Malignant
Disease:
Special Procedures
Staging
of Gynecologic
Oncology Patients With
Exploratory Laparotomy
Subclavian Port-A-Cath
Peritoneal Port-A-Cath
Application
of Vaginal
Cylinders for Intracavitary
Radiation Therapy
Application
of Uterine Afterloading Applicators
for Intracavitary Radiation Therapy
Pelvic High-Dose
Afterloader
Abdominal
Injection of Chromic Phosphate
( ) )
Supracolic
Total Omentectomy
Omental Pedicle "J"
Flap
Tube Gastrostomy
Total Vaginectomy
Radical
Vulvectomy
With Bilateral Inguinal
Lymph Node Dissection
Reconstruction
of the
Vulva With Gracilis Myocutaneous Flaps
Transverse
Rectus
Abdominis Myocutaneous
Flap and Vertical Rectus
Abdominis Myocutaneous
Flap
Radical
Wertheim
Hysterectomy With
Bilateral Pelvic Lymph
Node Dissection and With Extension of the Vagina
Anterior Exenteration
Posterior Exenteration
Total Pelvic
Exenteration
Colonic
"J" Pouch Rectal
Reservoir
Kock Pouch
Continent Urostomy
Omental "J" Flap
Neovagina
Ileocolic
Continent Urostomy (Miami Pouch)
Construction
of Neoanus
Gracilis Dynamic Anal
Myoplasty
Skin-Stretching
System Versus Skin Grafting
Gastric
Pelvic Flap for
Augmentation of Continent Urostomy or Neovagina
Control
of Hemorrhage in Gynecologic Surgery
Repair
of the Punctured
Vena Cava
Ligation
of a Lacerated
Internal Iliac Vein and
Suturing of a Lacerated Common Iliac Artery
Hemorrhage
Control in
Sacrospinous Ligament
Suspension of the Vagina
Presacral
Space
Hemorrhage Control
What
Not to Do in Case of Pelvic Hemorrhage
Packing
for Hemorrhage
Control
Control
of Hemorrhage
Associated With Abdominal Pregnancy |
Peritoneal Port-A-Cath
Recent data indicate that some forms of intraperitoneal chemotherapy
for ovarian malignancies with small volume disease may be more efficacious
than intravenous chemotherapy.
Physiologic Changes. Intraperitoneal
chemotherapy allows a greater dose of drug to come into direct contact
with tumor cells and, at the same time, secondary to the large molecular
weight of the chemical, facilitates a delayed absorption across the
peritoneum into the vascular space. Therefore, a smaller dose of the
drug arrives at sensitive target organs, such as kidney, nerve, and
heart, per unit of time.
The length of time the cancer cells spend under
the curve of the ultimate dose of chemotherapy is important. After
an appropriate time under the "curve," the adjacent normal cells receive
no further damage from the drug because the chemotherapy can then be
withdrawn. Withdrawal reduces the time that the drug is administered
to the systemic circulation. This reduces the toxicity associated with
chemotherapy.
Points of Caution. A Port-A-Cath intraperitoneal
chemotherapy devices should not be inserted if there is bacterial contamination
of the peritoneal cavity.
The Port-A-Cath system should be flushed frequently
with heparinized saline solution. Ideally, it should be flushed once
a week to prevent clogging of the system with peritoneal fluid. It
should always be flushed thoroughly after any infusion of chemotherapy.
Technique
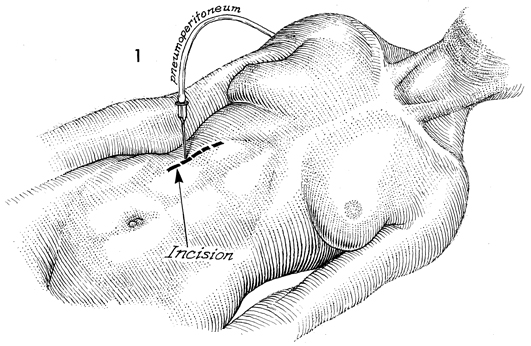
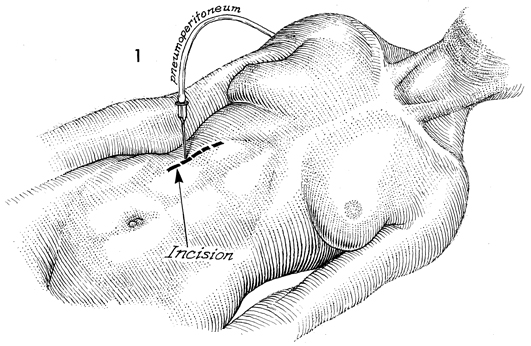
The patient is placed in the
supine position. The surgeon selects a site for the Port-A-Cath
by penetrating the abdominal wall with a 17-gauge Tuohy needle.
A saline syringe is attached to the needle, and assessment is
made for easy flow into the peritoneal cavity to ascertain when
the point of the needle is free in the peritoneal cavity and
when it is in an intraperitoneal organ or trapped between adhesions.
