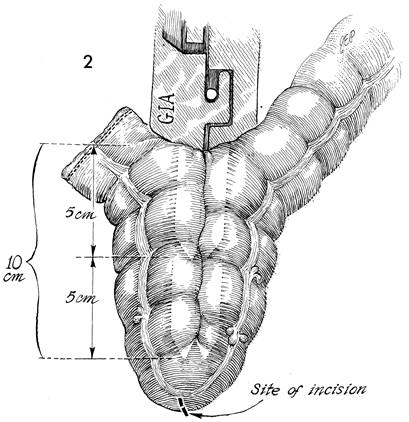
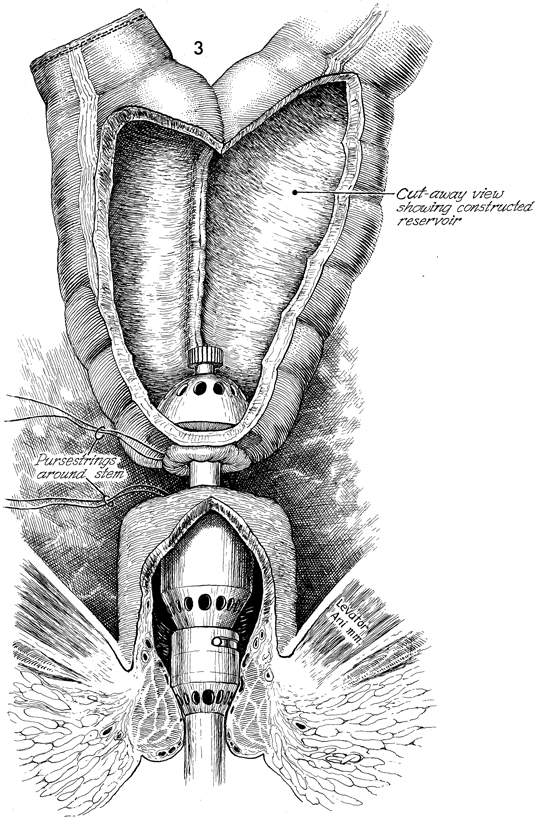
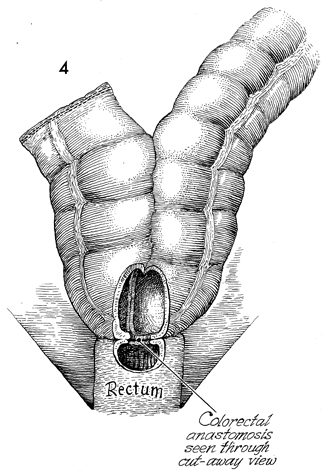
Colonic "J" Pouch Rectal Reservoir When the rectosigmoid colon must be removed in the treatment of genital cancer, an end sigmoid colostomy or a very low coloproctostomy may be performed. Very low anastomosis of the colon to the rectum may be associated with an unacceptable frequency of daily bowel movements. Although it is a social and esthetic relief to the patient to eliminate the colostomy stoma, having 6-8 bowel movements per day is an inconvenience and hardship. Treatment of the problem with opiates may produce addiction. The purpose of the "J" colonic pouch is to provide a rectal reservoir, thereby reducing the number of bowel movements and eliminating the need for drugs. Physiologic Changes. The "J" pouch rectal reservoir provides an increased storage area for feces. This may precipitate fluid absorption from the fecal stream and result in a firm but soft stool. The patient experiences a reduction in tenesmus. Points of Caution. Adequate mobilization of the transverse and descending colon must be performed to allow the end-to-side Strasbourg-Baker anastomosis to be performed without tension. Since many of the patients undergoing this procedure have had pelvic irradiation, it is important to keep the inferior mesenteric artery and its superior hemorrhoidal branch intact if possible. These arteries will supply blood to the anastomosis, thereby aiding the wound healing process and reducing suture line leaks and fistulae. Although it is possible to perform this procedure with a suture technique the use of surgical staplers reduces tissue trauma, allows precise placement of sutures, and significantly reduces operative time. If the patient has had pelvic irradiation or inflammatory bowel disease, a temporary diverting colostomy should be performed and kept in place until complete wound healing has been demonstrated. This is usually accomplished within 8 weeks. Technique
|
|||||
Copyright - all rights reserved / Clifford R. Wheeless,
Jr., M.D. and Marcella L. Roenneburg, M.D.
All contents of this web site are copywrite protected.