|
||||||||
Malignant
Disease: Staging
of Gynecologic Application
of Vaginal Application
of Uterine Afterloading Applicators Abdominal
Injection of Chromic Phosphate Radical
Vulvectomy Reconstruction
of the Transverse
Rectus Colonic
"J" Pouch Rectal Ileocolic Continent Urostomy (Miami Pouch) Construction
of Neoanus Skin-Stretching
System Versus Skin Grafting Gastric
Pelvic Flap for Control
of Hemorrhage in Gynecologic Surgery Repair
of the Punctured Ligation
of a Lacerated Hemorrhage
Control in Presacral
Space What
Not to Do in Case of Pelvic Hemorrhage |
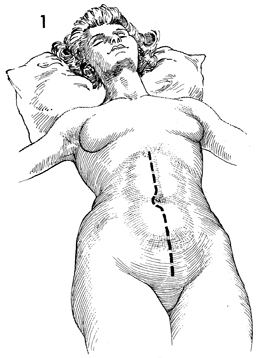
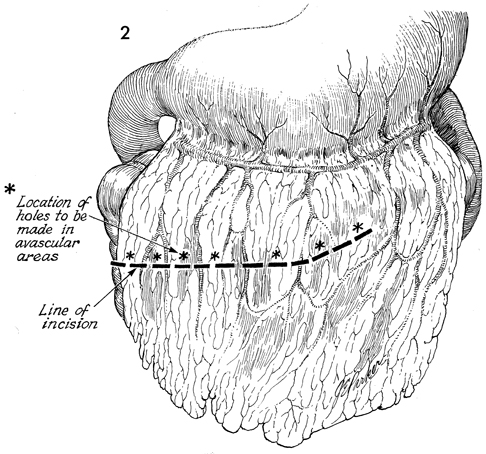
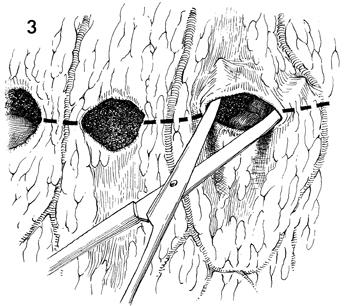
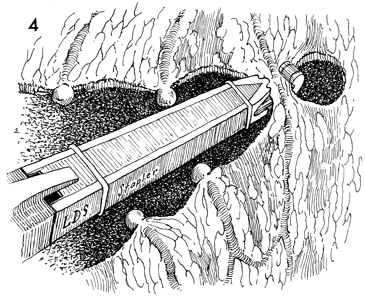
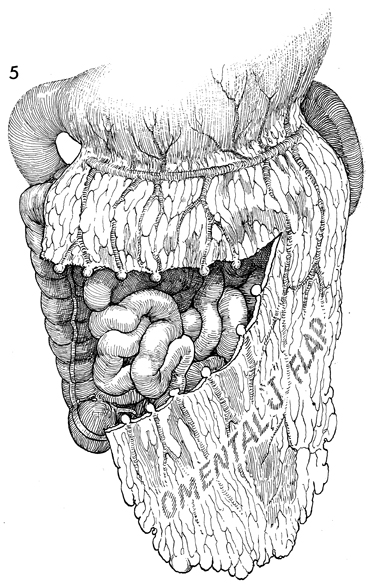
Omental Pedicle "J" Flap An omental "J" flap provides (1) a nonirradiated vascular pedicle flap to cover intestinal anastomoses and (2) vesicovaginal-rectovaginal fistula repairs to form a lid on the inlet of the true pelvis after exenteration and to form a cylinder for a neovagina. The purpose of this operation is to create a flap from the omentum by transecting the omentum from its attachments to the stomach, leaving enough branches of the left gastroepiploic vessels to provide an adequate blood supply for the flap. Physiologic Changes. Irradiation produces obliterative endarteritis, ischemia, and fibrosis, all of which retard healing. By applying a vascular pedicle that has not been irradiated, the surgeon attempts to reverse some of the ischemia present in the irradiated tissue by promoting capillary and arterial ingrowth from the pedicle flap's blood supply. In addition, when the inlet to the true pelvis has been blocked by an omental lid, the small bowel is prevented from dropping into the denuded true pelvis after an extensive operation. Therefore, the possibility of intestinal obstruction and fistula formation is reduced. The omentum has a copious blood supply. Therefore, it is an excellent recipient of a skin graft for a neovagina. Points of Caution. The short gastric vascular arcades to the omentum must be identified on the greater curvature of the stomach prior to initiating the procedure to ensure an adequate blood supply from the gastroepiploic artery remains for the proposed omental flap. The flap should be designed so the stomach is not pulled into the lower abdomen. The flap should not be placed on tension. Technique
|
|||||||
Copyright - all rights reserved / Clifford R. Wheeless,
Jr., M.D. and Marcella L. Roenneburg, M.D.
All contents of this web site are copywrite protected.