Another technique used to locate
a site for the Port-A-Cath is to attach the hub of the needle
to a pneumoperitoneum device, such as the laparoscopy carbon
dioxide gas machine. If the needle is free in the peritoneal
space, the flow pressure will be no higher than 10 mm Hg.
Several attempts are often required for placement of the needle several weeks
after radical cytoreductive surgery.
When the appropriate spot has
been located, a 6-cm "minilaparotomy" longitudinal incision is
made in that area. |
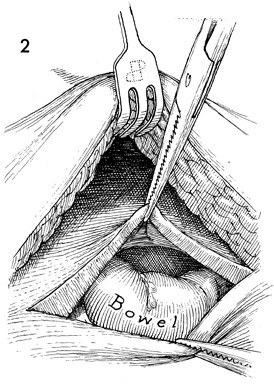
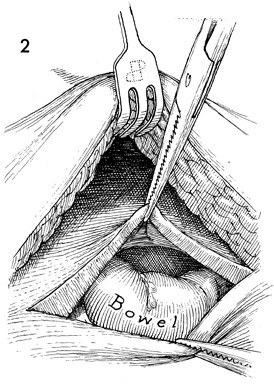
The incision is carried down
to the peritoneum, and the peritoneal cavity is entered. Dissection
of bowel and adhesions may be required to achieve complete
flow into the intraperitoneal space. |
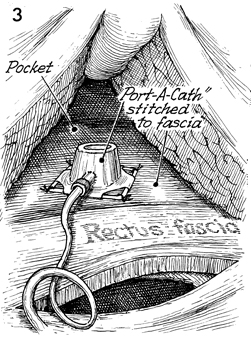
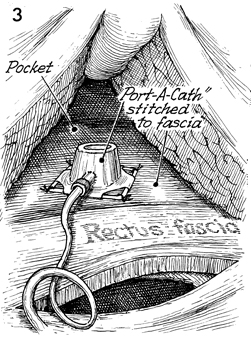
A subcutaneous pocket of 6-7
cm is created on top of the rectus fascia. The Port-A-Cath
is placed on top of the rectus fascia and secured with interrupted
3-0 nylon suture. At this point, the Port-A-Cath and its catheter
are filled with heparinized saline solution. |
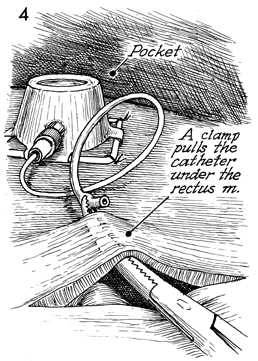
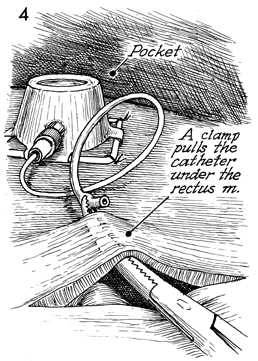
The incision in the rectus
fascia peritoneum remains open, and the catheter from the Port-A-Cath
is brought near that incision. A clamp is inserted through
the fascia and peritoneum, and a small cutdown is made onto
the tip of this clamp, approximately 3-4 cm lateral to the
fascia and the peritoneal incision. The catheter is brought
through this stab wound into the peritoneal cavity.
The Port-A-Cath catheter is
arranged in a manner that will allow it to traverse the entire
peritoneal cavity. The Port-A-Cath can be sutured to various
points in the peritoneal cavity to allow maximum distribution
of infused drug without creating the potential of a "clothesline"
effect of the catheter whereby a knuckle of bowel can become
involved in an internal hernia.
The incision in the peritoneum
and rectus fascias are closed in layers with delayed absorbable
sutures. |
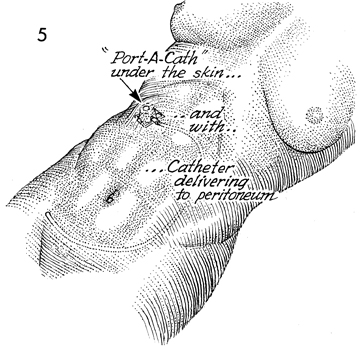
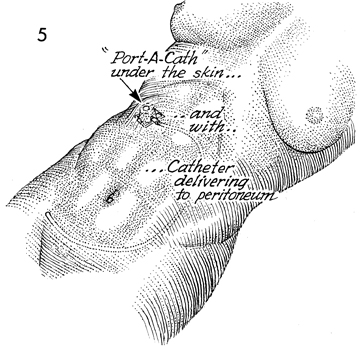
The Port-A-Cath is in its
pocket under the skin. The catheter travels through the peritoneal
cavity to deliver the drug to the pelvis and upper abdomen.
The surgeon can adjust the placement
of the catheter to meet individual needs. It can be placed adjacent
to the liver, diaphragm, or wherever the maximum tumor burden
lies.
The Port-A-Cath is flushed at the
end of the procedure with heparinized saline solution. |
|